Ab-Resist_07ho
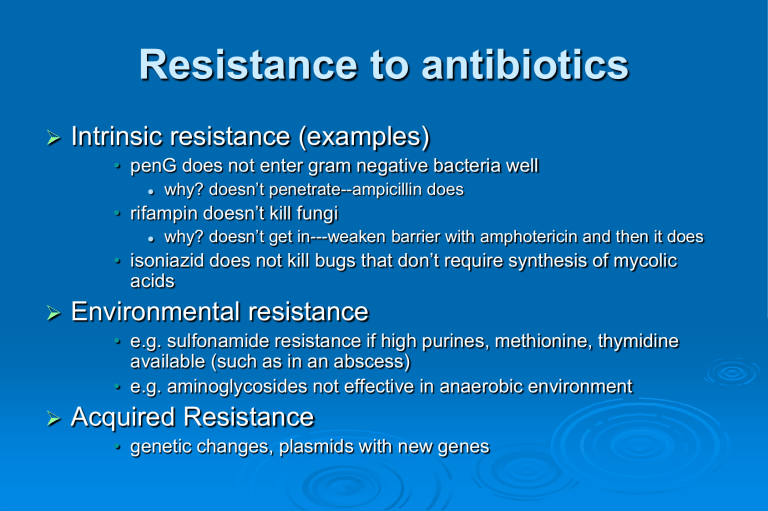
Resistance to antibiotics
Intrinsic resistance (examples)
• penG does not enter gram negative bacteria well
why? doesn’t penetrate--ampicillin does
• rifampin doesn’t kill fungi
why? doesn’t get in---weaken barrier with amphotericin and then it does
• isoniazid does not kill bugs that don’t require synthesis of mycolic acids
Environmental resistance
• e.g. sulfonamide resistance if high purines, methionine, thymidine available (such as in an abscess)
• e.g. aminoglycosides not effective in anaerobic environment
Acquired Resistance
• genetic changes, plasmids with new genes
2006 Antibiogram Harborview/UW
Acquired Drug Resistance
1. enzymatic inactivation ( b
-lactams, aminoglyc. chloramph)
Bacteria keep up with big pharma in the b -lactam antibiotic arms race bacteria can often express more than one b -lactamase
Inactivation of aminoglycosides by acetylation, phosphorylation, and adenylation in drugresistant organisms
Acquired Drug Resistance
1. enzymatic inactivation ( b
-lactams, aminoglyc. chloramph)
2. rapid efflux of drug out of cell (tetracyclines, ciprofloxacin)
Drug export systems in Gram +
Acquired Drug Resistance
1. enzymatic inactivation ( b
-lactams, aminoglyc. chloramph)
2. rapid efflux of drug out of cell (tetracyclines, ciprofloxacin)
3. decreased conversion to active form (isoniazid)
4. increased concentration of antagonist/competitor (sulfonamide resistance with increased PABA synthesis).
5. altered amount of receptor (trimethoprim-DHFR amplification)
6. altered structure of target to reduce binding (methicillin resistance, vancomycin resistance, ciprofloxacin res.)
Vancomycin resistance: mechanism
Vancomycin resistance: mechanism
Resistance can be transferred between bacteria
phage transduction
transposable elements
plasmid transfer during conjugation
• plasmids can contain multiple resistance genes
• transfer can occur between non-pathogen and pathogens
Plasmid-mediated drug resistance tetracycline sulfonamide chloramphenicol aminoglycoside
Problems with Antibiotic resistance
more than 50% of antibiotics used in domestic animals for subtherapeutic effect: breeding ground for resistance
There are 7.5 billion chickens, 292 million turkeys, 109 million cattle and 92 million pigs in the United States.
Antibiotics given to pigs as of 2000
“KFC does not purchase poultry treated nontherapeutically with medically important antibiotics.” – Letter to “Keep Antibiotics
Working,” August 28, 2002
McDonald’s
‘We’ve listened to the concerns, studied the issue, and the bottom line was we thought it was the right thing to do to discontinue the use of
[fluoroquinolone antibiotics] in poultry,’ said Walt
Riker, spokesman for Oak Brook-based
McDonald’s. – Walt Riker, McDonald’s,
“Chickens Fed With Antibiotics McGone,”
Chicago Sun-Times, February 12, 2002
Prospects for new antibiotics?
new antibiotic development slowed in 80’s/90’s
selective drugs have lower market value
5-15 yr time frame to get new drugs to physicians
recent increase in new antibiotic development is encouraging
active against Strep pneumoniae
Plasmid Mediated Quinolone
Resistance (PMQR)
First reported in a strain of K. pneumoniae
QnrA protein – 218 aa protein
Protects DNA gyrase and topoisomerase IV from the inhibitory activity of quinolones--exact mechanism is not known yet
Qnr proteins
QnrA2 – K. oxytoca (China)
QnrB - E. coli, K. pneumoniae, E. cloacae, C. koseri (USA and India) - 40% aa identity with QnrA
QnrS – S. flexneri (Japan) - 59% aa identity with QnrA
The presence of other mechanisms of resistance may increase plasmid-mediated quinolone resistance
PREVALENCE OF PLASMID-MEDIATED RESISTANCE TO
QUINOLONES IN Escherichia coli
1% QnrA+ isolates among ciprofloxacin-resistant E.coli from different countries [AAC (2003) 47:559]
11% QnrA+ isolates among ciprofloxacin-resistant K. pneumoniae and 0% in E.coli from USA [AAC (2004)
48: 1295]
7.7% QnrA+ isolates among ciprofloxacin-resistant E. coli in Shanghai (China) [AAC (2003) 47: 2242]
0.4% QnrA+ isolates among nalidixic acid- resistant
Escherichia coli (France) [AAC (2005) 49: 3091]
TB drug development
no new TB drugs in past 40 years
multi-drug resistant
TB prevalent
Johnson & Johnson
R207910
targets mycobacterium ATP synthetase
b
-Lactam Antibiotic development
spectrum of action
resistance to b
-lactamase specific b
-lactamase inhibitors
Ampicillin
Penicillin G
Amoxicillin
Methicillin
Dicloxacillin
R
Group
Natural penicillins
Pen G/Pen V b
-lactam antibiotics-1
Spectrum b
-lactamase sensitivity narrow spectrum gram positive sensitive
Penicillinase resistant
-methicillin
-dicloxacillin narrow spectrum resistant
Methicillin resistance
caused by unique peptidyl transferase that does not bind b
-lactams had been largely confined to hospital acquired infections more recently--outbreaks in athletic teams, iv drug users, school children, gay community, general population
900 cases in LA county jails
(2002)
Structure of PBP2a
Group b
-lactam antibiotics-1
Natural penicillins
Pen G/Pen V
Spectrum narrow spectrum gram positive b -lactamase sensitivity sensitive
Penicillinase resistant methicillin dicloxacillin
Aminopenicillins ampicillin amoxicillin
Antipseudomonal ticarcillin piperacillin narrow spectrum gram negative gram negative including pseudomonas resistant sensitive sensitive
Cephalosporins
Brody’s Human Pharmacology
Group
Cephalosporins cefaclor ceftriaxone b
-lactam antibiotics-2
Spectrum broad spectrum b -lactamase sensitivity variable
Newer
b
-lactams
aztreonam (monobactam)
gram specific resistant to b
-lactamase
Carbapenems: imipenem, meropenem
broad spectrum
(gram + ,gram ) resistant to b
-lactamase penetrates CSF
imipenem a substrate for dehydropeptidase I in kidney, meropenem is not
Brenner
b
-lactamase inhibitors
b
-lactamase inhibitors
Clavulanic acid (suicide inhibitor for most lactamases)
• little antibiotic action on its own
• combine with amoxicillin to get Augmentin (oral activity)
• combine with ticarcillin to get Timentin
Sulbactam (similar inhibitor)
• combine with ampicillin to get Unasyn (given iv or im)
Activity of available b -lactamase inhibitors against clinically important b -lactamases