Cost-Effectiveness of Statins for Primary Cardiovascular Prevention
advertisement

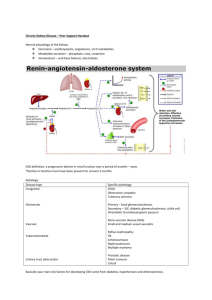
Cost-Effectiveness of Statins for Primary Cardiovascular Prevention in Chronic Kidney Disease (Technical Appendix) Table of Contents: Text: Mortality in End-Stage Renal Disease Modeling CKD Progression Determining Baseline Cardiovascular Risk Calibrating Rates of Non-Cardiovascular Death Selected Model Assumptions Deterministic Sensitivity Analysis Results and Exploratory Analyses Probabilistic Sensitivity Analysis Tables: Table S1: Studies on Risk Reduction from Statins in Mild-to-Moderate (Stage 3) CKD Table S2: Modeled Versus Reported Life Expectancy in Men under Different Scenarios (prior to use of Statins) Table S3: Modeled Versus Reported Life Expectancy in Women under Different Scenarios (prior to use of Statins) Table S4: Statins at Average Retail Prices – Health Benefits, Costs, and Incremental Cost-Effectiveness Ratio from Statin Therapy for Patients with Different Age, Sex, and Cardiovascular Risk Profiles Table S5: Detailed Results from the Base Case Table S6: Annual Mortality Rate with ESRD by Incident Age Table S7: Studies on Annual Rate of CKD Progression Table S8: Framingham-Based Probability of Stroke in One Year by Age in Patients with Moderate Hypertension Table S9: Framingham-Based Probability of Myocardial Infarction in 1 Year by Age in Patients with Moderate Hypertension Table S10: Probabilistic Sensitivity Analysis Inputs Table S11: Costs and Distributions for ESRD Figures: Figure S1a: Model Schematic – Cardiovascular Disease Model Figure S1b: Model Schematic – Chronic Kidney Disease Model Figure S1c: Model Schematic – Statin Toxicities Model Figure S2: Cost-effectiveness of Statins under Different Assumptions about CKD Progression Figure S3: Statins at Average Retail Prices – Differing Cardiovascular Risk Groups in Women Figure S4: Statins at Average Retail Prices – Differing Cardiovascular Risk Groups in Men Figure S5 Sensitivity Analysis – Severity of CKD upon Statin Initiation Figure S6: Sensitivity Analysis – Relative Risk Reduction in CKD Progression from Statins in the Base Case Figure S7: Sensitivity Analysis Assuming Statins Cause Diabetes Figures S8: Sensitivity Analysis Assuming Irreversible Memory Loss from Statins Figure S9: Probabilistic Sensitivity Analysis in 65 Year Old Men Figure S10: Probabilistic Sensitivity Analysis in 50 Year Old Men Figure S11: Probabilistic Sensitivity Analysis in 65 Year Old Women Figure S12: Probabilistic Sensitivity Analysis in 50 Year Old Women Figure S13: Survival after Developing ESRD by Age of Onset Figure S14: Proportion of Simulated Cohort in Each CKD Stage Assuming Constant GFR Decline for Each Individual Figure S15: Proportion of Simulated Cohort in Each CKD Stage Assuming New Rate of Decline for Each Individual per Year Figure S16: Modeled CKD Progression in 50 Year-olds under Different Assumptions about Within-person Variability in Rate of Progression Figure S17: Modeled CKD Progression in 65 Year-olds under Different Assumptions about Within-person Variability in Rate of Progression Figure S18: Modeled CKD Progression in 80 Year-olds with Different Assumptions About Within-person Variability in Rate of Progression Figure S19: 10-year Probability of MI in Men with Baseline Characteristics by Age Figure S20: 10-year Probability of MI in Women with Baseline Characteristics by Age Figure S21: Relative Increase in Mortality in Men with Stage 3a CKD vs. No CKD by Age Figure S22: Relative Increase in Mortality in Men with Stage 3b CKD vs. No CKD by Age Figure S23: Relative Increase in Mortality in Men with Stage 4 CKD vs. No CKD by Age Figure S24: Estimated Cost of Healthy Year Figure S25: Quality of Life in Healthy Individuals with Age Figure S26: Sensitivity Analysis of Rate of CKD Progression Figure S27: Sensitivity Analysis – Relative Risk Reduction in CV Events from Statins in Stage 3 CKD Figure S28: Sensitivity to Rate of Rhabdomyolysis for 50 Year-old Men Experiencing Different Relative Risk Reductions from Statins. Figure S29: Deterministic Sensitivity Analyses in Women Figure S30: Deterministic Sensitivity Analyses in Men Additional Results when Statins are obtained at Average Retail Prices: Table S12: Statins at Average Retail Prices – Detailed Results from the Base Case Figure S31: Statins at Average Retail Prices – Cost-effectiveness of Statins under Different Assumptions about CKD Progression Mortality in End-Stage Renal Disease (ESRD) Upon progression to end-stage renal disease, we no longer accounted for different causes of death. Consequently, major health events following progression to ESRD (stage 5 CKD) such as CV events, kidney transplantation, timing of dialysis therapy, and dialysis modality, were not explicitly modeled. Instead, mortality each year was a function of 1) Age of development of ESRD; 2) Years since development of ESRD. Mortality rates were calculated from the United States Renal Data System (USRDS) report of all-cause mortality in the ESRD population, and include all ESRD patients in the United States. Consequently, the average mortality rate includes mortality from the mix of ESRD patient modalities (such as peritoneal dialysis or kidney transplant) at each age range in the United States. For each interval reported by USRDS, we assumed a constant hazard of death. For example, USRDS publishes ESRD mortality in the 1st 3 years of ESRD, then mortality in the 1st 5 years of ESRD. To determine mortality rates in years 3 – 5, we divided survival to 5 years by survival to 3 years and calculated the associated annual rate of death. Annual rates were calculated using the most recent survival data available. (See table S6 and figure S13 for detail on ESRD mortality estimates). To account for a range of uncertainty due to potential differences between the composition of ESRD patients of a given age group nationally and within modeled cohorts, we applied a range of +- 20% for mortality in ESRD in deterministic sensitivity analysis. Estimates for probabilistic sensitivity analysis were based from varying the proportion of transplant recipients and mix of patient co-morbidities in the ESRD population. Modeling CKD Progression In the base case, we assumed that patients had mild-to-moderate stage 3a CKD with hypertension and a glomerular filtration rate (GFR) of 50 ml/min/1.73m2. Probability of progression from stages 3a to 3b, 3b to 4, and 4 to 5 (ESRD) were obtained from a separate microsimulation model implemented in SAS software. Published observations from several comparable cohorts of CKD patients were used to estimate a mean annual rate of GFR decline and population standard deviation (1-4). In the base case, patients were randomly assigned an eGFR decline from a population distribution with a mean annual eGFR decline of 1.36 ml/min/1.73m2 and standard deviation of 3.75. Because these patient cohorts included many patients with hypertension, the effect of hypertension on CKD progression was not modeled separately. Additionally, because data suggest statins do not modify CKD progression (5-7) despite modifying incidence of CVD, we assumed that patients who develop CVD do not experience differential rates of CKD progression. (Table S7) The cohort analyses reporting average rates of GFR decline are generally of limited duration. For example, the mean duration of follow-up in the 4 studies used for estimating rate of GFR decline was 3.12 years. There are few reports in the literature about within person variation in rate of progression over a longer period of time. For example, if a person’s GFR declines by 2 ml/min/1.73m2 in one decade it is unknown whether they can be expected to progress faster, slower, or at the same rate over the next decade. The degree of correlation in rate of decline within individuals has a significant impact on timing and the proportion of a cohort ultimately progressing to more advanced stages of CKD and ESRD. Figures S14 and S15 illustrate differences in the proportion of simulated individuals progressing through each CKD stage over time depending on assumptions about within individual correlation (prior to including death as a competing risk). When each patient is assumed to receive a constant rate of GFR decline (Figure S14), some patients progress rapidly to ESRD, while others remain in stage 3a indefinitely. In contrast, if there is no correlation within a patient’s rate of progression each year, eventually the entire population progresses to stages 4 then 5 CKD, although progression to more advanced CKD stages takes longer (Figure S15). To determine which of these two assumptions produces CKD progression rates more reflective of what occurs when actual population cohorts are observed over long periods of time, we simulated our CVD and CKD model without statins under varying assumptions about withinpatient correlation in CKD progression in the base case. Because death is a competing risk with ESRD, the proportion of a cohort progressing to ESRD over time is determined by the relative rates of death and rate of CKD progression since patients must survive to progress to ESRD. Several cohort studies over 10-15 year periods have reported the proportion of patients with stages 3 and 4 CKD who progress to ESRD (4,8-10). In a European cohort of 3047 patients with stage 3 CKD the 10-year incidence of ESRD was 4% (95% CI 3%-6%) (4), while the HUNT II study of patients in Norway found a 10-year rate of ESRD of 2.2% in those with a GFR between 45-60 ml/min/1.73m2 (8). A comparison of the population from HUNT II to the U.S. population using NHANES concluded progression to ESRD is 2.5 times more likely in the U.S., which would translate to approximately 5.3% progression to ESRD in the U.S. (8). In a U.S. cohort from the Cardiovascular Health Study of older patients (mean age 75), 3% of patients with eGFR between 45 and 60 ml/min/1.73m2 progressed to ESRD in 9.7 years of follow-up (9) while the MRFIT study of patients at high CV risk in 1973 found a risk of ESRD between 1.5 and 2% at 10 years, 2.5% at 15 years, and 5% at 25 years (10). The results from MRFIT are likely to be an underestimate of current day progression rates due to higher mortality rates in patients prior to progression to ESRD in the 1970s and 1980s. These studies suggest that progression to ESRD in the U.S. occurs in approximately 2 to 5% of patients at 10 years with perhaps twice that amount over a longer period such as 25 years. Figures S16-18 illustrate the proportion of 50, 65 and 80 year-olds who progress to CKD stages 4 and 5 under 1) Assumption of constant rate of CKD progression within patients; 2) Assumption of new rate of progression assigned at random from the population distribution every year. As the figures illustrate, if CKD progression occurs at a constant rate for each individual, in 10 years approximately 25% of 50 year-olds, 21% of 65 year-olds and 9% of 80 year-olds will have progressed to ESRD. In contrast, if patients receive new progression rates every cycle, 5% of 50 year-olds, 4% of 65 year-olds, and 1% of 80 year-olds progress to ESRD in 10 years. Because the rates of ESRD progression resulting from the assumption that an individual’s rate of CKD progression can vary every year are more consistent with those observed in long-term cohorts, we used this assumption in the simulation model. Determining Baseline Cardiovascular (CV) Risk Baseline risk for myocardial infarction (MI) and stroke were derived from Framingham Risk scores (11,12). 1-year risk of MI and stroke were estimated for men and women with no hypertension, mild hypertension (SBP 120-130 on treatment) and moderate hypertension (SBP 130-140 on treatment) separately. Baseline CV risk was estimated for a hypothetical patient being treated for moderate hypertension, with a total cholesterol between 160mg/dl and 200mg/dl and no other “traditional” cardiovascular risk factors aside from age. The annual probabilities of stroke for each age in men and women with and without hypertension were calculated using a Framingham prediction model described by Wolf et al (12). (Table S8) Framingham risk scores were calculated for men and women at each age between 50 and 80 for each CV risk (in the base case a patient with moderate hypertension with a total cholesterol between 160mg/dl and 200mg/dl and no other cardiovascular risk factors aside from age) (11). Since the Markov Model operated in cycles less than 1 year in duration, and extra step was taken to transform 10-year probabilities of MI predicted from Framingham risk scores into 1-year probabilities for inclusion in the Markov model. To do this, the annual rate of MI at each age was expressed as a function of age and two constants in the following form: (Rate of MI)Age = α*e^β*(Age) A solver function was used to determine α and β such that the sum of the absolute values of the difference between the 10-year probabilities of MI resulting from the estimated rate function and the 10-year probabilities of MI predicted from the Framingham risk scores were minimized. For men with the baseline characteristics, the Framingham-based 10-year probability of MI reached a maximum of 20% at age 75 while for women it reached a maximum of 14% at age 75. As a result, the solver function minimized differences in 10-year probabilities between ages 50 to 75 in men and women. However, to allow for a smooth transition to the maximum annual rate (the constant annual rate associated with 20% 10-year probability of MI in men and 14% probability of MI in women) the rates produced from the rate function were used for several years after ages 75 in men and 70 in women until the annual rate reached the maximum rate, at which time the maximum rate was used for all subsequent ages. (Table S9; Figure S19; Figure S20) Because the model tracks patient events at 3 month intervals, 1-year probabilities of MI were converted to 3-month rates using an exponential transformation: 𝑃3−𝑚𝑜𝑛𝑡ℎ = 1 − 𝑒 1−𝑙𝑛(1−𝑃12−𝑚𝑜𝑛𝑡ℎ𝑠 ) ) 4 −( Calibrating Rates of Non-Cardiovascular Death Prior to Inclusion of Chronic Kidney Disease (CKD): Acute complications of MI and stroke and an increased risk of death following these events comprise a sizable portion of mortality in the general population represented in U.S. Life Tables and in patients with chronic kidney disease. Consequently, by including MI and stroke – and an increased hazard of death following these events – as a competing risk of death our model would overestimate mortality in the population by “double counting” death associated with these events. To correct for this, an age and gender-based adjustment factor was applied to the rate of death obtained from U.S. Life Tables in every cycle of the model to estimate the rate of nonCV mortality. The adjustment factor was first determined prior to including additional risks associated with CKD in the model. The following steps were performed to make this adjustment: 1) The prevalence of hypertension in the U.S. was obtained from the National Health and Nutrition Examination Survey for men and women at each decade of age (13). Probabilities of MI and stroke as a function of age for non-hypertensive men and women were generated from Framingham scores using the method described above. 2) The cardiovascular model was run for individual cohorts of men and women ages 50, 60, 70, and 80 prior to inclusion of assumptions related to CKD. For each age and gender cohort the model was run twice. First, it was run for individuals without hypertension (using Framingham-based cardiovascular risks derived for that population). Second, it was run for individuals with moderate hypertension. For each age cohort, the model was run for 10 years and annual mortality rates were calculated over that period. 3) For each simulated year, a weighted average of the mortality rate from the hypertensive and non-hypertensive cohorts was obtained based on prevalence of hypertension in the U.S. population for a given age group and gender. 4) Average life expectancy over 10 years (based on the weighted average of the mortality rates in the hypertensive and non-hypertensive cohorts) was compared with 10-year life expectancy from U.S. life tables. An age and gender based adjustment was made to rate of death in each 10-year age and sex group such that 10 year mortality was within 0.1 percent of that from the U.S. life tables. After Inclusion of Stages 3 and 4 CKD: Although there are few reports in the literature of the increased hazard of noncardiovascular death in patients with CKD compared to those without CKD, several large epidemiologic studies have described the magnitude of the increased risk of cardiovascular events and death from all causes experienced by patients with stages 3 and 4 CKD compared with the non-CKD population (14-16). In our decision analytic model, in patients not given statins the presence of CKD (stages 3a, 3b, and 4) modify the likelihood of mortality through the following mechanisms: 1) Increasing the risk of MI and stroke; 2) Increasing the risk of death from acute MI and stroke; 3) Increasing the risk of death following MI and stroke; 4) Increasing the risk of death from non-cardiovascular causes. Since the increased risk of CV events (14,15) and increased risk of death (16) due to CV events in the CKD vs. non-CKD population is well described, and the increased risk in death from all causes (14-16) is well described , we imputed the hazard of non-cardiovascular death associated with CKD stages 3a, 3b and 4 such that the model produced accurate ratios in the rate of death from any cause in the CKD versus non-CKD populations. This hazard of non-CV death was applied prior to acute cardiovascular events. This was done in the following steps: 1) 4 separate versions of the model were created. One version consisted of cohorts with hypertension but no CKD (i.e. without the increased probabilities of death and CV events associated with CKD). A second version consisted of cohorts with stage 3a CKD who did not progress to 3b, a third consisted of cohorts with stage 3b who did not progress to stage 4, and a fourth version consisted of cohorts with stage 4 CKD who did not progress to ESRD. 2) The rates of mortality from all causes in the stage 3a, 3b and 4 CKD versions of the model were compared with mortality rates in the non-CKD versions to obtain risk ratios associated with each stage of CKD. 3) For each comparison – 1) stage 3a CKD versus no CKD; 2) stage 3b versus no CKD; 2) stage 4 CKD versus no CKD – eight separate cohorts were created including men and women starting the Markov model at ages 50, 60, 70 and 80. Each cohort was followed for 10 years from the start age, and the annual rate of mortality in each year was calculated. 4) Mortality rates for identical age-and-gender-matched cohorts were compared (e.g. mortality for 60 year old women with stage 4 CKD was compared with mortality for a 60year-old woman with hypertension and no CKD). Among matching cohorts, a risk ratio was calculated each year by dividing the mortality rate in the CKD group by the mortality rate in the non-CKD group. 5) For each comparison, the average of the ratios for all 8 paired cohorts was calculated. This number provided an estimate of the relative difference in all-cause mortality in patients with CKD stages 3a, 3b, and 4 compared with no CKD 6) The imputed values – non-cardiovascular hazard of death associated with CKD stages 3a, 3b and 4 – were incrementally increased until the average all-cause mortality in CKD versus no-CKD produced from the modeled cohorts was equal to that reported in the literature (1.2 for stage 3a CKD, 1.8 for stage 3b CKD and 3.2 for stage 4 CKD). (14,16) (See figures S21-23) Tables S2 and S3 illustrate how life expectancy by age for men and women changes with the addition of each disease state. Life expectancies from U.S. Life Tables are included for comparison. Each addition of a new disease state (hypertension, non-progressive CKD, progressive CKD) reduces life expectancy as expected. Selected Model Assumptions Probability and Hazard Rate Assumptions: The probabilities of death due to an acute MI or stroke were derived from large observational studies from the general population (16-23). The added probability of death due to CKD was derived from comparisons of mortality rates following acute MI and stroke in patients with and without CKD (16). The increased hazards of death following an acute MI and stroke were derived from observational studies estimating the increased hazard of death following CV events after controlling for other patient characteristics (20-24). Cost, quality of life, and incidence of Myopathy: The probability of myopathy while on statins was obtained from a report in the literature. (25) Patients with myopathy experienced a one-time cost of checking a creatinine kinase (CK) level, obtained from Medicare Laboratory Fees (26), while the quality of life loss due to myalgias was derived from the quality of life reported for mild osteoarthritis of the hip that does not impair function (27). Probability of Rhabdomyolysis: Literature on adverse events such as myalgias and rhabdomyolysis is not conclusive. Many of the clinical trials involving statins found no increased risk of rhabdomyolysis, although patient selection, study size, and closer monitoring in the trial setting likely contributed to the absent risk. Studies of adverse events when statins have been given in the community provide important insight about the magnitude of risk in the general population (28-30). For example, one review found a rate of 0.44 cases of rhabdomyolysis per 10,000 person-years of patients taking statins (29). Excluding patients taking cerivastatin (which has been removed from the market due to muscle toxicity) a study of adverse events reported to the U.S. Food and Drug Administration (FDA) found rates consistent with 0.61 cases per 10,000 patient-years assuming patients fill 2 prescriptions per year (31), while a study in Sweden found rates consistent with 1.72 cases per 10,000 person years (30). It is unclear to what degree CKD elevates this risk. One epidemiologic survey of patients with kidney disease found a rate of 7.62 cases per 10,000 person years, which was comparable to the rate found among healthy people taking high-dose statins (28). The same analysis compared risk of rhabdomyolysis in CKD using a multivariate model and found an increase in the odds of rhabdomyolysis of 3.75 in people with kidney disease compared with those without (28). In our base case, we used an average of the upper and modified lower values that have been reported. To develop a modified lower value, we multiplied the rate of 0.44 cases per 10,000 person-years reported by Graham et al. for the general population by the increased odds of rhabdomyolysis associated with CKD (3.75). The upper value was the 7.62 cases per 10,000 patient-years in patients with CKD reported by McClure et al. (28). The average of these estimates (used in our base case) was 4.64 cases per 10,000 person years. Due to large uncertainty about the risk of muscle toxicity in CKD we explored a wide range on sensitivity analysis, varying the estimated risk of rhabdomyolysis by factors of 10 in each direction, which is similar in magnitude to the differential rates of rhabdomyolysis reported by McClure et al. between patients in the general population taking high dose and low dose statins (7.7 vs. 0.86 cases per 10,000 individuals) (28). Our assumptions about the probability of death among patients who develop rhabdomyolysis were derived from literature reporting mortality rates from rhabdomyolysis in the general population (25,28-30,32,33). The cost associated with rhabdomyolysis was obtained from case reports of patients hospitalized with rhabdomyolysis (34). We assumed patient experienced zero QALYs during a 2-week admission for rhabdomyolysis. Risk Reduction from Statins: A number of secondary analyses of large clinical trials on statins have estimated the treatment effect from statins for both primary and secondary prevention in patients with early CKD (35-38). The recently reported SHARP trial describes reduction in cardiovascular events in patients with more advanced CKD (39). For patients with stage 3 CKD, we used the relative risk reduction in cardiovascular mortality published from a Cochrane Review of statins in CKD (5). This analysis was primarily reflective of results from the Pravastatin Pooling Project, (37) and reports risk reductions similar in magnitude to two recently published meta-analyses (6,7). (Table S1) The ranges on sensitivity analysis came from a combination of the meta-analysis and Pravastatin Pooling Project. For patients with stage 4 CKD, we used risk reduction from the SHARP trial. When testing cost-effectiveness of brand name rosuvastatin we used results from a secondary analysis of patients with CKD from the JUPITER trial (38). Cost of healthy year: Medical costs associated with the healthy state (i.e. no history of cardiovascular disease, prior to addition of costs associated with CKD stage) were obtained from published literature (40). To avoid bias associated with the categories used for cost reporting, we interpolated a smoothed cost curve. This was done with the following assumptions: 1) Costs increase linear with age between reported categories 2) Costs reported for each age group represent the cost incurred at the median age of that cohort. Figure S24 illustrates a comparison of the reported and interpolated health care costs. Additional Cost of Stage III CKD, Stage IV CKD, and ESRD: The incremental increase in medical costs due to stages III and IV CKD were obtained from Smith et al. (41). They represent the incremental cost associated with CKD observed in a managed care population (Kaiser Permanente Northwest), after adjusting for demographic and comorbid conditions in a multivariate analysis. These costs were derived from departmental expenditures, administrative costs, indirect costs and joint costs multiplied by utilization volume. The cost of ESRD was obtained from the average paid per patient by Medicare in 2008 reported by the USRDS Atlas of ESRD. We used Medicare costs because it is the primary payer for ESRD. Because the USRDS Atlas also includes outpatient prescription drug costs for patients with and without prior kidney transplant, these were included in the cost estimates. While we did not explicitly include the cost of statins for patients who develop ESRD in the model, the ESRD total costs used in the model do reflect the degree of continued statin use that occur in patients with ESRD in the United States from whom these costs were estimated. Cost of Myocardial Infarction and Stroke: The cost of an acute myocardial infarction was obtained by Kauf et al. (42) and was based upon the average Medicare hospital and physician reimbursement paid in 2002. The costs in the first year and in subsequent years after an MI were obtained from cost data collected from a clinical trial (43). Costs in the first year after an MI were obtained from an average of the cost following an MI in the treatment and control arms of the clinical trial, while the cost for subsequent years was obtained from reported costs in the treatment arm since control arm costs appeared unrepresentatively low. The cost of an acute stroke, the cost of the 1st year following a stroke, and the cost in subsequent years following a stroke were derived from three studies (44-46). The cumulative first year costs (cost of acute stroke and remaining first year costs) were comparable in the three studies (In 2010 dollars: $33,158 in Samsa et al. (44), $26,287 in Leibson et al. (45) and $23,243 to $31,665 depending on age by Taylor et al. (46)). We used the estimates from Leibson et al. in the base case since their estimates are in the range Taylor et al. reports and comparable to the cost reported by Samsa et al. which comes from Medicare claims. The estimates from Leibson et al. are based on inpatient and outpatient charges in a healthcare system in Rochester, Minnesota in 1987 – 1989. The cost of subsequent years following a stroke were obtained from Samsa et al. and is based from Medicare claims in patients over 65 in the 4 years following a diagnosis of cerebral infarction in 1991 (44). The estimate ($6,060 per year in 2010 dollars) is comparable to the lower age estimate from Taylor et al. (46), which was acceptable since Taylor et al. reports both direct and indirect costs of a stroke. Cost of Statins: In the base case, the annual cost of generic statins available from discount retailers and integrated health systems was derived from a Wal-Mart online price list (47) and Zen Rx Research. (48) Average retail prices were obtained from Consumer Reports “Best Buy Drugs” (47). Cost of laboratory testing and physician monitoring came from the Medicare clinical laboratory and physician fee schedules (26,49). Quality of life in a healthy year: Quality of life in the healthy population varied with age in accordance with the addition of comorbidities that occur with population aging. These estimates were obtained from the Beaver Dam study (50) and were used as a baseline from which to add any additional quality of life decrements associated with chronic kidney disease, cardiovascular disease, cerebrovascular disease, or myopathy. Age-based QALYs are reported in Beaver Dam study for specific age groups. To allow for a continuous decrement of QALYs with aging, rather than step-wise, we made the following assumptions: 1) The QALY associated with a given age range was equal to the QALY for individuals at the median age within that range. 2) QALY decreases linearly between any two age ranges. From these assumptions, we interpolated QALYs for each age and sex. Figure S25 illustrates the interpolated vs. reported values. Quality of life based on CKD stage: Quality of life has been shown to decline due to burden of CKD. While the decline in quality of life is small in early-moderate stage 3 CKD, it becomes more significant as CKD advances. Estimates of quality of life in CKD came from several sources. Gorodetskaya et al. published “Health-related Quality of Life and Estimates of Utility in Chronic Kidney Disease” where they described the burden associated with stages 3, 4, and 5 (ESRD) CKD (51). Because our model further delineates between stages 3a and 3b, we imputed quality of life for these states. To do this we assumed: 1) Quality of life in stage 3 CKD declined in a linear fashion 2) Quality of life associated with stage 4 CKD began at GFR of 30 (i.e. entry into stage 4) We divided the interval of stage 3 CKD into thirds using the following equation: (1 – QALYstage4)/3 = y. Then, 1 – y was equal to the QALY associated with stage 3a. Meanwhile, 1 – 2y was equal to the QALY associated with stage 3b. With a Stage 4 QALY of .875, this produced stage 3a QALY of 0.958 and stage 3b QALY of 0.917. The average, 0.9375 was nearly identical to 0.93, reported by Gorodetskaya et al. for the average QALY associated with stage III CKD. QALY associated with stage 5 CKD (i.e. ESRD) was reported as 0.704. This is also consistent with several indices published in “One Thousand Health Related Quality of Life Estimates (27)”. Quality of life loss in patients with ESRD (0.704) was derived from an analysis by Gorodetskaya et al. under the “effects of kidney disease” for patients with a GFR under 15 ml/min/1.73m2 or on dialysis (51). This was comparable to the range reported by Tengs et al. (0.50 to 0.84) (27) for various dialysis-related conditions. Quality of life following myocardial infarction and stroke: Quality of life following a myocardial infarction was derived from Tengs & Wallace for the category “a history of coronary heart disease” and was 0.80 (27). This was lower than the quality of life for survivors of myocardial infarction reported in another analysis (0.87), but the latter analysis excluded patients with congestive heart failure(52). Consequently the higher estimate motivated the upper range (0.90) used in the deterministic sensitivity analysis. The lower range in the deterministic sensitivity was based on estimates reported by Tengs & Wallace (27) for various coronary artery disease-related conditions and was 0.50. For quality of life following a stroke, baseline assumptions and the range in the deterministic sensitivity analysis were derived from Tengs & Wallace (27). The baseline assumption was 0.80, while the deterministic sensitivity assumption included a range of 0.40 to 0.92. Deterministic Sensitivity Analysis Results and Exploratory Analyses Virtually all of the model’s assumptions were tested using one-way sensitivity analysis. These analyses provide several insights. First, lower rates of CKD progression led to improvement in the cost-effectiveness of statins in women; an annual GFR decline from 1.0 to 2.0 ml/min/1.73m2 led to statins costing between $49,500 to $77,000 per QALY gained in 50 year-old women. (Figure S26) In 65 year-old men and women, the cost of statin therapy ranged from $13,800 to $40,100 per QALY gained over the range of relative risk reductions described from statins in CKD stage 3. (Figure S27) In a 2-way sensitivity analysis, cost- effectiveness of statins therapy was more sensitive to the rate of rhabdomyolysis in younger men if the relative risk reduction from statins is diminished (i.e., a diminished treatment effect with higher rates of complications) than our baseline assumption. (Figure S28) If Statins were to reduce CKD progression, they become more cost-effective. This occurs with relatively low benefits in CKD progression such as a 5 percentage point reduction in rate of progression. (Figure S6) The results do not vary markedly when the remaining cost, quality-of-life, probability, and hazard assumptions are varied. (Figures S29-30) Exploratory analyses of additional statin side-effects: Due to recent reports of an increased risk of additional side-effects from statins, we conducted sensitivity analyses where 1) patients had a risk of developing diabetes while on statins; 2) patients had a risk of developing irreversible memory loss while on statins. (53,54) The following estimates of the probability of diabetes, costs, quality of life, and increased hazard of death with diabetes were obtained from literature: Probability of diabetes while on statins: 2 cases per 1,000 person years (53). Additional annual medical cost due to diabetes: $6,702 in 2010 dollars (55). Quality adjusted life years associated with diabetes: 0.80 (56). Increased hazard of death in all health states associated with diabetes: 2.31 (57). It is important to note that data on increased risks of diabetes from statin use in CKD patients are currently extremely limited. This exploratory analysis is conservative from the point of view of statins’ cost-effectiveness in the CKD population because it potentially includes costs, hazards or death, and quality of life decrements associated with CKD and CVD twice (once in the model without diabetes, and again as a part of the cost, quality of life, and hazard estimates due to diabetes).This implies that the decrements from each additional case of diabetes while on statins applied in the model are likely higher than that which would be observed in an empirical study. The following estimates of the probability of irreversible memory loss while on statins and quality of life associated with this condition were also obtained from literature (54,58): Probability of irreversible memory loss while on statins: 1.1% of statin users (54). Quality of life associated with mild memory loss: 0.82 reduction in QALYs (58). If statins cause increases in type II diabetes rates for patients with CKD, the ICER from statin increases to $74,911 per QALY gained in 65 year-old men (range from $60,662 to $177,608 per QALY gained in men of different ages and CVD risks). In women (who have a lower baseline cardiovascular risk), the ICER increases to $336,000/QALY gained in 65 yearolds, and a treatment strategy with statin therapy is dominated by one without statins at ages below 60 (i.e. a strategy without statins yields more quality adjusted life years at a lower cost). Irreversible memory loss increases the ICER to $61,347/QALY gained in 65 year old men and $150,731 per QALY gained in 65 year old women. For younger men, the ICER is as high as $103,795/QALY gained in 50 year olds, while in younger women, it is as high as $704,000/QALY. (Figures S7-8) Probabilistic Sensitivity Analysis Distributions for probabilistic sensitivity analysis were obtained – when possible – from uncertainty in estimates reported in the literature. (See Table S10) In instances where a wide range of estimates have been reported in the literature, the distribution variance was increased to reflect this. Assumptions regarding cost of ESRD were derived from national averages for different age groups published by the USRDS. The degree of uncertainty about ESRD costs for probabilistic sensitivity analysis was estimated by determining a range of costs associated with varying mixes of transplant recipients and privately versus publically insured recipients (upper 95%CI for cost assumed 10% fewer transplants and 10% more privately insured). This uncertainty is likely correlated across age groups. For instance, if there are 5% fewer transplant recipients and 5% fewer privately insured individuals in our modeled cohort compared to prevalent ESRD patients in the United States in one age group, a similar difference is likely to be present in the other age groups. However, because older patients are less likely to receive transplants and are less likely to be privately insured, the magnitude of the cost uncertainty (as a share of average ESRD costs) associated with a given percentage point reduction (or increase) in the number of patients with transplants or privately insured is smaller in older individuals. To account for this attenuation of uncertainty at older ages while maintaining a realistic correlation of uncertainty across age groups, we modeled ESRD cost uncertainty in the following manner: 1) We defined a single uncertainty distribution in terms of the percentage above/below the base case estimates of ESRD costs for 50-59 year-olds. In this case, a normal distribution with mean 1.0 and 95% confidence interval spanning 0.88-1.12. This corresponded to +/-12% of the base case value for 50-59 year-olds. 2) We drew from the normal distribution defined in 1) and subtracted 1.0 to get the percentage difference from the base case 3) We then multiplied this percentage difference by age specific multipliers defined in Table S11, given the lower range of uncertainty in costs for older individuals with ESRD, especially those on Medicare. 4) When then added 1.0 to the number in 3) and multiplied by the base case age-specific ESRD costs, shown for convenience in Table S11 to produce a distribution of agespecific ESRD costs that were correlated across age groups and had lower uncertainty for older individuals with ESRD. Uncertainty regarding mortality in ESRD was obtained from reported mortality in the setting of more or fewer kidney transplants in addition to differing racial and co-morbid mixes in the ESRD population. The analysis adopted a societal perspective, and discounted all healthcare costs and benefits at 3% annually. We used TreeAge software to implement the decision model and to perform the deterministic sensitivity analyses as well as the probabilistic sensitivity analyses. Table S1: Studies on Risk Reduction from Statins in Mild-to-Moderate (Stage 3) CKD Pravastatin Pooling Project (primary prevention) JUPITER (primary prevention) TNT (includes CHD) HR 0.77 0.55 0.68 LCI 0.68 0.38 0.55 UCI 0.86 0.82 0.84 N 4,491 3,267 3,107 RR LCI UCI N 0.8 0.75 0.74 0.66 0.89 0.85 18,781 19,363 0.78 0.76 0.68 0.73 0.89 0.8 35,417 45,362 Meta-analyses Navaneethan et al.: CV mortality Non-fatal CV event Palmer et al.: CV mortality Non-fatal CV event - Upadhyay et al.:1 CV mortality 0.82 0.74 0.91 13,211 Non-fatal CV event 0.78 0.71 0.86 18,407 Sources: (5-7,35,37). HR = Hazard Ratio; LCI and UCI = Lower and Upper 95% Confidence Intervals Table S2: Modeled Versus Reported Life Expectancy in Men under Different Scenarios (prior to use of Statins) 50 55 60 65 70 75 80 85 Life Table No CKD, Hypertensive CKD Not Progressing Beyond Stage III Progressive CKD 28.8 24.7 20.7 17.0 13.6 10.4 7.8 5.7 27.9 23.8 20.0 16.4 13.1 10.2 7.7 5.7 22.6 19.1 15.8 12.9 10.2 7.9 6.0 4.5 17.9 15.9 13.8 11.6 9.5 7.5 5.8 4.4 Table S3: Modeled Versus Reported Life Expectancy in Women under Different Scenarios (prior to use of Statins) 50 55 60 65 70 75 80 85 Life Table No CKD, Hypertensive CKD Not Progressing Beyond Stage III Progressive CKD 32.5 28.0 23.8 19.7 15.9 12.3 9.3 6.8 32.1 27.7 23.5 19.5 15.7 12.3 9.3 6.8 27.1 23.1 19.3 15.8 12.5 9.7 7.3 5.4 20.0 18.1 16.0 13.7 11.4 9.1 7.0 5.3 Table S4: Statins at Average Retail Prices – Health Benefits, Costs, and Incremental CostEffectiveness Ratio from Statin Therapy for Patients with Different Age, Sex, and Cardiovascular Risk Profiles Starting Age 10-Year Probability of MI % Increased Cost ($) Gain in Increased life QALYs expectancy (discounted) (undiscounted) (months) Reduced risk of MI or stroke (percent) Incremental costeffectiveness ratio ($/QALY) Men 50 6 7,000 0.09 1.6 4.4 82,600 55 10 6,700 0.09 1.7 4.8 71,800 60 12 6,200 0.10 1.7 5.0 63,500 65 16 5,600 0.10 1.6 5.1 57,200 70 17 4,800 0.09 1.5 5.0 52,600 75 20 4,000 0.08 1.2 4.7 51,800 80 20 3,200 0.06 0.9 4.1 55,400 85 20 2,400 0.04 0.6 3.3 62,600 Women 50 1 7,700 0.03 0.7 2.1 257,700 55 2 7,500 0.04 0.9 2.6 191,700 60 3 7,100 0.05 1.0 3.1 148,000 65 5 6,600 0.06 1.1 3.5 117,000 70 8 5,800 0.06 1.1 3.7 97,800 75 14 4,800 0.06 1.1 3.8 82,800 80 14 3,800 0.05 0.9 3.6 74,300 85 14 2,900 0.04 0.6 3.0 79,300 Because costs are rounded to the nearest $100, incremental cost-effectiveness ratios may be slightly different than the incremental costs and QALYs in the table suggest. Table S5: Detailed Results from the Base Case Statins Cost ($) No statins Difference Discounted QALYs Statins No statins Difference ICER ($/QALY) Men 50 204,300 202,500 1,700 10.74 10.66 0.09 20,500 55 186,300 184,500 1,800 9.59 9.50 0.09 19,600 60 176,200 174,400 1,800 8.44 8.35 0.10 18,900 65 172,100 170,300 1,800 7.31 7.21 0.10 18,000 70 161,500 160,000 1,600 6.14 6.05 0.09 16,900 75 145,700 144,400 1,300 5.04 4.96 0.08 16,300 80 123,200 122,300 900 4.02 3.96 0.06 16,100 85 94,500 94,000 600 3.12 3.09 0.04 15,400 Women 50 230,100 228,400 1,700 11.46 11.43 0.03 56,800 55 216,000 214,200 1,800 10.50 10.46 0.04 46,200 60 209,300 207,400 1,900 9.43 9.38 0.05 39,200 65 206,200 204,300 1,900 8.26 8.20 0.06 33,400 70 194,000 192,200 1,700 6.98 6.92 0.06 29,300 75 174,100 172,700 1,400 5.70 5.65 0.06 25,000 80 146,400 145,400 1,100 4.56 4.51 0.05 21,300 85 111,700 111,000 700 3.58 3.54 0.04 19,800 Because costs are rounded to the nearest $100, cost differences and incremental costeffectiveness ratios may be slightly different than the incremental costs and QALYs in the table suggest. Table S6: Annual Mortality Rate with ESRD by Incident Age Incident ESRD 90 days From: 90 days 1 year 2 years To: 1 year 2 years 3 years Age: 50-59 0.18 0.09 0.11 0.12 60-64 0.24 0.11 0.15 0.17 65-69 0.32 0.14 0.18 0.20 70-79 0.48 0.19 0.25 0.26 80-84 0.65 0.26 0.34 0.34 85+ 0.93 0.28 0.44 0.44 Note: Time intervals include specified interval plus 90 days 3 years 5 years 5 years indefinitely 0.12 0.16 0.20 0.30 0.42 0.50 0.13 0.20 0.27 0.34 0.44 0.49 Table S7: Studies on Annual Rate of CKD Progression Base Case SD: 3.75 SD from AASK --- 3.3, MDRD 4.2, VA approx 3.75 VA study (1) MDRD (2) European (4) AASK (3) Average annual GFR decline -1.152 -3.800 -1.030 -1.640 Sum: Persons 4171 840 3047 1094 9152 Follow-up (years) 2.6 2.2 3.7 4.0 12.5 Personyears 10844.6 1873.5 11172.3 4376.0 28266.4 Study Weight 0.38 0.07 0.40 0.15 1.00 Weighted GFR Decline -0.44 -0.25 -0.41 -0.25 -1.36 Table S8: Framingham-Based Probability of Stroke in One Year by Age in Patients with Moderate Hypertension Age 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 Men 0.0022 0.0023 0.0024 0.0025 0.0027 0.0028 0.0030 0.0031 0.0033 0.0034 0.0036 0.0038 0.0040 0.0042 0.0044 0.0047 0.0049 0.0052 0.0054 0.0057 0.0060 0.0063 0.0066 0.0070 0.0073 Women 0.0010 0.0010 0.0011 0.0012 0.0013 0.0013 0.0014 0.0015 0.0016 0.0017 0.0019 0.0020 0.0021 0.0023 0.0024 0.0026 0.0028 0.0030 0.0032 0.0034 0.0036 0.0038 0.0041 0.0044 0.0047 Age 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 Note: Probability constant after age 84 when the study stopped Men 0.0077 0.0081 0.0085 0.0090 0.0094 0.0099 0.0104 0.0110 0.0115 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 0.0121 Women 0.0050 0.0053 0.0057 0.0061 0.0065 0.0069 0.0074 0.0079 0.0084 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 0.0090 Table S9: Framingham-Based Probability of Myocardial Infarction in 1 Year by Age in Patients with Moderate Hypertension Age 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 Men 0.0046 0.0049 0.0052 0.0055 0.0059 0.0063 0.0067 0.0071 0.0075 0.0080 0.0085 0.0090 0.0096 0.0102 0.0108 0.0115 0.0122 0.0130 0.0138 0.0146 0.0155 0.0165 0.0175 0.0186 0.0198 Women 0.0006 0.0006 0.0007 0.0007 0.0008 0.0009 0.0010 0.0011 0.0012 0.0014 0.0015 0.0017 0.0019 0.0021 0.0023 0.0025 0.0028 0.0031 0.0034 0.0038 0.0041 0.0046 0.0051 0.0056 0.0062 Age 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 Men 0.0210 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 0.0221 Women 0.0069 0.0076 0.0084 0.0093 0.0102 0.0113 0.0125 0.0138 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 0.0150 Table S10: Probabilistic Sensitivity Analysis Inputs Intervention effects: (Targeted Mean Value) Range (95% CI) Distribution CV relative risk reduction from statins (stage 3 CKD and no CKD) 0.80 0.68 0.90 beta CV relative risk reduction from statins (stage 4 CKD) 0.83 0.68 0.94 beta Rate of rhabdomyolysis (per 10,000 person-years) 4.64 2.38 7.66 gamma Probability of death from rhabdomyolysis 0.08 0.06 0.09 beta Probability of myopathy on statins 0.09 0.06 0.13 beta Non-CKD Natural History Parameters: Probability of MI and stroke (Framingham model) (+-20%) lognormal Probability of death from acute MI 0.07 0.06 0.08 beta Increased hazard of death after MI - hazard ratio 1.40 1.00 1.98 lognormal Probability of death from acute stroke 0.12 0.11 0.14 beta Increased hazard of death after Stroke - hazard ratio 2.36 1.95 2.76 normal Increased all-cause mortality (CKD stage 3a) - hazard ratio 1.20 1.10 1.30 normal Increased all-cause mortality (CKD stage 3b) - hazard ratio 1.80 1.70 1.90 normal Increased all-cause mortality (CKD stage 4) - hazard ratio 3.20 3.00 3.40 normal (see appendix text) 0.77 1.27 lognormal Increased risk of MI and Stroke (CKD stage 3a) - hazard ratio 1.40 1.30 1.50 normal Increased risk of MI and Stroke (CKD stage 3b) - hazard ratio 2.00 1.90 2.10 normal Increased risk of MI and Stroke (CKD stage 4) - hazard ratio 2.80 2.65 2.95 normal Increased hazard of death from acute MI due to CKD (all stages) 1.40 1.20 1.60 normal Increased hazard of death from acute stroke due to CKD (all stages) 1.86 1.45 2.26 normal 1.36 1.14 1.60 lognormal CKD-Specific Natural History Parameters: Probability of death from ESRD Rate of CKD progression (ml/min/1.73m2/yr) Table S10 (continued): Quality of life assumptions (Targeted Mean QALY) CKD stage 3a 0.96 0.85 0.11 normal CKD stage 3b 0.92 0.81 0.98 beta CKD Stage 4 0.88 0.69 0.98 beta CKD stage 5 0.70 0.50 0.87 beta Following MI 0.80 0.76 0.84 beta Following Stroke 0.80 0.68 0.90 beta Myalgia 0.80 0.68 0.90 beta Cost assumptions ($2010) (Targeted Mean $) Annual Cost Following MI 4,343 3,534 5,217 gamma Annual Cost Following Stroke 6,060 3,100 9,984 gamma Annual Cost of Stage 3a CKD 1,833 1,493 2,201 gamma Annual Cost of Stage 3b CKD 4507 3,675 5,408 gamma Annual Cost of Stage 4 CKD 5,844 1,201 14,054 gamma Acute cost of MI 11,070 5,551 18,401 gamma First year after MI 7,747 6,850 8,675 gamma Acute cost of Stroke 18,516 15,309 21,955 gamma First year after Stroke 7,770 4,940 11,200 gamma Cost of Rhabdomyolysis 55,794 45,650 66,825 gamma 4 2 7 lognormal Hepatic panel 11.7 1 48 lognormal Level 1 office visit 19.7 9 39 lognormal Monthly cost of Statin Table S11: Costs and Distributions for ESRD Age Age-Based Multiplier applied to the percentage difference drawn from a single uncertainty distribution in the Probabilistic Sensitivity Analysis1 ESRD Cost2 50-59 1.000 66883.6 60-64 1.025 65671.9 65-69 1.041 70077.8 70-79 0.812 77574.5 80-84 0.371 84573.7 85+ 0.246 85509.9 1 Multiplied by the cost drawn from the probabilistic sensitivity analysis 2 Range (95% CI) Includes an estimate of Medicare Part D Costs Range (95% CI) Figure S1a: Model Schematic – Cardiovascular Disease Model Probability of myocardial infarction and stroke are derived from probabilities from a Framingham model multiplied by an additional hazard of cardiovascular (CV) event due to chronic kidney disease (CKD) stage. Independent mortality hazards associated CKD stages are multiplied by mortality rates from U.S. life tables to obtain mortality in the “healthy” state. Mortality following myocardial infarction and stroke are derived from combining mortality from U.S. life tables, mortality hazards following CV events in the general population, and hazards of death in patients with CKD. Figure S1b: Model Schematic – Chronic Kidney Disease Model Not shown in the schematic, the model subdivides stage III CKD into IIIa and IIIb. Figure S1c: Model Schematic – Statin Toxicities Model Rhabdo. refers to rhabdomyolysis. Scenarios where patients develop diabetes or memory loss were modeled separately. We assume patients with diabetes or memory loss remain on statins. Figure S2: Cost-effectiveness of Statins under Different Assumptions about CKD Progression Figure S3: Statins at Average Retail Prices – Differing Cardiovascular Risk Groups in Women Figure S4: Statins at Average Retail Prices – Differing Cardiovascular Risk Groups in Men Figure S5: Sensitivity Analysis – Severity of CKD upon Statin Initiation Figure S6: Sensitivity Analysis – Relative Risk Reduction in CKD Progression from Statins in the Base Case Figure S7: Sensitivity Analysis – Assuming Statins Cause Diabetes *Treatment strategy without statins is the “dominant” strategy (i.e. leads to more quality-adjusted life years at a lower cost) Incremental cost-effectiveness ratio for 60 year old women is $1.5 million /QALY gained, while for 65 year old women it is $338,000/QALY gained Figure S8: Sensitivity Analysis – Assuming Irreversible Memory Loss from Statins Figure S9: Probabilistic Sensitivity Analysis in 65 Year Old Men Figure S10: Probabilistic Sensitivity Analysis in 50 Year Old Men Figure S11: Probabilistic Sensitivity Analysis in 65 Year Old Women Figure S12: Probabilistic Sensitivity Analysis in 50 Year Old Women Figure S13: Survival after Developing ESRD by Age of Onset Figure S14: Proportion of Simulated Cohort in Each CKD Stage assuming Constant GFR Decline for Each Individual Figure S15: Proportion of Simulated Cohort in Each CKD Stage assuming New Rate of Decline for Each Individual per Year Figure S16: Modeled CKD Progression in 50 Year-olds under Different Assumptions about Within-person Variability in Rate of Progression: Figure S17: Modeled CKD Progression in 65 Year-olds with Different Assumptions About Within-person Variability in Rate of Progression: Figure S18: Modeled CKD Progression in 80 Year-olds under Different Assumptions about Within-person Variability in Rate of Progression: Figure S19: 10-year Probability of MI in Men with Baseline Characteristics by Age Figure S20: 10-year Probability of MI in Women with Baseline Characteristics by Age Figure S21: Relative Increase in Mortality in Men with Stage 3a CKD vs. No CKD by Age Figure S22: Relative Increase in Mortality in Men with Stage 3b CKD vs. No CKD by Age Figure S23: Relative Increase in Mortality in Men with Stage 4 CKD vs. No CKD by Age Figure S24: Estimated Cost of Healthy Year Estimates based on reported costs in $2010 of $3,474 for people 50-64, 10,948 for ages 65-74, and 18,968 for 75+. Figure S25: Quality of Life in Healthy Individuals with Age Note: data imputed from Beaver Dam Study where for men aged 45-54, 55-64, 65-74, 75-84, and 84+, QALYs are: 0.0941, 0.874, 0.841, 0.838, 0.817 respectively. For women aged 45-54, 55-64, 65-74, 75-84, and 84+, QALYs are: 0.901, 0.871, 0.833, 0.792, 0.8 respectively. Figure S26: Sensitivity Analysis of Rate of CKD Progression Figure S27: Sensitivity Analysis – Relative Risk Reduction in CV Events from Statins in Stage 3 CKD Figure S28: Sensitivity to Rate of Rhabdomyolysis for 50 Year-old Men Experiencing Different Relative Risk Reductions from Statins. Figure S29: Deterministic Sensitivity Analyses in Women Figure S30: Deterministic Sensitivity Analysis in Men Table S12: Statins at Average Retail Prices – Detailed Results from the Base Case Statins Cost ($) No statins Difference Discounted QALYs Statins No statins Difference ICER ($/QALY) Men 50 209,600 202,500 7,000 10.74 10.66 0.09 82,600 55 191,200 184,500 6,700 9.59 9.50 0.09 71,800 60 180,600 174,400 6,200 8.44 8.35 0.10 63,500 65 175,900 170,300 5,600 7.31 7.21 0.10 57,200 70 164,800 160,000 4,800 6.14 6.05 0.09 52,600 75 148,400 144,400 4,000 5.04 4.96 0.08 51,800 80 125,500 122,300 3,200 4.02 3.96 0.06 55,400 85 96,300 94,000 2,400 3.12 3.09 0.04 62,600 Women 50 236,100 228,400 7,700 11.46 11.43 0.03 257,700 55 221,700 214,200 7,500 10.50 10.46 0.04 191,700 60 214,500 207,400 7,100 9.43 9.38 0.05 148,000 65 210,900 204,300 6,600 8.26 8.20 0.06 117,000 70 198,000 192,200 5,800 6.98 6.92 0.06 97,800 75 177,500 172,700 4,800 5.70 5.65 0.06 82,800 80 149,100 145,400 3,800 4.56 4.51 0.05 74,300 85 113,800 111,000 2,900 3.58 3.54 0.04 79,300 Because costs are rounded to the nearest $100, cost differences and incremental costeffectiveness ratios may be slightly different than the incremental costs and QALYs in the table suggest. Figure S31: Statins at Average Retail Prices – Cost-effectiveness of Statins under Different Assumptions about CKD Progression 1. Al-Aly Z, Zeringue A, Fu J et al. Rate of kidney function decline associates with mortality. Journal of the American Society of Nephrology 2010;21:1961-9. 2. Hunsicker LG, Adler S, Caggiula A et al. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney International 1997;51:1908-19. 3. Lewis J, Greene T, Appel L et al. A comparison of iothalamate-GFR and serum creatinine-based outcomes: acceleration in the rate of GFR decline in the African American Study of Kidney Disease and Hypertension. Journal of the American Society of Nephrology 2004;15:3175-83. 4. Eriksen BO, Ingebretsen OC. The progression of chronic kidney disease: a 10-year populationbased study of the effects of gender and age. Kidney International 2006;69:375-82. 5. Navaneethan SD, Pansini F, Perkovic V et al. HMG CoA reductase inhibitors (statins) for people with chronic kidney disease not requiring dialysis. Cochrane Database of Systematic Reviews 2009:CD007784. 6. Upadhyay A, Earley A, Lamont JL, Haynes S, Wanner C, Balk EM. Lipid-Lowering Therapy in Persons With Chronic Kidney Disease: A Systematic Review and Meta-analysis. Annals of Internal Medicine 2012;157:251-62. 7. Palmer SC, Craig JC, Navaneethan SD, Tonelli M, Pellegrini F, Strippoli GFM. Benefits and Harms of Statin Therapy for Persons With Chronic Kidney Disease: A Systematic Review and Metaanalysis. Annals of Internal Medicine 2012;157:263-75. 8. Hallan SI, Coresh J, Astor BC et al. International comparison of the relationship of chronic kidney disease prevalence and ESRD risk. Journal of the American Society of Nephrology 2006;17:227584. 9. Dalrymple LS, Katz R, Kestenbaum B et al. Chronic kidney disease and the risk of end-stage renal disease versus death. Journal of General Internal Medicine 2011;26:379-85. 10. Ishani A, Grandits GA, Grimm RH et al. Association of single measurements of dipstick proteinuria, estimated glomerular filtration rate, and hematocrit with 25-year incidence of endstage renal disease in the multiple risk factor intervention trial. Journal of the American Society of Nephrology 2006;17:1444-52. 11. Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486-97. 12. Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991;22:312-8. 13. Burt VL, Whelton P, Roccella EJ et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension 1995;25:305-13. 14. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C-y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization.[Erratum appears in N Engl J Med. 2008;18(4):4]. New England Journal of Medicine 2004;351:1296-305. 15. Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. Journal of the American Society of Nephrology 2002;13:745-53. 16. USRDS. Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. United States Renal Data System. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2011. 17. Rogers WJ, Frederick PD, Stoehr E et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. American Heart Journal 2008;156:1026-34. 18. Myerson M, Coady S, Taylor H, Rosamond WD, Goff DC, Jr., Investigators A. Declining severity of myocardial infarction from 1987 to 2002: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2009;119:503-14. 19. McGovern PG, Jacobs DR, Jr., Shahar E et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation 2001;104:19-24. 20. Roger VL, Jacobsen SJ, Weston SA et al. Trends in the incidence and survival of patients with hospitalized myocardial infarction, Olmsted County, Minnesota, 1979 to 1994.[Summary for patients in Ann Intern Med. 2002 Mar 5;136(5):I16; PMID: 11874327]. Annals of Internal Medicine 2002;136:341-8. 21. Petty GW, Brown RD, Jr., Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota, 1975 through 1989. Neurology 1998;50:208-16. 22. Hollander M, Koudstaal PJ, Bots ML, Grobbee DE, Hofman A, Breteler MMB. Incidence, risk, and case fatality of first ever stroke in the elderly population. The Rotterdam Study. Journal of Neurology, Neurosurgery & Psychiatry 2003;74:317-21. 23. Dennis MS, Burn JP, Sandercock PA, Bamford JM, Wade DT, Warlow CP. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke 1993;24:796-800. 24. Gruppetta M, Calleja N, Fava S. Long-term survival after acute myocardial infarction and relation to type 2 diabetes and other risk factors. Clinical Cardiology 2010;33:424-9. 25. Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA 2003;289:1681-90. 26. Services DoHaHRCfMaM. Clinical Laboratory Fee Schedule. 2010. 27. Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Medical Care 2000;38:583-637. 28. McClure DL, Valuck RJ, Glanz M, Murphy JR, Hokanson JE. Statin and statin-fibrate use was significantly associated with increased myositis risk in a managed care population. Journal of Clinical Epidemiology 2007;60:812-8. 29. Graham DJ, Staffa JA, Shatin D et al. Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs. JAMA 2004;292:2585-90. 30. Hedenmalm K, Alvan G, Ohagen P, Dahl M-L. Muscle toxicity with statins. Pharmacoepidemiology & Drug Safety 2010;19:223-31. 31. Alsheikh-Ali AA, Ambrose MS, Kuvin JT, Karas RH. The safety of rosuvastatin as used in common clinical practice: a postmarketing analysis. Circulation 2005;111:3051-7. 32. Ballantyne CM, Corsini A, Davidson MH et al. Risk for myopathy with statin therapy in high-risk patients. Archives of Internal Medicine 2003;163:553-64. 33. Omar MA, Wilson JP. FDA adverse event reports on statin-associated rhabdomyolysis. Annals of Pharmacotherapy 2002;36:288-95. 34. Skrabal MZ, Stading JA, Cannella CA, Monaghan MS. Two cases of rhabdomyolysis associated with high-dose simvastatin.[Erratum appears in Am J Health Syst Pharm. 2003 Sep 1;60(17):1733]. American Journal of Health-System Pharmacy 2003;60:578-81. 35. Shepherd J, Kastelein JJP, Bittner V et al. Intensive lipid lowering with atorvastatin in patients with coronary heart disease and chronic kidney disease: the TNT (Treating to New Targets) study. Journal of the American College of Cardiology 2008;51:1448-54. 36. Heart Protection Study Collaborative G. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial.[Summary for patients in Curr Cardiol Rep. 2002 Nov;4(6):486-7; PMID: 12379169]. Lancet 2002;360:7-22. 37. Tonelli M, Isles C, Curhan GC et al. Effect of pravastatin on cardiovascular events in people with chronic kidney disease. Circulation 2004;110:1557-63. 38. Ridker PM, MacFadyen J, Cressman M, Glynn RJ. Efficacy of rosuvastatin among men and women with moderate chronic kidney disease and elevated high-sensitivity C-reactive protein: a secondary analysis from the JUPITER (Justification for the Use of Statins in Prevention-an Intervention Trial Evaluating Rosuvastatin) trial. Journal of the American College of Cardiology 2010;55:1266-73. 39. Baigent C, Landray MJ, Reith C et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 2011;377:2181-92. 40. Meara E, White C, Cutler DM. Trends in medical spending by age, 1963-2000. Health Aff (Millwood) 2004;23:176-83. 41. D. H. Smith GAN, C. M. Gullion, E.S. Johnson, D. Keith. Predicting Costs Of Care In Chronic Kidney Disease: The Role Of Comorbid Conditions. The Internet Journal of Nephrology 2007;4. 42. Kauf TL, Velazquez EJ, Crosslin DR et al. The cost of acute myocardial infarction in the new millennium: evidence from a multinational registry. Am Heart J 2006;151:206-12. 43. Tsevat J, Kuntz KM, Orav EJ, Weinstein MC, Sacks FM, Goldman L. Cost-effectiveness of pravastatin therapy for survivors of myocardial infarction with average cholesterol levels. Am Heart J 2001;141:727-34. 44. Samsa GP, Bian J, Lipscomb J, Matchar DB. Epidemiology of recurrent cerebral infarction: a medicare claims-based comparison of first and recurrent strokes on 2-year survival and cost. Stroke 1999;30:338-49. 45. Leibson CL, Hu T, Brown RD, Hass SL, OFallon WM, Whisnant JP. Utilization of acute care services in the year before and after first stroke: A population-based study. Neurology 1996;46:861-869. 46. Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke 1996;27:1459-66. 47. Drugs CRHBB. Statin Drugs to Treat High Cholesterol and Heart Disease. 2010. 48. Research Z. Prices for Pravastatin. March 7, 2012. 49. Services DoHaHRCfMaM. Physician Fee Schedule. 2011. 50. Fryback DG, Dasbach EJ, Klein R et al. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making 1993;13:89-102. 51. Gorodetskaya I, Zenios S, McCulloch CE et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int 2005;68:2801-8. 52. Tsevat J, Goldman L, Soukup JR et al. Stability of time-tradeoff utilities in survivors of myocardial infarction. Med Decis Making 1993;13:161-5. 53. Preiss D, Seshasai SRK, Welsh P et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA 2011;305:2556-64. 54. Glasser SP, Wadley V, Judd S et al. The association of statin use and statin type and cognitive performance: analysis of the reasons for geographic and racial differences in stroke (REGARDS) study. Clinical Cardiology 2010;33:280-8. 55. Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Affairs 2010;29:297-303. 56. Sullivan PW, Ghushchyan V. Preference-Based EQ-5D index scores for chronic conditions in the United States. Med Decis Making 2006;26:410-20. 57. Gregg EW, Gu Q, Cheng YJ, Narayan KMV, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000.[Summary for patients in Ann Intern Med. 2007 Aug 7;147(3):I10; PMID: 17577000]. Annals of Internal Medicine 2007;147:149-55. 58. Ekman M, Berg J, Wimo A, Jonsson L, McBurney C. Health utilities in mild cognitive impairment and dementia: a population study in Sweden. International Journal of Geriatric Psychiatry 2007;22:649-55.