treatment of acute rejection
advertisement

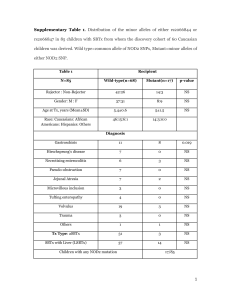
Created by: Emily Israeli, Vivian Fong, Sarah Mitchell, Jill Harrison, Ashley Schomer Three Main Types of Rejection Hyperacute rejection – caused by preexisting antibodies and activation of complement system – occurs immediately Acute Rejection – caused by mismatched HLA antigens – influx of T-Cells and cytokines – occurs 7-10 days out Chronic rejection – caused by proliferation of SMCs and excess collagen production that occludes the vasculature over time – occurs over long periods Healthy Islets surrounded by non-insulin producing pancreatic cells Islets suffering from hyperacute rejection Chronic rejection still remains a major problem up to 3 years out. At this point up to 40% of allografts have been rejected Basics of Molecular Mechanism of Rejection • Major histocompatibility complex (MHC) – locus on Chromosome 6 that encodes MHC molecules – polymorphic and codominant • Called human lymphocyte angtigen (HLA) molecules in humans • Mismatched HLA molecules present bound peptides • That MHC-peptide complex is presented by antigen presenting cells (APCs) to host T-cells • Two main methods of presentation: direct and indirect Indirect Presentation • Host APCs digest foreign MHCpeptide complexes • Then present the peptides from the digested complex on its own MHC molecules to T-cells • In this case the foreign MHC molecules are handled as if they were any other foreign antigen Direct Presentation • Donor APCs present donor MHC-peptide complexes • Host T-cells still recognize these complexes due to similarities • Most rejection mechanisms are elicited through direct presentation • Many different host T-cells can recognize a single foreign MHC molecule Indirect vs. Direct Presentation The direct and indirect pathways of antigen presentation. In the direct pathway, MHC molecules on donor APCs from the graft tissue present graft-derived peptides to host T-cells. In the indirect pathway, host APCs take up graft proteins and present donor-derived processed peptides on host MHC molecules to host T-cells. Immunosuppressive Agents "There are few examples of clinical procedures that have moved from complete failure to outstanding success in such a short space of time (Parrot)." Organ transplantation therapy is one of those examples. The human HLA antigen proved such a barrier to organ grafting, "that prior to the late 1950's, transplantation yielded uniformly dismal and consistently fatal results (Lysaght)." It was only through the discovery, evolution, and routing use of immunosuppressant agents that this barrier has finally been overcome. In fact, many organ transplantations are now routine clinical procedures - the kidney transplant is a prime example, with 15,122 procedures performed in 2003. Organ transplantation therapy is highly dependent on the success of pharmacotherapy to suppress recipient immune responses to the foreign organ; allograft rejection remains as the major barrier to long-term graft survival in patients. In fact, transplant patients require lifelong immunosuppressive drug therapy to prevent this rejection. Clinical Science currently has a comprehensive understanding of the cellular mechanisms behind graft rejection. Rejection follows a certain path with steps that include graft recognition, cytokine signaling, lymphocyte proliferation, and attack. Different immunosuppressive agents work by blocking this path at various steps. Corticosteroid Prednisone (Deltasone®), Methylprednisolone (SoluMedrol®) s Corticosteriods are used in maintenance immunosuppression, and the treatment of acute rejection. A corticosteroid is a medication that works principally to block T cell and APC derived cytokine and cytokine-receptor expression. The major elements blocked are IL-1, IL-6, IL-2, INF-γ , and TNF-α . These elements, notably IL-1, are essential for lymphocyte-APC communication. A decrease in production effectively obstructs an APC's capacity to activate allograft-specific lymphocytes. As a result, threat of acute rejection is reduced. Corticosteroids have a hydrophobic structure that allows them to easily diffuse into cells and bind to specific cytoplasmic receptors. The resulting complexes progress to the nucleus, where they are able to inhibit the transcription of the genes of the cytokines named above. Corticosteroids are also able to inhibit cytokine production in macrophages. This subsequently inhibits the macrophage phagocytosis and chemotaxis properties. Corticosteroids are also potent non-specific antiinflammatory agents - administration results in an acute reduction of circulating lymphocytes and monocytes. Calcineurine Inhibitors Cyclosporine (Sandimmune®, Neoral®, Gengraf®), Tacrolimus (Prograf®, FK506) Calcineurine Inhibitors are used in maintenance immunosuppression. The mechanisms of Calcineurine Inhibitors converge at the inhibition of the calcineurin. This inhibition ultimately inhibits the production and secretion of IL-2. The interaction between IL-2 and the IL-2 Receptor is crucial in the activation, differentiation, and proliferation of B and T cells. Therefore, halting the rejection process at this step is highly effective at combating rejection. Cyclosporine is a small fungal cyclic peptide. Cyclosporine works by binding a protein found in the cytosol: cyclophilin. This complex inhibits calcineurin. The rest of the mechanism is outlined above. Cyclosporine is a highly effective immunsuppressant. In fact, cyclosporine is generally hailed as the cornerstone of immunosuppression. The clinical introduction of Cyclosporine significantly increased graft survival and significantly reduced the occurrence of acute rejection in patients. Tacrolimus is a microlide antibiotic that works in a mechanism similar to that of cyclosporine. Tacrolimus binds the cytosolic protein FKPB-121. This complex inhibits calcineurin in a manner parallel to cyclosporine. Antiproliferative Agents Mycophenolate Mofetil (CellCept®), Azathioprine (Imuran®) Sirolimus (Rapamune®) Antiproliferative Agents are used in maintenance immunosuppression and treatment of rejection. Antiproliferative Agents are drugs that work to block the proliferative phase of acute cellular rejection. They are an integral part of most immunosuppression regimens. Mycophenolate Mofetil Mycophenolate Mofetil (MMF) is absorbed and rapidly hydrolyzed in the blood to its active form: MPA. MPA inhibits the key enzyme in the de novo pathway of purine biosynthesis, IMPDH. Rapidly dividing cells, such as activated lymphocytes, depend on the de novo pathway for the production of purines necessary for RNA and DNA synthesis. In this way, activated lymphocytes are selectively inhibited since they are not allowed to proliferate once activated. Antiproliferative Agents Azathioprine Azathioprine is rapidly hydrolyzed in the blood to 6-mercaptopurine. In this form (a purine analog and antimetabolite), it incorporates into the DNA, inhibiting nucleotide synthesis by causing feedback inhibition in the early stages of purine metabolism. This ultimately prevents mitosis and proliferation of rapidly dividing cells, such as activated B and T lymphocytes. Through this action, Azathioprine is able to block most Tcell functions and inhibit primary antibody synthesis. Azathioprine has little effect on established immune responses, and is therefore effective only in the prevention (not treatment) of acute rejection. Sirolimus Sirolimus is a highly potent macrolide antibiotic that has a chemical structure similar to Tacrolimus. Sirolimus binds to the same protein as Tacrolimus: FKBP-12. Instead of inhibiting Calcineurin as Tacrolimus does, this complex inhibits mTOR. This inhibition prevents the progression of T cells from the G1 to the S phase of the cell cycle by blocking signaling downstream of the IL-2 receptor. It therefore is able to block DTH immune reactions, CTL activity, and humoral responses directed against a transplanted organ. Because Cyclosporine and Sirolimus have different mechanisms, the combination of clinical combination of the two in an immunosuppression regimen results in effects that are synergistic. Monoclonal Antibodies Muromonab-CD3 (Orthoclone OKT3®), Daclizumab (Zenapax®) Interleukin-2 Receptor Antagonist (Basiliximab, Simulect®) Monoclonal Antibodies are used in early rejection prophylaxis and treatment of rejection. Monoclonal antibodies are antigen-specific immunosuppressants that will reduce immune response to alloantigens of the graft while preserving the response to alloantigens to unrelated antigens. These agents are specific to blocking T-cell activation, resulting in rapid depletion of T cells from the circulation by binding of antibody coated T cells to Fc receptors on phagocytic cells. The most recently FDA approved monoclonal antibodies are the IL-2 receptor antagonists genetically engineered to possess both human and murine antibody sequences. The chimerization of these antibodies is an attempt to decrease the immunogenicity of the agent. Other monoclonal antibody-based drugs are still in clinical trials for FDA approval. Monoclonal Antibodies Muromonab – CD3 Muromonab-CD3 is the first type of murine monoclonal antibody directed against the ε chain of the CD3 molecule (an integral part of the T Cell Receptor complex) and modulates the receptor and inactivates T-cell function blocking both naïve T cells and CTLs. This results in rapid depletion of T cells from circulation and cytokine release. This antibody is used to treat acute rejection and steroid resistant rejection. Baxiliximab Basiliximab is a chimeric (70% human and 30% murine) monoclonal antibody utilized in the prevention of acute organ rejection. This monoclonal antibody has a specificity and high affinity for the α subunit of the interleukin (IL)-2 receptor (IL-2Rα, also known as CD25 or Tac) preventing IL-2 from binding to the receptor on the surface of activated T cells. By acting as an IL-2Ra antagonist, Basiliximab inhibits IL-2mediated activation and proliferation of T cells, the critical step in the cascade of cellular immune response of allograft rejection. Therefore, Basiliximab has a long half-life of approximately 7-12 days and saturates the IL-2 receptor for up to 59 days. Due to its high percentage of humanization in its antibody sequences the occurrence and acuteness of adverse effects is significantly lower when used with standard immunotherapy. Monoclonal Antibodies Muromonab – CD3 Daclizumab is a similar agent to Basiliximab, but is a more humanized IgG monoclonal antibody (90% human and 10% murine). It also binds to and inhibits the α-subunit of IL-2 receptor and thus works in a manner similar to Basiliximab. Daclizumab is able to saturate the IL-2 receptor twice as long as Basiliximab. Because it is more humanized, there are less side effects associated with Daclizumab. Side Effects - HAMA One of the major problems affecting monoclonal therapy is the side effects associated with the HAMA (Human anti-Murine Antibody) response and serum sickness. These are both directly caused by the structure of the antibodies. Laboratories routinely use murine antibodies as a starting point for monoclonal antibodies. This poses a problem: human immune system is able to identify the murine antibody as non-self and eliminate the treatment from circulation. This renders the monoclonal therapy ineffective. A counteractive measure includes humanizing (or chimerizing) the antibody. Because the only immunologically offensive portion of the antibody is the constant region, recombinant techniques can be used to splice and replace the constant region of the murine antibody with that of a characteristic human antibody. Current drugs have been developed that are more favorably humanized. They are also shown to be more effective with less adverse side effects. Further chimerization and other improvements in antibody therapy are active fronts of current research. Polyclonal Antibodies Antithymocyte globulin-equine (Atgam®) Antithymocyte globulin-rabbit (RATG, Thymoglobulin®) Polyclonal Antibodies are used in early rejection prophylaxis, treatment of rejection. Polyclonal antibodies are directed against lymphocyte antigens; instead of the single-specificity of the monoclonal antibodies, these anitlymphocyte antibodies are directed against multiple epitopes. Antithymocyte globulin is a polyclonal antibody derived from either horses (Atgam®) or rabbits (Thymoglobulin®). The agents contain antibodies specific for many common T cell surface antigens including CD2, CD3, CD4, CD8, CD11a, CD18. The antithymocyte globulin binds lymphocytes that display the surface antigens previously listed. This effectively depletes T-cell concentration in the body through complementdependent cytolysis and cell mediated opsonization following with T cell clearance from the circulation by the reticuloendothelial system (RES). Despite the glamorous advances of immunosuppressants, it is important to bear in mind the mechanism behind immunosuppression: Immunosuppressants dampen the body's immune system. With current therapy, there are adverse side-effects that include, among others, a high incidence of opportunistic infection and transplant-related malignancies in patients. These are the unfortunate consequences of overimmunosuppression. Accordingly, a major goal of immunosuppression is to identify the optimal balance of therapy such that there is effective prevention of allograft rejection, while drug-related adverse effects, infection, and malignancies are minimized. Because this compromise is largely unsatisfactory, there is a constant search for more effective and specific immunosuppressive agents and strategies. Side Effects Associated with Immunosuppressants: alopecia - loss of hair, baldness hypertricosis - excessive hair growth anemia - a pathological deficiency in the oxygen carrying compound of the blood hypertriglyceridemia - a disorder due to disturbances in synthesis and/or degradation of triglycerides-rich plasma lipoprotiens arthralgias - pain experienced in the joints hyperuricemia - the presence of excess uric acid in the blood bone marrow depletion - a depletion of bone marrow (a soft, fatty, vascular tissue that fills most bone cavities - it is the source of blood cells) hypomagnesemia - a deficiency of magnesium in the blood coronary artery disease - a stage of arteriosclerosis involving fatty deposits inside the artery walls that feed the heart cushingoid appearance - moon face, buffalo hump, centripetal obesity gastrointestinal upsets - discomfort spurring from the stomach and/or intestines gingival hyperplasia - an increase in the amount of gum tissue in the mouth glaucoma - eye diseases characterized by high intraocular fluid pressure, damaged optic disk, hardening of the eyeball, and loss of vision hepatoxicity - damage to the liver hirsutism - excess facial and body hair hypercholesterolemia - the presence of excess cholesterol in blood hyperglycemia - the presence of excess sugar in the blood leucopenia - a decrease in the total number of white blood cells in circulating blood malignancy - presence of a tumor (cancer) nausea - extreme disgust with an urge to vomit nephrotoxicity - damage or poisoning to the kidneys neoplasia - the formation of tumors opportunistic infection - any infection caused by a microorganism that does not normally cause disease in humans osteoporosis - a condition characterized by decrease in bone mass and bone density pancreatitis - inflammation of the pancreas pruritis - a sensation of itchiness on the skin hyperkalemia - a condition where potassium levels are too high in the body thrombocytopenia - decrease in the number of blood platelets that is often associated with hemorrhage conditions hyperlipidemia - the presence of excess fat or lipids in the blood tremor - trembling or shaking, usually from physical weakness and disease hypertension - abnormally high blood pressure - especially arterial blood pressure ulcer formation - development of a break in the skin or mucous membrane with loss of surface tissue Drug Efficacy Immunosuppression Usage by Organ in 2001 and 2002 Drug Efficacy Tacrolimus vs. Cyclosporine Polyclonal vs. Monoclonal Results from a randomized control trial of a Monoclonal Antibody (against the IL-2R) as compared with RATG for prophylaxis against rejection against renal allographs (New England Journal of Medicine) Inductive Therapy Inductive therapy refers to the prophylactic application of perioperative antibodies in addition to baseline immunosuppression. The goal of the employment of these drugs is to induce hyporesponsiveness in the organ recipient toward the transplanted organ in order to prevent early post-transplant rejection. Ideally, only T cells that respond to the donor antigen are inhibited and the rest of the patient's immune system would remain fully functional. Unfortunately, modern medication is not yet so specific, and so the general inhibition of the immune system causes the patient to be more susceptible to infection. The drugs must be strong enough to prevent rejection while protecting the patient from infection at the same time. This balance is complicated by the various interactions of multi-drug therapy; reactions can often be synergistic or lead to the up/down-regulation of drug metabolism. Initial efforts at inductive therapy utilized polyclonal antibodies, which are nonspecific and can cause allergic reactions, release of pro-inflammatory cytokines, neutropenia, and hemolysis. Today, however, murine monoclonal anti-lymphocyte antibodies, such as OKT3, are often used. To combat the side effects and generally increased risk of infection (caused by relatively nonspecific suppression of the immune system), antimicrobial agents are a necessary component of inductive therapy. Maintenance Therapy Maintenance immunosuppression refers to the classic combination therapy (known clinically as Triple Therapy) to which transplant recipients usually adhere for the rest of their lives. The combination includes: a corticosteroid a calcineurine inhibitor an antiproliferative The concurrent administration of these three drugs have distinct combined effects on each individual. The balance of dosages can be altered to enhance the efficacy of the immunosuppression for each patient. As with inductive therapy, the goal of maintenance immunotherapy is to balance between underimmunosuppression (which result in graft rejection) and overimmunosuppression (which expose the patient to high risks of infection and other potentially fatal side effects). The various side effects of each drug must be considered, as well as potential interactions between drugs, especially those that cumulatively present significant risk factors to certain patients. Thus, although the regimen of triple therapy is conventionally standardized, there is much room to improve immunosuppressive therapy to maximize efficacy and safety for the thousands of patients permanently on this treatment. Functional Tolerance The reduction of dosages in maintenance immunotherapy without graft rejection consequences is a phenomenon that has been observed by many researchers (as well as many patients who routinely disregard their doctors' prescriptions). Most notably, Dr. Tom Starzl has studied the induction of functional tolerance in transplant patients on maintenance immunotherapy. By mechanisms not entirely understood, over time some patients require less immunosuppression in order to prevent graft rejection. The medical benefits to such a reduction of therapy, as well as the cost benefits for those spending as much as $25,000 per year on immunosuppression, are outstanding. Functional tolerance is certainly a focus for future research and a realistic goal for maintenance immunotherapy treatment. Dr. Tom Starzl presented some of his findings on functional tolerance at the 19th International Congress of the Transplantation Society. A Tolerance Video available on the group webpage features his insightful explanations of his recent studies. Episodic Treatment Immunotherapy is truly a treatment that delays the inevitability of graft rejection. However, when an acute rejection episode does finally occur, transplant patients still have good therapy options. Rejection Episodes can be treated by the one of the following treatments: Corticosteroid Polyclonal and Monoclonal Antibodies Antiproliferatives Current Areas of Research Despite enhancements in immunosuppressant pharmacological therapies, doctors still struggle to balance the adverse reactions of overimmunosuppression and organ rejection from underimmunosuppression. Additionally, organ transplantation is severely limited by availability of donor organs; 75% on the organ waiting list who are in desperate need of an allograft die empty-handed. The individuals lucky enough to receive donor organs are resigned to a life of immunosuppressant therapy and its long list of associated side effects. Overall, there is an apparent problem with the current methods of immunosuppression. There are two main potential answers to this dilemma. Either immunosuppressant drugs need to become more specific and effective in dealing with transplant rejection and side effects must be significantly diminished, or immunosuppressant therapy needs to step away from drug use as a whole with alternative therapies stepping in. Both approaches represent the forefront of medical research. New drugs are being developed that are increasingly specific and effective in combating transplant rejection. Drug Efficacy is also discussed. These topics are supplemented by research into alternate means of immunosuppression through tissue engineering, stem cell research, and induction of tolerance. Xenotransplantation is also being worked out as a possible alternative to allogenic transplantation. As stated earlier, an important current area of research includes improving current drugs, and developing concepts for new approaches for pharmacotherapy. There are many aspects of current drug immunosuppressant therapy that can be improved. A first point of concern is the many side affects associated with current medications. Drugs can also be improve in effectiveness, as most transplants ultimately fail. This section highlights some of the drugs being researched, but is in no way meant to represent a complete list of new drugs. Drugs Under Development Include: Basiliximab (Simulect) Anti-CD20 CP-690,550 Antibodies Targeting Costimulatory Proteins Alternative Therapies Xenotransplantation Tissue Engineering Stem Cell Research Induction of Tolerance Tolerance refers to a state where adverse immune response to transplant antigens is eliminated while the rest of the immune system remains intact. Tolerance can be achieved through lymphocyte anergy. Anergy is a situation in which the lymphocytes specific for transplant antigens are unable to respond effectively or potential transplant-specific lymphocytes are deleted before having a chance to mature and circulate. Tolerance can be achieved in the following methods suppression of appropriate APC derived co-stimulatory signals and obstruction of pathways through which rejection occurs clonal deletion of cells reactive to the foreign graft - irradiating the thymus and administering anti-CD4 and anti-CD8, theoretically collapse the immune system suppressor T cell (or Ts cell)

![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)