01 Rocky Mtn - ACP S MacLeod final 24Nov12

High Cost Treatments / Limited Resources
Seeking a Balance
Rocky Mountain/ACP/AMA Internal Medicine Meeting
Banff, Alberta – November 24, 2012
Stuart MacLeod, MD, PhD, FRCPC
Professor, Pediatrics, University of British Columbia
Child & Family Research Institute, Vancouver
Disclosure
• Until August 2012 SMM was vice president research coordination and academic liaison for BC Provincial Health Services Authority.
• SMM has served as a consultant to Health Canada,
European Community FP-7, Canadian Agency for Drugs and
Technology in Health and Ontario MOH.
• Speaking fee was received in 2011 from Eli Lilly (Canada) Inc.
• consultant to Purdue Pharma (USA) in 2012 re trial of management of chronic pediatric pain.
• member of Data Monitoring Board, ApoPharma Ltd 1995-2012
evolution or extinction
New technologies are receiving increasingly close scrutiny.
Ultimately public-private views must align in a true risk sharing partnership to optimize benefit.
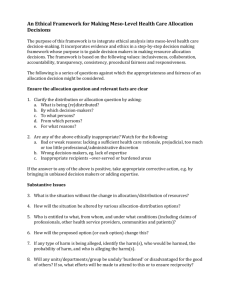
Applied health research & evaluation for decision makers: Perspective matters questions about health interventions
• Does it work in real life?
• For whom?
• Better than current treatments?
• Is it safe?
• Compared to what?
• At what cost?
public health decision-makers
Reimburse?
Recommend treatments?
Healthcare direction physicians
Treat my patients?
« The best for my patients » patients
What to choose?
« The best for me »
« The best for my population »
J-P Collet, CFRI, Vancouver, 2008
Key messages
▪ complexity
▪ measurement
▪ uncertainty and choice
▪ prioritization
▪ implementation
Determination of Benefit and Risk is at the core of present decision-making about therapeutic and diagnostic innovation.
It is essential to preserve a public policy environment that fosters incremental innovation.
VALUING INNOVATIVE PRODUCTS: a deliberative process that considers context
• evidence-informed vs evidence-based
• increased focus on comparative effectiveness
• observational studies that go beyond RCTs
• effective use of colloquial evidence (Lomas et al)
• EPOC approach (Cochrane Effective Practice and Organization of Care Group)
Expectations of evidence based medicine must be tempered by reality.
The real world is a special case. (Andrew Herxheimer, Oxford University)
Key issues
1. The new economy requires innovation to drive competitiveness and improved productivity.
2. Different levels of government seek different returns on investment.
3. Investment in evaluation and implementation science lags behind the cost driver of new technologies.
4. Academic attitudes to technologic advance in health
(commercialization) is erratic and sometimes hostile.
The academic milieu is inadequately supportive of innovation
• Human resource plans impede recruitment of researchers in applied, evaluative, or implementation science.
• University research is often not well aligned with public/patient
(eg, CIHR-SPOR)
• It is easier to accept the dogma of evidence based medicine than to pursue an approach that recognizes culture and values.
• Many academics openly oppose the innovation/ commercialization agenda.
Globe and Mail 16 September 2011 by KEVIN LYNCH and MUNIR SHEIKH
Wanted: culture of innovation
“Productivity isn’t everything,” Paul Krugman once wrote in his
New York Times column, “but in the long run it is almost everything.”
Strange then, with Canada’s poor productivity and innovation performance compared with that of the U.S., that we remain complacent . Where’s our sense of urgency?
Productivity growth is the dividend produced by innovation. So our difficulties are placed in sharp relief when we see that our productivity growth has dropped substantially, from average growth of close to 3 per cent annually from 1961 to 1980, to under 1 per cent since 2000. And that gap between Canada and the U.S. has widened in the past decade, despite the relative improvement of macroeconomic fundamentals in our country.
LIFE IN THE BALANCE
How do researchers and policy-makers decide on the value of health?
Daniel Cressey looks at
Britain’s National Institute for Health and Clinical Excellence
Nature 2009;461(17);336-9
2012 Health Canada CADTH initiative
▪ HTA collaborative steering committee
▪ inclusive of provinces, regions and stakeholders
▪ charged with preparation of Health Technology Strategy 2.0
(renewal of 2004 strategy)
▪ seeks agreement on transparent decision making shift from HT assessment…
… to HT management
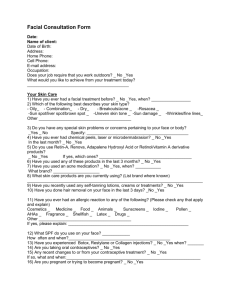
Health technology management
macro: governments and regional health authorities
▪ regulate introduction and use, including coverage
meso: hospitals
▪ address issues re acquisition and impact analysis
▪ prioritization of resource use
micro: providers
▪ participate in field evaluation
▪ establish clinical practice guidelines
Pan Canadian health technology strategy 2.0
▪ assess new technology as a cost driver
▪ address sustainability of the healthcare system
▪ consult with potential end-users and decision-makers
▪ emphasize contextualization of evidence
▪ training and assurance of human resources for evaluation and implementation science
Closing the know-do gap
Both valleys can easily be made deeper and wider by overzealous investigators, regulators, government decision-makers.
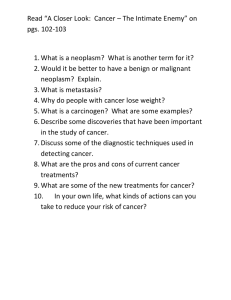
Valuing health outcomes: Factors warranting consideration alongside cost benefit
• lack of, or inadequacy of, alternative treatments
• seriousness of the condition (rights of rescue)
• affordability from the patient perspective
• financial implications for government
• equity objectives
• social values
• potential overall impact of innovation
Daniels and Sabin 1998
There are four elements of legitimacy and fairness in public decisionmaking:
stakeholder involvement
publicity (transparency, dissemination)
revision or appeal
leadership, including accountability for reasonableness
Health Affairs 1998;17:50-64.
The relationship between social value and incremental cost per quality-adjusted life-year (QALY)
LOWER
INCREMENTAL
COST PER QALY
HIGHER SOCIAL VALUE
C
A
B
HIGHER
INCREMENTAL
COST PER QALY
LOWER SOCIAL VALUE
M F Drummond, 2007
The challenge in achieving appropriate valuation of outcomes by decision-makers climbing a Wall of Fear
• inertia may be safer
• high cost of innovation
• interplay of values and evidence
• divergence in social values
• ambiguity re ‘effectiveness’
• lack of consensus on methods
• constraints on access to data
Resolution requires an innovative approach to risk sharing agreements.
The Ontario experience:
An example of best practice
OHTAC decision determinants
overall clinical benefit
consistency with expected societal ethical values
value for money
feasibility (ease) of adoption
HEALTH SYSTEM SUSTAINABILITY
Leadership and Innovation
The data deluge The Economist 25 Feb 2010
Knowing what works in health care: A roadmap for the nation
January 24, 2008
In 2009 the Obama administration committed
$1.1B to comparative effectiveness research.
There ain’t nothin’ in the middle of the road
‘cept yellow lines and dead armadillos.
Jim Hightower, Texan senator
The Canadian health system in its present form is not sustainable.