Nancy Strassel, Senior Vice President, Greater Cincinnati Health
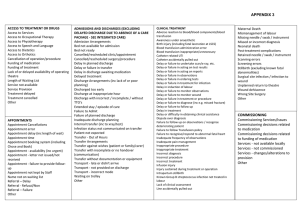
advertisement

Transforming Healthcare Nancy M. Strassel Senior Vice President Greater Cincinnati Health Council Where Are the Connections? • 270,000 discharges • 1 in 5 patients readmitted • We can do better P Laser Focus • • • • 18 hospital learning collaborative Reduce heart failure readmissions Improve transitions of care Know who our patients are – equity in care These 5 areas are targeted for high risk CHF patients in support of the ACT Hospitals. Readmission Reduction and Care Transitions Standards (T5) 1) 2) 3) 4) 5) Upon admission implement a risk assessment tool with a focus on Heart Failure to identify patients who are at high risk of readmission considering social factors Include a comprehensive assessment of the post hospital needs Use the teach-back method during the hospital stay from admission to discharge during key clinical interventions. Provide real-time handover communications (IHI, 2011) Provide patient and primary care givers a patient-friendly post-hospital care plan which includes a clear medication list Provide customized, real-time critical information to the next clinical care provider(s) For high risk patients, have a clinician call the individual(s) listed as the patient’s emergency contact to discuss the patient’s status and plan of care as applicable Address timely physician follow-up (appt to occur within 5-7 days of discharge) Either schedule follow up physician appointment for the patient, provide scheduling info to the patient or sit with the patient while they make the appointment prior to discharge – appointment should be tailored to the care giver’s schedule (include primary care specialist and therapy appointments if possible) Follow up with the patient or primary care giver (or emergency contact) within 48-72 hours of discharge via telephone or home visit. Adopted by the ACT Leadership on 10/12/11 from a variety of sources including Project BOOST, STAAR and IHI. Chart Reviews and Patient Interviews • 36% had a follow-up appointment scheduled prior to discharge (6/7/12 sample) • 52% did not call a health professional for guidance before being readmitted (10/18/12 sample) • 39% made and/or kept appointment within 7 days (4/11/13 sample) Care Transitions – New Approaches P • 5 hospitals, Health Council, COA • Christ, Mercy FF, Jewish, University, Clinton • Patient coaching and empowerment model • Two-year contract with CMS • RESULTS: Baseline of 25% to a current readmission rate of 15.2% (coached patients) Equity in Care • Standardized categories and methodology for the collection of patient race, ethnicity and language data • Data integrity standards • Spread to primary care practices • 56% collecting all three fields (REL) to 100% • LEP improvement project underway P9 What Did We Learn? One model doesn’t fit all Focus on entire continuum of care This is not linear work IT has to integrate into the work processes Leadership and grassroots group needed to drive change Power of patient interviews; test staff perceptions Measure! Pull in physicians to be part of the dialogue Build on common ground with post-acute providers Data delays can be a challenge Questions Thank You………. www.gchc.org Nancy Strassel, SVP nstrassel@gchc.org