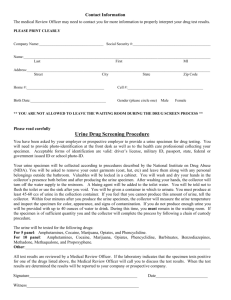
UA PPT Flashcards
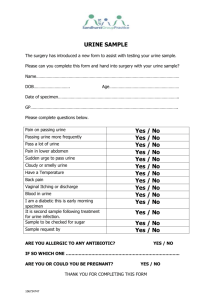
advertisement

UA PPT Flashcards 1) What are the agencies involved in developing guidelines for mandated safety policies? 2) What is the primary objective of biological safety? 3) How does a microorganism transmit? 4) What are the infectious agents? 5) What are the reservoirs of potentially harmful microorganisms? 6) What are the means of transmission for microorganisms? 7) What are the potential portal of entry of microorganisms? 8) What are examples of standard precautions? Centers for Disease Control and Prevention Occupational Health and Safety Administration Clinical Laboratory Standards Institute Preventing completion of the chain of infection Infectious agent, reservoir, portal of exit, means of transmission, portal of entry, susceptible host Bacteria, fungi, parasites, viruses Humans, animals, fomites Airborne, direct contact, droplet, vector, vehicle 9) Is handwashing a substitute for gloves? 10) What are the types of gloves? 11) What type of gloves if alternative for personnel with latex allergy? 12) What is the purpose of fluid-resistant lab coats? 13) How are the lab coats worn? 14) What are the types of face protection for PPE? Mucous membranes of the nose, mouth, and eyes Breaks in the skin Open wounds Hand hygiene Gloves Mouth, nose and eye protection Gown Patient-care equipment – disposal or sterilization Environmental control – clean and disinfect surfaces Linen – prevent exposure when handling Occupational health and bloodborne pathogens – no needle recapping Patient placement – Isolation Respiratory hygiene/cough etiquette – prevention of droplet and fomite transmission of respiratory pathogens No Sterile and nonsterile, powdered and nonpowdered, latex and nonlatex Nitrile or vinyl glove Protect skin and clothing Completely buttoned, gloves pulled over wrist cuffs Wear when working with specimens, remove when leaving lab Change when visibly soiled Discard disposable as biohazardous waste and nondisposable in designated laundry bins Goggles, full-face plastic shields, Plexiglas countertop shields 1 UA PPT Flashcards 15) Where does face protection as PPE help personnel? 16) Is it OK to centrifuge uncapped specimens? 17) What is the recommended foot protection? 18) What is the primary method of infection? 19) When do we sanitize our hands? 20) Who developed hand washing guidelines to be followed for correct hand washing? 21) Can urine be poured down the sink? 22) What are the examples of sharps? 23) Where are sharps disposed? 24) What are the steps that needs to be done for skin/eye chemical spill? 25) What is included in the chemical spill kit? 26) Is it OK to mouth pipet? 27) What is a chemical hygiene plan? 28) What information should an MSDS have? 29) What are possible radioactive hazard in labs? 30) What precautionary measures must be done for radioactive hazards? Splashes and aerosols caused by uncapping, pouring, transferring, and centrifuging No Closed-toed and covers the entire foot Hand contact CDC Before patient contact After gloves are removed Before leaving the work area At any time when hands have been knowingly contaminated Before going to designated break areas Before and after using bathroom facilities Yes Needles, lancets, broken glassware Puncture-resistant containers that are leak proof flush 15 minutes with water seek medical attention do not try to neutralize with other chemicals Protective apparel, nonreactive absorbent material, bags for disposal No Written plan required by OSHA that includes: appropriate work practices Standard operating procedures PPE Engineering controls, hoods, safety cabinets Employee training Medical consultation guidelines Physical and chemical characteristics Fire and explosion potential Reactivity potential Health hazards and emergency first aid procedures Methods for safe handling and disposal Primary routes of entry Exposure limits and carcinogenic potential Radiosotopes Symbol on doors Radiographers wear badges to measure exposure Pregnancy: avoid areas with this symbol 2 UA PPT Flashcards 31) How to avoid electrical hazards? 32) What to do in the event of electrical shock accident? 33) What must be done in the event of fire? 34) How do you operate a fire extinguisher? 35) What are the general precautions of physical hazards? 36) What is Quality Assessment? 37) What is Quality System? 38) What are the Quality Assessment Programs? 39) What are the Guidelines published by College of American Pathologists (CAP) and the CLSI to provide complete instructions for documentation? Avoid water and fluid contact Do not operate equipment with wet hands Observe for frayed cords, overloads; report Unplug and dry wet equipment Equipment grounded with three-prong plugs Do not touch person Remove electrical source Turn off circuit breaker Unplug equipment Move equipment using nonconductive items such as wood or glass. Rescue: anyone in danger Alarm: activate Contain: close affected area doors Extinguish/Evacuate: if possible, or exit Pull pin Aim at base of fire Squeeze handles Sweep nozzle side to side Avoid running in rooms and hallways Watch for wet floors Bend the knees when lifting heavy objects Keep long hair pulled back Avoid dangling jewelry Maintain a clean, organized work area Wear supportive, closed-toe shoes The overall process of guaranteeing quality patient care. The laboratory’s policies, processes, procedures, and resources needed to achieve quality testing. • Testing controls – Quality control • Preexamination variables – Specimen collection, handling, and storage • Examination variables – Reagent and test performance, instrument calibration and maintenance, personnel requirements, and technical competence • Postexamination variables – Reporting of results and interpretation Procedure manuals Internal and external quality control Standardization and equipment maintenance Proficiency testing and record-keeping Safety programs Training, education, competency assessment Scheduled, documented review processes Required by accrediting agencies 3 UA PPT Flashcards 40) Name the 6 Accrediting Agencies? 41) T or F, Urinalysis Manual must be available in work area? 42) What should a Urinalysis Procedure Manual must include? 43) How often the current methods must be reviewed? 44) What must be done when there is a change in the procedure manual? 45) Who must be notified of changes? 46) What are the variables before testing? 47) What is Turnaround Time (TAT) 48) What information should requisition and computerized entry forms must have? Joint Commission (JC) College of American Pathologists (CAP) American Association of Blood Banks (AABB) American Osteopathic Association (AOA) American Society of Histocompatibility and Immunogenetics (ASHI) Commission on Laboratory Assessment (COLA) True Principle or purpose of the test Clinical significance Patient preparation Specimen type and method of collection Specimen acceptability and criteria for rejection Reagents, standards, and controls Instrument calibration and maintenance protocols and schedules Step-by-step procedure, calculations Frequency and tolerance limits for controls and corrective actions Reference values and critical values Interpretation of results Specific procedure notes Limitations of the method Method validation Confirmatory testing Recording of results References Effective date, author, and review schedule Annualy Reviewed, referenced, and signed by a person with designated authority All personnel must be notified. Ordering of tests Patient preparation Specimen collection Specimen handling, transport, and storage Is the amount of time required from when a test is ordered by the health-care provider until the results are reported to the health-care provider. • Patient identification information o Name, sex, age, date of birth, hospital ID number • Test requested • Type of urine specimen to be obtained (voided, clean catch, catheterized) 4 UA PPT Flashcards • • 49) What is the acceptability of a specimen? 50) What reasons can a specimen are rejected? 51) What processes directly affect the testing of specimens? 52) What information reagents must have? 53) What QC must instrumentation and Equipment must be followed? 54) What is the procedure for Testing? Requested date and time of collection Actual collection information (time, storage/transport condition) • Received and tested time Matching patient information on specimen and requisition Properly labeled specimen Timely transport or refrigeration Adequate amount of specimen Noncontaminated specimen Tightly closed container Patient misidentification Wrong test ordered Incorrect urine specimen type collected Insufficient urine volume Delayed transport of urine to laboratory Incorrect storage or preservation of urine Reagents Instrumentation and equipment Testing procedure QC Preventive maintenance Access to procedure manuals Competency of personnel performing the tests Manufacturer, name, and chemical formula Instructions for preparation: Type of water used in preparation Clinical Laboratory Reagent Water (CLRW) Storage requirements Procedures for reagent quality control Label with date of opening or preparation Check reagent strips daily or each shift and when a new bottle is opened Safety and health precautions Operation, calibration, limitations, dilution procedures, recording Calibration and control of refractometers, osmometers, reagent strip readers Temperatures of refrigerators and water baths must be recorded daily Calibration and disinfection of centrifuges Prepare a routine preventive maintenance schedule Document all routine and nonroutine maintenance Specimen preparation: time and speed of centrifugation Specimen and reagent stability Calculation formulas 5 UA PPT Flashcards 55) What is Quality Control (QC)? 56) What does QC ensures? 57) What is External QC? 58) Within an external QC the verification of accuracy and precision can also calculate: 59) When should Corrective Actions be taken? 60) Corrective Actions must be ________ 61) What is an Internal QC? 62) What is achieved when an Internal and Procedural QC is done? 63) What is achieved in an Electronic Internal QC? 64) What is achieved in Proficiency Testing/External Quality Assessment (PT/EQA)? 65) What is the testing of unknown samples provided by an external agency? 66) What actions follow the completion of Proficiency Testing/External Quality Assessment? 67) How is the evaluation and comparison of a PT/EQA done? 68) What is the final step of a PT/EQA? Health and safety precautions Sources of error and interference Clinical situations influencing test, alternate procedures Helpful hints Turnaround time for STATs The materials, procedures, and techniques that monitor the accuracy, precision, and reliability of a laboratory test. It ensures that acceptable standards are met during the process of patient testing. Patient test results not reported until the QC is verified. • Verifies accuracy and precision such as: – Exposed to the same condition as a patient sample – Medically significant – Run two levels of control material – Record date of opening, manufacturer’s lot number, expiration date each time control is run – Same person running controls must run patient samples – Free of communicable disease (HIV, Hepatitis C, Hepatitis B) The mean, standard deviation, coefficient of variation and range. When the control values are outside the tolerance limits. Documented The internal monitoring included in the test system Monitors addition of patient specimen and reagents, instrument and reagent interaction and test completion. Verifies the functional ability of electrical components of instruments in place of liquid control medium. Unbiased validation of the quality of patient test results Proficiency Testing/External Quality Assessment (PT/EQA) The accuracy is evaluated and compared with other laboratories using the same method of analysis. The vendor statistically rates answers from all participating labs and returns the report to the lab director. Corrective actions performed and documented. 6 UA PPT Flashcards 69) What is included in a Personnel Assessment? 70) What is learned in Document training? 71) What must be available in Facilities? 72) The Facilities must have: 73) What must always be followed within the facility? 74) What are Post-Examination Variables? 75) Regarding Post-Examination Variables, what must be used in order to minimize health-care provider confusion? 76) What are the most common type of Post-Examination Variable? 77) What types of problems occur when using Electronic Transmissions? 78) What must be done in order to correct erroneous results in a timely matter? 79) What must be done when telephoning results? 80) Why should written procedures be available? 81) When Interpreting results you must include _______ and _______ of tests in the procedure manual. 82) In order to interpret results correctly a list of what type of substances must be documented within the manual? 83) When Interpreting results a welldocumented QA program will: 84) What is the importance of Urinalysis? 85) What is the CLSI definition of Urinalysis? 86) What are the reasons for performing Urinalysis on patients? 87) The ultrafiltrate of plasma is used to form _______. 88) What is an average daily urine output? 89) Urine consists of ____% water and ____% solutes. 90) What is the major organic solute in urine? Education and training, continuing education, competency assessment, and performance appraisals. The creation of Checklist of procedures The current reference materials A safe working area with adequate space. Standard Precautions Processes that affect the reporting of results and correct interpretation of data. The use of Standardized reporting formats which include reference ranges. Electronic Transmissions Autoverification is often programmed into many laboratory analyzers Do not erase original result from chart and document the errors. Confirm that the results are being reported to the appropriate person For reporting of critical values Specificity; Sensitivity Interfering substances Ensure quality test results and patient care Urine contains information, which can be obtained by inexpensive laboratory tests, to assess many metabolic functions. The testing of urine with procedures commonly performed in an expeditious, reliable, safe, and costeffective manner. The aiding of disease diagnosis, screening for asymptomatic diseases, and monitor of disease progress and therapy effectiveness. urine 1200 mL 95%; 5% Urea 7 UA PPT Flashcards 91) What consists of the inorganic solutes in urine? 92) The identification of these components identifies a fluid as urine. 93) The identification of these substances within urine increases the indication of disease. 94) The Urine volume is determined by: 95) What may influence the volume of urine? 96) What is the usual daily volume of urine? 97) What is the normal range of urine volume? 98) A decrease in Urine output 99) What is the definition of Anuria? 100) What is the definition of Nocturia? 101) What are the components of Polyuria? 102) Patients with Diabetes Mellitus who are experiencing Polyuria will have: 103) Paitents with Diabetes Mellitus who are experiencing Polyuria will also exhibit: 104) Patients with Diabetes Mellitus will have urine that appears: 105) Patients with Diabetes Insipidus who are experiencing Polyuria will have: 106) The urine of a patient with Diabetes Insipidus will appear: 107) Patients with Diabetes Insipidus will also exhibit: 108) What information is included on a specimen label? 109) What additional information is included on a specimen label? 110) Where must the specimen label be placed? 111) What must accompany the specimen/ 112) What must be stamped on the requisition form? 113) What information must be on the requisition form? 114) A specimen is rejected if: 115) A specimen is rejected if: 116) A specimen is rejected if: 117) A specimen is rejected if: Chloride, sodium and potassium Urea and Chloride Cells, casts, crystals, mucus, and bacteria The body’s state of hyradation Fluid intake, nonrenal fluid loss, antidiuretic hormone (ADH) variations, excretion of large amounts of dissolved solids (e.g., glucose) 1200-1500 mL 600-2000 mL Oliguria The cessation of urine flow Increased urine excretion at night Greater than 2.5 L of urine excreted a day. Increased volume caused by need to excrete the excess glucose not reabsorbed from the ultrafiltrate. Polydipsia Dilute with a high specific gravity Decreased production or function of antiduretic hormone (ADH) causing decreased reabsorption of water from ultrafiltrate. Dilute with low specific gravity. Polydipsia Patient’s name, ID number, date, time Age, location, health-care provider’s name. on the container not the lid. A requisition form Time of receipt Type of specimen, interfering medications The specimen is not labeled There is non-matching labels and requisition forms The exterior of the container is contaminated The Specimen is sent an insufficient quantity 8 UA PPT Flashcards 118) A specimen is rejected if: 119) In order to insure the proper quality of specimen a laboratory must include: 120) In order to have the correct test results the urine specimen must be tested within what amount of time? 121) What must be done in order to keep the integrity of the specimen if the testing is delayed? 122) What causes the most problems when trying to keep the integrity of a urine specimen? 123) In order to keep the integrity of a urine specimen the sample must be refrigerated at __°C to __°C 124) What is the ideal chemical preservative of a urine specimen? 125) The chemical preservative bactericidal: 126) What must be true in order to use a commercial transport tube? 127) What influences the composition of a urine specimen? 128) What influences the composition of a urine specimen? 129) What is the most common type of Specimen received? 130) When may Random Specimens be collected? 131) What must be recorded when collecting Random specimens? 132) What may alter the results of a Random Specimen? 133) What is the most ideal type of specimen for screening? 134) Why are First morning specimen’s the most ideal for screening? 135) Why are First Morning Specimens used? 136) Why is a First Morning Specimen more better for testing than a random specimen? 137) How is a first morning specimen collected? 138) What type of specimen is collected after the first morning specimen? The Specimen is improperly transported Written policies for rejection of specimens Within 2 hours of collection Refrigerate or chemically preserve the specimen Bacterial multiplication 2; 8 Bactericidal Inhibits urease and preserves formed elements The transport tube must be compatible with the tests The patient’s metabolic state and the timing and procedure used for collection Time, length, and method of collection and the patient’s dietary and medicinal intake Random Specimen Random Specimens may be collected at any time Collection time must be recorded Dietary intake and physical activity First Morning Specimen The patient is in a basal state For orthostatic protein confirmation, and urine pregnancy tests The urine is more concentrated Upon rising and delivered to the lab within 2 hours Fasting Specimen 9 UA PPT Flashcards 139) This type of urine specimen does not contain metabolites 140) What type of specimen is recommended for glucose monitoring 141) What type of specimen will produce accurate quantitative results? 142) What are good diurnal variation solutes? 143) True or False The patient must remain adequately hydrated during short collection period. 144) True or False The patient must be instructed on the procedure for collecting a timed specimen. 145) Concentration of a substance in a particular period must be calculated from? 146) 24-hour specimen must be thoroughly __________ and the _________ accurately measured and recorded 147) Multiple containers of the same collection must be _______ and _______ thoroughly. 148) True or False Additives should not interfere with the tests to be performed. 149) 24-hour specimens are needed for? 150) Substances with consistent levels can be measured with what type of specimen? 151) What is a critical factor for accurate results? 152) What is the procedure for a 2-hour postprandial specimen? 153) True or False Glucose tolerance specimens are collected at the same intervals as the blood samples Fasting Specimen Fasting Specimen A carefully timed specimen Catecholamines and electrolytes True True The urine volume produced during that time Mixed, volume Combined, mixed True Quantitative results, measuring substances with diurnal variation, and substances that vary with meals, activity, and body metabolism Shorter timed specimens Accurate timing 1. Patient voids before eating routine meal 2. Eats meal 3. Collects next specimen 2 hours after finishing meal 4. Monitors insulin therapy 5. Results can be compared with fasting urine specimen and blood test results True 10 UA PPT Flashcards 154) What type of specimen is used to correlate renal threshold with patient’s ability to metabolize glucose? 155) What type of specimen is a sterile specimen collected from the bladder with a hollow tube? 156) What is the most common test for a catheterized specimen? 157) What is an alternative to a catheterized specimen? 158) True or False Catheterized method is less traumatic than midstream clean-catch specimen. 159) What type of specimen is less contaminated than routine collection? 160) For midstream clean-catch specimen, you must provide the patient with mild _________ _________, a container, and instruction. 161) True or False For a midstream clean-catch specimen, you should not touch or contaminate inside of container. 162) What type of specimen is completely free of contamination for culture ad cytology? 163) What type of specimen is collected by external introduction of needle for aspiration from the bladder? 164) Which specimen is similar to midstream clean-catch? 165) How many containers are collected for a prostatitis specimen? 166) For a prostatitis specimen, what sample is collected in container 1? 167) For a prostatitis specimen, what sample is collected in container 2? 168) What needs to be done before the third sample of a prostatitis specimen is collected? 169) Why is the prostate massaged before the third collection of a prostatitis specimen? 170) What sample is collected in container 3 of a prostatitis specimen? Glucose tolerance specimen Catheterized specimens Bacterial culture A midstream clean-catch specimen False Midstream clean-catch specimen Cleaning material True Suprapubic aspiration Suprapubic aspiration Prostatitis specimen 3 First urine passed Midstream urine Massage prostate to obtain prostatic fluid To obtain prostatic fluid The remaining urine and prostatic fluid 11 UA PPT Flashcards 171) Which containers of a prostatitis specimen are examined microscopically? 172) What do these lab results indicate: Higher WBC/hpf count in specimen 3 than specimen 1; bacterial count in specimen 3 is 10 times higher than in specimen 1 173) Prostatitis specimen 2 is a control for? 174) A positive culture in specimen 2 invalidates what? 175) Why does a positive specimen 2 invalidate a positive specimen 3? 176) What specimens are collected for a pre- and postmassage test? 177) What is indicated by a quantitative culture result in the second glass that is 10 times higher than specimen 1? 178) How is a pediatric specimen collected? 179) True or False Clean-catch method with a sterile bag can be used for pediatric specimens. 180) Bags with tubes to a larger container are available for what type of specimens? 181) What must be documented for a drug collection? 182) Chain of custody for a drug specimen involves: 183) Drug specimens are free of: 184) What always accompanies drug specimens? 185) Drug specimen must withstand ________? 186) True or False A photo ID of the urine donor does not need to be collected 187) There is no unauthorized access to what type of specimen? 188) Witnessed versus unwitnessed collection is determined by? 189) True or False For witnessed and unwitnessed collections, the specimens must be handed immediately to the collector. 1 and 3 Prostatic infection Bladder or kidney infection A positive culture in specimen 3 Because it cannot differentiate urinary tract infection from prostate infection First a midstream clean catch specimen, second a postmassage specimen Prostatitis In a soft, clear, plastic bag, with hypoallergenic tape applied to genital area True Timed specimens Proper collection, labeling and handling Documentation from the time of specimen collection until the time of receipt of laboratory results Substitution, adulteration, or dilution Standardized form Legal scrutiny False Drug specimen Test orderer True 12 UA PPT Flashcards 190) The temperature of a drug specimen must be taken within ____ minutes to confirm the specimen was not adulterated. 191) What temperature range should the urine specimen be in? 192) What should you do if the specimen is not within normal temperature range? 193) The labeling, packaging, and transport of a drug specimen should follow? 194) What is the functional unit of the kidney? 195) How many nephrons are in each kidney? 196) What type of nephron makes up 85% of the nephrons, the loop remains within the cortex of the nephron, is responsible for removal of waste products and reabsorption of nutrients? 197) What type of nephron has longer loops of Henle, extends deep into the nephron medulla, and is responsible for urine concentration? 198) What type of functions are controlled in the nephron and include the following: renal blood flow, glomerular filtration, tubular reabsorption, and tubular secretion. 199) Renal blood flow: Renal artery, afferent arteriole, ______, efferent arteriole, _______, vasa recta/loops of Henle, peritubular capillaries/distal convoluted tubule, _____. 200) What supplies blood to the kidneys? 201) What carries the blood leaving the glomerulus? 202) What part of the nephron is adjacent to loops of Henle, acts as an osmotic gradient, and exhibits major exchange of water and salts? 203) Based on an average body size of 1.73m2 of surface, the total renal blood flow is approximately? 204) Renal plasma flow = 4 32.5oC to 37.7oC The temperature should be reported immediately, and another specimen collected ASAP. The urine color should also be inspected for possible contamination. Laboratory instructions. Nephron 1 to 1.5 million Cortical Juxtamedullary Renal functions Glomerulus, peritubular capillaries/proximal convoluted tubule, renal vein Afferent arteriole Efferent arteriole Vasa recta 1200mL/min 600-700mL/min 13 UA PPT Flashcards 205) True or False Correction for variance in body surface area must be calculated. 206) How many capillary lobes are in the glomerulus? 207) Where is the glomerulus located? 208) What type of filtration occurs in the glomerulus? 209) Cellular structure, hydrostatic and oncotic pressure, and renin-angiotensinaldosterone system are all factors of? 210) What 3 cellular layers make up the glomerulus? 211) The endothelial cells of the capillaries in the glomerulus differ from other capillaries because? 212) True or False The pores allow large molecules to pass through. 213) Does the basement membrane restrict or allow large molecules to pass through? 214) The inner layer of Bowman’s capsule contains what type of cells? 215) What repels molecules with a positive charge? 216) Give an example of a molecule small enough to pass through the three layers of the barrier. 217) The juxtaglomerular apparatus is responsible for? 218) How does the juxtaglomerular apparatus maintain consistent glomerular pressure? 219) In order to prevent decrecreased glomerular blood flow when the systemic blood pressure is low, the juxtaglomerular apparatus will? 220) In order to prevent overfiltration and glomerular damage when the systemic blood pressure is high, the juxtaglomerular apparatus will? 221) What does RAAS stand for? 222) The RAAS controls? 223) The RAAS reacts to what kind of changes? True 8 Bowman’s capsule Nonselective Glomerular filtration Capillary wall, basement membrane, bowman’s capsule inner layer They contain pores False Restrict Podocytes Shield of negativity Albumin Maintaining consistent glomerular pressure By regulating the arteriole size Dilate the afferent arteriole and constrict the efferent arteriole Constrict the afferent arteriole Renin-Angiotensin-Aldosterone System The regulation of blood flow to and within the glomerulus Changes in blood pressure and plasma sodium 14 UA PPT Flashcards 224) Blood pressure and plasma sodium are monitored by? 225) The juxtaglomerular apparatus contains different cells in each arteriole, list the cells and which arteriole they are found in. 226) In response to blood pressure changes, the macula densa initiates? 227) What six factors are associated with RAAS Cascade? Juxtaglomerular apparatus 228) These functions are related to _______? Dilates afferent arteriole Constricts efferent arteriole Stimulates sodium reabsorption in proximal convoluted tubule (PCT) Triggers release of aldosterone a. Reabsorption of sodium in distal convoluted tubule (DCT) and collecting duct (CD) b. Increase in potassium excretion Triggers release of antidiuretic hormone (ADH) c. Stimulates water reabsorption in CD Angiotensin II 229) What is the normal filtrate for Glomerular? A. 120 mL/min of filtrate B. 100 mL/min of filtrate C. 80 mL/min of filtrate D. 140 mL/min of filtrate 230) Ultrafiltrate of plasma, Same composition minus plasma proteins, protein-bound substances, and cells are referring to _______Filtrate? 231) What is the ultrafiltrate specific gravity for Gromerular? A. 10.10 B. 1.010 C. 10.15 D. 10.09 A. 120/mL min of filtrate Juxtaglomerular cells – afferent arteriole Macula densa – efferent arteriole RAAS • • • • • • Renin secreted by juxtaglomerular cells Angiotensinogen: blood substance Angiotensin 1: passes through lungs Angiotensin-converting enzyme (ACE) Angiotensin II Aldosterone Glomerular B. 1.010 15 UA PPT Flashcards 232) Tubular reabsorption starts when the plasma ultrafiltrate enters the proximal convoluted tubule? True or False 233) Active transport consists of these things? True of False Carrier proteins and cellular energy needed for transport back to blood, Glucose, salts (Na is highest), amino acids in proximal convoluted tubule, Chloride in ascending loop of Henle, Sodium in distal convoluted tubule. 234) Referring to tubular re-absorption, these functions occur during what transport? Controlled by the differences in substance concentration gradients on sides of a membrane, Water reabsorption occurs throughout the nephron, Exception is ascending loop of Henle, Accompanies high amount of sodium reabsorption in PCT, Urea in PCT and ascending loop of Henle, Sodium in the ascending loop of Henle. A. Active B. Passive 235) Plasma concentration of a substance that is normally completely reabsorbed reaches an abnormally high level is call________ Reabsorptive Capacity (Tm). 236) Referring to maximal reabosorptive capacity, Renal threshold includes: Normally reabsorbed substance appears in urine, Glucose threshold: 160 to 180 mg/dL, Threshold distinguishes excess filtration from tubular damage. True or False? 237) Plasma level causing active transport to cease is referred to as _______ _______? 238) In regards to tubular concentration, Passive reabsorption of water into the high osmotic gradient of the renal medulla is referred to as? A. Ascending loop Henle B. Descending loop Henle C. All the above True True B. Passive Maximal True Renal Threshold B. Descending 16 UA PPT Flashcards 239) Chloride actively reabsorbed, Sodium passively reabsorbed and walls are impermeable to water are referred to ______ loop Henle? 240) Referring to tubular concentration, what are these functions associated with? a. Maintains concentration in the medulla b. Medulla is diluted by the water from the descending loop c. Reconcentrated by sodium and chloride from the filtrate in the ascending loop 241) Aldosterone-controlled Na reabsorption if needed by body is associated with DCT? True or False 242) Water reabsorption controlled by ADH in response to body hydration, Osmotic gradient in the medulla, Vasopressin (ADH) is associated with? 243) Controls permeability of DCT and CT walls to water, Amount of ADH produced by hypothalamus determines permeability is associated with? 244) The chemical balance in the body is actually the final determinant of urine volume and concentration is associated with? 245) Final filtrate concentration, ADH and The chemical balance in the body is actually the final determinant of urine volume and concentration is associated with? 246) Body Hydration = ↓ADH = ↑Urine Volume ↓Body Hydration = ↑ADH = ↓Urine Volume What chart is this referring to? 247) Referring to tubular secretion, Secretion = blood peritubular capillaries to filtrate. True or False 248) Contrast to reabsorption = filtrate to blood is associated to Secretion? True or False Ascending Loop Henle Countercurrent mechanism True Final filtrate concentration ADH Collecting Duct Concentration Collecting Duct Concentration Diagram of ADH Regulation True True 17 UA PPT Flashcards 249) Eliminate nonfiltered wastes are associated to: Protein-bound substances, Regulate acid-base balance? (Secrete H+ ions to return filtered buffers to the blood, Excrete excess H+ ions). True or False 250) Normal blood pH is 7.4. True or False 251) Dietary intake and Body metabolism are associated with Acid-Base Balance. True or False 252) Secretion of hydrogen ions (H+) into filtrate, 100% of bicarbonate reabsorption and PCT are associated with Bicarbonate (HCO3) returned to blood. True or False 253) Rates determined by the acid-base balance in the body are associated with ________ balance. 254) Metabolic acidosis and Renal tubular acidosis are associated with _________ causes. 255) Referring to Renal functions tests, Tests evaluate: Glomerular filtration, Tubular reabsorption, Tubular secretion, Renal blood flow. True or False a. Measure rate at which the kidneys can remove a filterable substance from the blood b. Substance analyzed cannot be reabsorbed or secreted by the tubules c. Stability of substance during a long urine collection period d. Consistency of plasma level e. Availability to the body f. Availability of tests to measure the substance 256) These clearance tests are associated with? 257) What 6 things are associated with measuring GFR? True True True True Acid-base Disruptive causes True Glomerular Filtration Creatinine Beta2 microglobulin Cystatin C Radioisotopes Exogenous procedure Requires an infused substance Endogenous procedure 18 UA PPT Flashcards 258) Substance already present in the body and Method of choice are related to Endogenous procedure? True or False 259) Exogenous procedure requires an infused substance. True or False 260) Creatinine is current routine test for what substance? 261) Referring to creatinine clearance, Waste product of muscle destruction found at relatively constant plasma level and Automated chemical tests, calculate an eGFR utilizing serum creatinine and do not require urine testing is correlated to? 262) Tubular secretion increases with high blood creatinine levels Gentamicin, cephalosporins, and cimetidine inhibit tubular secretion Bacteria break down creatinine if urine is stored at room temperature Diet heavy in meat during timed collection increases urine creatinine Not reliable with muscle-wasting diseases Accurate results depend on the accurate completing of a 24-hour collection It must be corrected for smaller/larger body surface area Are these tests an advantages or disadvantages? 263) Greatest error is improperly timed urine specimen Principle: to determine the amount of creatinine (mL) completely cleared from the plasma during 1 minute Report in milliliters per minute This is referred to as the glomerular filtration rate (GFR) These factors are associated with what? 264) Report in milliliters per minute is correlated to procedure. True or False 265) This is referred to as the glomerular filtration rate (GFR) in procedure. True or False a. Urine volume in milliliters per minute (V) b. Urine creatinine in mg/dL (U) c. Plasma creatinine in mg/dL (P) True True Endogenous Advantages Disadvantages Procedure True True Required 19 UA PPT Flashcards d. Calculation of urine volume 266) These associated with _______ measurements. 267) Milliliters in specimen/minutes collected are associated with calculation of urine volume. True or False 268) Referring to procedure, some examples are: 2-hour specimen volume = 240 mL, 2 × 60 = 120 min, 240/120 = 2 mL/min. True or False 269) What is the Standard Clearance Formula? 270) What are the normal values of creatinine for both men & women? 271) How is creatinine produced? 272) Normal creatinine values are based on what? 273) True or False: Normal reference range of plasma creatinine is 0.5 to 1.5 mg/dL 274) Which variables does eGFR modification of diet in renal disease (MDRD) use? 275) What's the advantage of the MDRD formula? 276) What's the sample formula? 277) Cystatin C is produced by___ filtered by __ and absorbed by __ 278) Beta microglobulin is removed from the plasma by __ and measured by___ 279) Beta microglobulin is sensitive indicator of what? 280) What is an exogenous procedure that measures plasma disappearance of an injected isotope and provides simultaneous visualization of the kidneys? 281) Tubular Reabsorption Tests are a good indicator of? 282) What's necessary for accurate results of tubular reabsorption tests? 283) What do tubular reabsorption tests measure? 284) How is renal concentration assessed? 285) Specific gravity includes? 286) Name the colligative properties True True CP = UV and C = UV/P 107 to 139 mL/min for men 87 to 107 mL/min for women As a result of muscle destruction Size, the larger the person, the more creatinine is produced TRUE Serum BUN, serum albumin, and ethnicity Without weight all calculations are available from the lab computer. MDRD-IDMS All nucleated cells, glomerulus, renal tubules Kidneys, enzyme immunoassay Decrease in GFR Radioisotopes Early Renal disease Control of fluid intake Renal Concentrating Ability By Osmolarity Number and Size of Molecules Freezing point, boiling point, osmotic pressure and vapor pressure 20 UA PPT Flashcards 287) Describe what happens in Osmometry? 288) What's the primary urine method? 289) In Renal Concentration- Osmolality, urine depends on: 290) Controlled fluid intake has a ratio of: 291) Vapor pressure osmometers measure? 292) What are the technical factors for vapor pressure osmometers? 293) What's the clinical significance: evaluating renal concentrating ability, monitoring course of renal disease, monitoring fluid & electrolyte therapy, differential diagnosis of hyponatremia & hypernatremia, evaluating secretion of and response to ADH? 294) What happens in Diabetes Insipidus? 295) What happens after ADH injection? 296) What's free water clearance? 297) What determines if enough water is excreted to remove wastes & the kidney's response to body hydration? 298) True or False: Ultrafiltrate has a different osmolarity as plasma 299) In Tubular Secretion Renal Blood Flow, to measure secretion, the blood flow must be adequate 300) To measure blood flow, the secretion must be adequate 301) The tests are unrelated, because secretion is independent on renal blood flow 302) What is a test for renal blood flow? 303) PAH is secreted in___ , loosely bound to __ and removed from the __ 304) The PAH test normal values are based on? 305) What's the average renal blood flow? 306) What percentage does not come in contact with functional renal tissue? 307) Titratable Acidity/Urine Ammonia are tests for tubular secretion of? Measured sample is supercooled & vibrated to form crystals, heat of fusion raises temperature to freezing point, probe measures freezing point Freezing point osmometers Fluid intake or exercise 3:1 Dew point (temperature at which water vapor condenses to a liquid) Lipemic serum, Lactic acid, Volatile/ethanol All of the above Decreased ADH production, inability of tubules to respond to ADH 1:1 ratio= no ADH receptors in CD, 3:1 ratio = inability to produce ADH Expands serum: urine ratio. Osmolar clearance done first with water deprivation, timed urine & serum Free water clearance FALSE TRUE TRUE FALSE P-Aminohippuric Acid (PAH) Proximal convoluted tubule, plasma proteins, blood Normal Hct 1200 mL/min About 8% H+ and NH4+ 21 UA PPT Flashcards 308) What does physical examination of urine include? 309) What do results provide? 310) Which disorders: Glomerular bleeding, liver disease, inborn errors of metabolism, urinary tract infection, or renal tubular function does physical characteristics of urine provide information about? 311) What is the color of urine? 312) What are normal variations not caused by: ingested materials, pathologic conditions, physical activity, hereditary disorders, or normal metabolic functions? 313) Abnormal variations are caused by physical activity, infection, or bleeding? 314) What are the consistent common terminologies used within institutions to describe normal urine color? 315) _____ is a pigment causing the yellow color of urine. 316) Urochrome normally excretes at a _____ rate. 317) Does urochrome increase or decrease in thyroid disease and fasting states? 318) Does urochrome increase or decrease when urine specimen sits at room temperature? 319) True or False: Urochrome provides estimate of body hydration. 320) True or False: Uroerythrin and urobilin pigments cause color change in older specimens. 321) _____ is a pink pigment that attaches to amorphous urates which are formed in refrigerated specimens. 322) _____ is an oxidation prduct of normal urinary constituent urobilinogen which yeilds an orange-brown color in older specimens. 323) True or False: The following are all common abnormal colors of urine: dark yellow/amber/orange red/pink/brown brown/black, blue/green Color, clarity, and specific gravity Preliminary information, correlation with other chemical and microscopic results All of the above Ranges from colorless to black Hereditary disorders Infection and bleeding pale yellow, yellow, dark yellow Urochrome constant increase increase True True Uroerythrin Urobilin True 22 UA PPT Flashcards 324) True or False: Dark yellow, amber, or orange urine may not always signify normal concentrated urine but can be caused by the presence of the abnormal pigment bilirubin. 325) _____ in urine indicates possible hepatitis virus present. 326) Bilirubin produces what color foam when shaken? 327) Normal urine produces small amount of white foam caused by _____. 328) Photooxidation of large amounts of urobilinogen produces what color urine? 329) Photooxidation of bilirubin to biliverdin produces what color urine? 330) True or False: Phenazopyridine (pyridium) or Azo-Gantrisin for urinary tract infection produces thick orange pigment and yellow foam (no bilirubin). 331) _____ is common cause of red urine. 332) True or False: Red is the usual color that blood produces in urine, but the color may range from pink to brown. 333) RBCs remaining in acidic urine for several hours produce what color urine due to the oxidation of hemoglobin to methemoglobin. 334) A fresh brown urine containing blood may indicate what? 335) Cloudy red urine indicates the presence of what? 336) Clear red urine indicates the presence of what two substances? 337) _____ resulting from the in vivo lysis of RBCs, patient’s plasma will be red. 338) Breakdown of skeletal muscle produces _____, patient’s plasma will be clear. 339) Urine specimens containing _____ may appear as a port wine color resulting from the oxidation of porphobilinogen to porphyrins. 340) True or False: Nonpathogenic causes of red urine include menstrual contamination, ingestion of highly pigmented foods, and medications. True Bilirubin yellow protein yellow-orange yellow-green True Blood True brown glomerular bleeding RBCs hemoglobin and myoglobin Hemoglobin myoglobin porphyrins True 23 UA PPT Flashcards 341) In genetically susceptible people, eating fresh beets causes a red color in _____ urine. 342) Ingestion of blackberries can produce a red color in _____ urine. 343) True or False: Additional testing is recommended for urine specimens that turn black after standing at room temperature and test negative for blood. 344) _____ is an oxidation product of the melanogen which is produced in excess when a malignant melanoma is present. 345) Homogentisic acid yields a black color in alkaline urine from persons with the inborn-error of metabolism, called _____. 346) True or False: Medications producing brown or black urine includes levodopa, phenol derivatives, and flagyl. 347) True or False: Pathogenic causes of blue/green urine color are limited to bacterial infections, including urinary tract infection by Pseudomonas species and intestinal tract infections resulting in increased urinary indican. 348) A _____ staining may occur in catheter bags and is caused by the presence of indican in the urine or a bacterial infection, frequently caused by Klebsiella or Providencia species 349) IV phenol medications causes _____ urine includes Clorets medications: Robaxin, methylene blue, Elavil (blue). 350) True or False: Color and clarity produces include: Use a well-mixed specimen View through a clear container View against a white background Maintain adequate room lighting Evaluate a consistent volume of specimen Determine color and clarity 351) _____ refers to the transparency or turbidity of a urine specimen. 352) What are the common terminologies used to report clarity of urine? alkaline acidic True Melanin alkaptonuria True True purple green True Clarity clear, hazy, cloudy, turbid, milky 24 UA PPT Flashcards 353) True or False: Clarity of urine can be determined by visual examination or automated turbidity readings. 354) Fresh clean-catch urine is normally _____. 355) Urine clarity reported as no visible particulates and transparent is known as? 356) Urine clarity reported as few particulates and print easily seen through urine is known as? 357) Urine clarity reported as many particulates and print blurred through urine is known as? 358) Urine clarity reported as print cannot be seen through urine is known as? 359) Urine clarity reported as may precipitate or be clotted is known as? 360) The following are considered pathologic or nonpathologic turbidity: hazy female specimens with squamous epithelial cells and mucus bacterial growth in nonpreserved specimens refrigerated specimens with precipitated amorphous phosphates (white) and urates (pink) contamination of fecal, talc, semen, vaginal creams, IV contrast media 361) The following are considered pathologic or nonpathologic turbidity: RBCs, WBCs, bacteria nonsquamous epithelial cells, yeast, abnormal crystals, lymph fluid, lipids extent of turbidity should correspond to the amount of material observed in the microscopic examination clarity is one of the criteria considered in determining the necessity of performing a microscopic examination 362) What evaluates urine concentration and determines if specimen is concentrated enough to provide reliable screening results? 363) What is defined as the density of a solution compared with the density of an equal volume of distilled water at the True clear clear hazy cloudy turbid milky nonpathologic pathologic specific gravity specific gravity 25 UA PPT Flashcards same temperature? 364) Specific gravity of 1.010 is called _____. 365) Specific gravity lower than 1.010 is called _____. 366) Specific gravity higher than 1.010 is called _____. 367) _____ measures velocity of light in air versus velocity of light in a solution. 368) Concentration changes the _____ and angle at which the light passes through the solution. 369) _____ in the refractometer determines the angle that light is passing through the urine and converts angle to calibrated viewing scale. 370) What are two advantages of refractometer? 371) For each gram of _____ present, 0.003 must be subtracted from specific gravity reading. 372) For each gram of _____ present, 0.004 must be subtracted from specific gravity reading. 373) True or False: Protein or glucose concentration can be determined from the chemical reagent strip tests. 374) A specimen containing 1 g/dL protein and 1 g/dL glucose has a specific gravity reading of 1.030. Calculate the corrected reading. 375) True or False: The methodology of refractometer are as follows: place one or two drops of urine on prism focus light source and read scale wipe off prism between specimens 376) Refractometer calibration of distilled water should read _____. 377) Refractometer calibration of 5% _____ should read 1.022 ± 0.001. 378) Refractometer calibration of 9% _____ should read 1.034 ± 0.001. isosthenuric hyposthenuric hypersthenuric Refractometer velocity Prisms Temperature compensation is not needed. Only small volume of specimen is needed (1-2 drops). protein glucose True 1.030 – 0.003 (protein) – 0.004 (glucose) = 1.023 True 1.000 NaCl Sucrose 26 UA PPT Flashcards 379) True or False: Abnormally high results of specific gravity >1.040 can be caused by the following: excretion of the injected radiographic contrast media (IVP) patients receiving dextran and other IV plasma expanders 380) True or False: Reagent strip readings and osmometry are not affected by high-molecular-weight substances. 381) In _____, a more representative measure of renal concentrating ability can be obtained. 382) True or False: Specific gravity depends on the number of particles present in a solution and the density of these particles, whereas osmolality is affected only by the number of particles present. 383) The substances of interest for osmolality include small molecules of what? 384) _____ is defined as 1 g molecular weight of a substance divided by the number of particles into which it dissociates. 385) Glucose has a molecular weight of _____ g/osm. 386) NaCl has a molecular weight of _____ g/osm. 387) What unit of measure is used in the clinical laboratory? 388) _____ of a solution can be determined by measuring a property that is mathematically related to the number of particles in the solution 389) Lower freezing point, higher boiling point, increased osmotic pressure, and lower vapor pressure are all changes in _____ properties 390) What is measured in the urinalysis laboratory with an osmometer? 391) The additional step to the routine urinalysis procedure is: 392) What does an automated osmometer utilize to measure osmolality? 393) What change is the reagent strip reaction based on? True True osmolality True sodium, chloride, and urea Osmole 180 58.5 milliosmole (mOsm) osmolality colligative Osmolality. Measuring osmolality with an osmometer. Freezing point depression. The change in pka (dissociation constant) of a polyelectrolyte in an alkaline medium. 27 UA PPT Flashcards 394) Releasing H+ions in proportion to the number of ions in the solution. 395) What effect will an increased number of H+ ions on pH? 396) What indicator on the reagent pad measures the change in pH? 397) What is the range of the bromothymol-LS blue indicator? 398) What has no effect on reagent strip? 399) What is not routinely reported in urinalysis? 400) How does fresh urine smell? 401) What does older urine smell like? 402) Maple syrup urine disease is caused by a: 403) What causes a fruity odor to urine? 404) What smell permeates with an infection? 405) What foods cause an odor in urine? 406) Why can’t all people smell asparagus in urine? 407) If urine smells mousy, you may suspect the patient has: 408) What odor does urine emit with tyrosinemia? 409) What does Isovaleric academia cause? 410) What malabsorption causes urine to smell like cabbage? 411) Bleach odor in a urine sample indicates: 412) What routine chemical tests on urine is simple and fast? 413) What two types of reagent strips are available? 414) Is there significance in the brand and number of reagent strip test? 415) What to reagent strips consist of? 416) What occurs when the absorbent pads of the reagent strips come in contact with urine? 417) How is the reagent strips reaction interpreted? 418) What information do the charts supplied by the manufacturer? Direct It will lower the pH. Bromothymol-LS blue From blue (1.00 [alkaline]) through shades of green to yellow (1.030 [acid]) Non-ionizing substances Odor Faintly aromatic Ammonia Metabolic disorder Ketosis Unpleasant ammonia smell Garlic, onions, and asparagus Genetically not all people are capable. Phenylketonuria. Rancid. Urine with a sweaty feet smell. Methionine. Contamination. Reagent strips. Single and multitest varieties. No, it is based on laboratory preference. Chemical-impregnated absorbent pads on a plastic strip. A color-producing reaction. By comparing the color produced on the pad within the required time frame with a chart supplied by the manufacturer. Several degrees of color comparison to provide semiquantitative readings of neg, trace, 1+, 2+, 3+, 4+, and occasionally estimates of mg/dL for the test areas. 28 UA PPT Flashcards 419) What is the proper technique for a reagent strip test? 420) What errors occur with improper technique? 421) The following requirements are necessary for? Store below 300C in a tightly sealed container with desiccant. Remove strips immediately prior to use. Do not expose to volatile fumes. Do not use past expiration date. Visually inspect for discoloration/deterioration. 422) How often should quality control be done on reagent strips? 423) When should additional controls be run on reagent strips? 424) Why should distilled water not be used as a negative control? 425) Are there manufactured positive and negative controls available? 426) True or False: All control results must be recorded. 427) True or False: All negative control readings should be negative. 1. Dip strip into well-mixed specimen at room temperature. 2. Remove excess urine by touching edge of strip to container as strip is withdrawn. 3. Blot edge of strip on absorbent pad. 4. Wait specified amount of time. 5. Read using a good light source. 1. Formed elements, such as red and white blood cells, sink to the bottom of the specimen and will not be detected in an unmixed specimen. 2. Leaching of reagent from the pads by allowing the strip to remain in the urine for an extended period of time. 3. Distortion of the color between chemicals on adjacent pads occurs when excess urine remains on the strip. 4. Not following manufacturer’s stated time. 5. Accurate interpreatation of color reactions requires a good light source. 6. Using the appropriate manufacturer color charts. 7. Refrigerated specimens not allowed to come to room temperature. Proper handling and storing for reagent strips. Run positive and negative controls at least once per 24 hours 1. New bottle of strips is opened. 2. Results are questionable. 3. Concerns over strip integrity. Reactions are designed for urine ionic concentration. Yes. True. True. 29 UA PPT Flashcards 428) What should positive control readings agree with? 429) What should you be aware for quality control of reagent strips? 430) True or False: Chemical readings should correlate with each other and physical and microscopic readings. 431) What uses different reagents or methodologies to detect the same substances as reagent strips with the same or greater sensitivity or specificity? 432) What may be used when questionable results are obtained in confirmatory testing? 433) What must be checked using positive and negative controls? 434) Lungs and kidneys are major regulators of acid-based content in: 435) The normal urine pH range is: 436) True or False: Absolute values are assigned to urine pH. 437) First morning urine is: 438) Postprandial urine is more: 439) What makes urine pH vary from patient to patient? 440) What pH level is associated with aged, improperly preserved specimen, and a new specimen should be obtained? 441) What clinical significance does urine pH provide? 442) What measures pH between 5.0 and 9.0 in one half or one unit increments? 443) How does the double-indicator system reaction indicate pH? Published control values. Manufacturer-stated limitations and interfering substances. True. Confirmatory testing. Non-reagent strip testing procedures using tablets and liquid chemicals. Chemical reliability. Urine pH. 4.5 to 8.0. False. Slightly acidic at 5.0 to 6.0. Alkaline. 1. Acid-based content of the blood. 2. Patient’s renal function. 3. Presence of a urinary tract infection. 4. Patient’s dietary intake. 5. Age of specimen. pH of 8.5 or above. Respiratory or metabolic acidosis/ketosis Respiratory of metabolic alkalosis Renal tubular acidosis Renal calculi formation Treatment of UTI Precipitation/identification of crystals Determination of unsatisfactory specimens pH-Reagent Strip Reactions Methyl red for 4 to 6 with red/orange to yellow color. Bromthymol blue for 6 to 9 with green to blue color. 30 UA PPT Flashcards 444) True or False: There are no known substances that interfere with urinary pH measurements performed by reagent strips. 445) The most indicative substance of renal disease in urine is: 446) When is proteinuria present in renal disease? 447) Normal urine protein levels are: 448) Low-molecular-weight serum proteins are: 449) What is the primary protein of concern in urine? 450) What other urine proteins are examined? 451) Presence of protein in urine requires: 452) What urine protein levels indicate proteinuria? 453) What causes protein in the urine? 454) How does prerenal proteinuria develop? 455) Where does prerenal proteinuria occur? 456) Where is prerenal proteinuria rarely seen? 457) How is multiple myeloma confirmation done? 458) Bence Jones Protein (BJP) can be indicative of: 459) What is Bence Jones Protein (BJP)? 460) Renal proteinuria is indicative of: 461) What other conditions can cause glomerular or tubular damage? 462) What causes glomerular proteinuria? 463) What immune substances deposit on the membrane? 464) What immune disorders result in glomerular proteinuria from immune complex formations? 465) What causes increased pressure on the kidney filtration mechanism? 466) Strenuous exercise, high fever, dehydration, and exposure are causes of: True. Protein. Early renal disease. <10mg/dL or 100mg/24hr Filtered and reabsorbed. Albumin. Vaginal, prostatic, seminal, and Tamm-Horsfall (uromodulin) Determination of normal or pathological condition 30mg/dL, 300mg/24hr Prerenal, renal, and postrenal. Transient low-molecular-weight plasma proteins acute phase reactants increase and exceed the reabsorptive capacity. The plasma. Reagent strip. Serum electrophoresis. Multiple myeloma (plasma myeloma) Immunoglobulin light chains in urine. Glomerular or tubular damage Glomerular proteinuria, microalbuminuria, Orthostatic (postural) proteinuria, and tubular proteinuria Damage to glomerular membrane from impaired selective filtration from increased protein filtration. Amyloids and other toxins. Lupus erythematosus and streptococcal glomerulonephritis Hypertension Strenuous exercise Dehydration Pregnancy, especially Preeclampsia Benign proteinuria (transient) 31 UA PPT Flashcards 467) What causes diabetic nephropathy in type 1 and type 2 diabetes mellitus with reduced glomerular filtration and eventual renal failure? 468) Microalbuminuria is associated with an increased risk of: 469) Orthostatic (postural) proteinuria appears when there is: 470) What are the collection instructions for a postural proteinuria? 471) Why are two specimens required for a postural proteinuria test? 472) Acute tubular necrosis is caused by: 473) Fanconi syndrome is a: 474) What malignancy does tubular proteinuria? 475) Extended tubular proteinuria may lead to: 476) True or False: Same amounts of urine protein are found in glomerular disorders and tubular disorders. 477) Postrenal proteinuria can be caused by: 478) What are the traditional principles for a protein-reagent strip reactions? 479) What overrides the acid buffer system? 480) What gives false-positive results? 481) What is the confirmatory test for protein? 482) What type of specimen is needed for Sulfosalicylic Acid? Microalbuminuria Cardiovascular disease Increased pressure on the renal vein when in the vertical position, but disappears in horizontal position. 1. Empty bladder before bed. 2. Collect specimen immediately on arising The first morning specimen will show negative, and the second specimen will be found positive. Toxic substances, heavy metals, viral infections, Fanconi syndrome. Generalized convoluted tubule defect. Tubular damage affecting reabsorptive ability. Acute tubular necrosis. False. Protein added in the lower urinary and genitourinary tract. Microbial infections causing inflammations and release of interstitial fluid protein. Menstrual contamination. Semen/ prostatic fluid. Vaginal secretions. Traumatic injury. a. protein error of indicators b. certain indicators change color in the presence of protein at a constant pH c. Protein accepts H+ from the indicator, increased sensitivity to albumin due to more amino groups to accept H+ than other proteins Highly buffered alkaline urine a. highly pigmented urine b. high specific gravity c. quaternary ammonium compounds, detergents, antiseptics, chlorhexidine Sulfosalicylic Acid Precipitation Centrifuged specimen to remove any extraneous contamination 32 UA PPT Flashcards 483) What is the semiquantitative testing for patients at risk for renal disease? 484) What measures creatinine to produce an albumin:creatinine ratio? 485) What specimen is recommended for microalbuminuria? 486) What technique is used for Immunodip Test? 487) How does Immunodip Test work? Microalbuminuria Microalbuminuria First morning specimens Immunochromographic technique • • • • • • 488) How does Micral-Test work? • • • • • • • • 489) What strips are used for microalbumin tests? 490) How does Clinitek microalbumin reagent strips and Multistix Pro reagent strips work? 491) What is albumin strip dye? 492) How does creatinine reagent strip work? 493) What is the purpose of creatinine reagent strip? Place container in controlled amount of specimen for 3 min, urine enters container Albumin binds to blue latex particles coated with antihuman albumin antibody Bound and unbound migrate up strip Unbound encounters area of immobilized albumin on strip—forms blue band Bound continues migrating to an area of immobilized antibody and forms blue band Color of band is compared with chart Dip strip in urine to marked level for 5 seconds Albumin binds to antibody Bound and unbound conjugates move up strip Unbound removed in captive zone containing albumin; bound continues up strip Reaches enzyme substrate, reacts Colors from white (neg) to red (varying degrees) Compare color to chart Results read from 0 to 10 mg/dL Clinitek microalbumin reagent strips and Multistix Pro reagent strips • Simultaneous measurement of albumin and creatinine • Provide an estimate of the 24-hour albumin concentrations from random urine • Albumin pad uses dye-binding reaction for specific albumin testing It is specific for albumin. It has a sensitivity of 8 to 15 mg/dL. It is highly buffered alkaline urine interference, which is controlled by treated paper. Creatinine combines with copper sulfate to form copper-creatinine peroxidase Peroxidase reacts with DBDH, releases oxygen ions that oxidized TMB Colors change from orange to green to blue To correlate creatinine with albumin results to determine the albumin:creatinine ratio 33 UA PPT Flashcards 494) What strips measures creatinine? 495) What methods does Bayer Multistix Pro 10 strips measure? 496) What are not included on Bayer Multistix Pro 10 strips? 497) How are Albumin:Creatinine Ration reported as? 498) What is the most frequent chemical analysis performed on urine? 499) What is the major screening test for diabetes mellitus? 500) What is the renal threshold for glucose? 501) What is renal glycosuria? 502) How does glucose oxidase reaction work? 503) Is glucose oxidase reaction specific for glucose? 504) What are the reasons for falsepositive results? 505) What are the reasons for falsenegative results? 506) How does Copper Reduction Test work? 507) What is the procedure of clinitest? 508) Pass through clinitest procedure include________. 509) What is Reducing substances test mean? Bayer Mutistix Pro 10 Protein-high is protein error of indicators method Protein-low is dye-binding method Urobilinogen and bilirubin Results are reported as Normal or Abnormal Glucose Glucose test 160 to 180 mg/dL Tubular reabsorption disorder Glucose oxidase catalyzes a reaction between glucose and oxygen Peroxidase catalyzes the reaction between peroxide and chromogen to form an oxidized colored compound True Only peroxide, oxidizing detergents Ascorbic acid and strong reducing agents High levels of ketones High specific gravity and low temperature Greatest source of error is old specimens Reduction of copper sulfate to cuprous oxide with alkali and heat • Pass through • Hygroscopic tablets: strong blue color and excess fizzing = deterioration -High levels of reducing substance -Color from blue through red back to green-brown: rapid reaction -Repeat with two-drop procedure • • • • Not a specific test for glucose Clinitest does not provide a confirmatory test for glucose Interference from reducing sugars Major use is quick screen for “inborn error of metabolism” in children up to 2 years old 34 UA PPT Flashcards 510) What is Ketones? 511) Three intermediate products of fat metabolism are_____________. 512) What is the clinical significance of Ketones? 513) What is Diabetic Ketoacidosis, and what is its cause? 514) Clinical significance of Ketonuria unrelated to diabetes are__________. 515) What is the primary reagent strip reaction of Ketone? 516) What dose sodium nitroprusside measure primarily? 517) Acetoacetic acid assumes________. 518) The reagent strip reaction result is______. 519) Identify the four reaction interference of Ketone? 520) What is Acetest? 521) What is the difference between Hematuria and hemoglobinurea? 522) The clinically significant of blood urine considered_________. 523) Chemical tests for hemoglobin is provide_______. • • products of fat metabolism Appear in urine when body stores of fat must be metabolized to supply energy -Acetone: 2% -Acetoacetic acid: 20% -β-hydroxybutyrate: 78% • Increased fat metabolism • Primary causes • Diabetes mellitus • Vomiting (loss of carbohydrates) • Starvation, malabsorption, dieting (↓ intake • Ketonuria shows insulin deficiency • Diabetic ketoacidosis -increased accumulation of ketones in the blood -Electrolyte imbalance, dehydration, and diabetic coma – Inadequate intake/absorption of carbohydrates – Vomiting – Weight loss – Eating disorders – Frequent strenuous exercise • sodium nitroprusside – (Nitroferricyanide) • acetoacetic acid -the presence of β-hydroxybutyrate and acetone acetoacetate (and acetone) + sodium nitroprusside Alkaline + (glycine) ——————> purple color • Levodopa in large dosage • Medications containing sulfhydryl groups • False-positive results from improperly timed readings • Falsely decreased values in improperly preserved specimens • Not a urine confirmatory test • Tablet = sodium nitroprusside, glycine, disodium phosphate, lactose (gives better color) • Hematuria: intact RBCs – Cloudy red urine • Hemoglobinuria: product of RBC destruction – Clear red urine • Any amount of blood greater than five cells per microliter of urine. the most accurate means for determining the presence of blood 35 UA PPT Flashcards 524) Why we used the microscopic examination in blood urine? 525) What is the cause of Hematuria? 526) What is the cause of Hemoglobinuria? 527) Hemoglobinuria may result from______. 528) What is hemosiderin? 529) What is Myoglobinuria? 530) What is Rhabdomyolysis? 531) What cause Rhabdomyolysis? 532) What is the reagent strip reactions of blood urine? 533) False –positive of reaction interference is_______. 534) False –negative reaction interference is_______. 535) What is bilirubin? to differentiate between hematuria and hemoglobinuria • Damage to renal system – Renal calculi – Glomerular disease – Tumors – Trauma – Pyelonephritis – Exposure to toxic chemicals – Anticoagulants – Transfusion reactions – Hemolytic anemias – Severe burns – Infections/malaria – Strenuous exercise/RBC trauma – Brown recluse spider bites The lysis of red blood in dilute, alkaline urine. yellow brown granules in sediment • heme-containing protein in muscle tissue; clear, red/brown urine muscle destruction • Muscular trauma/crush syndromes • Prolonged coma • Convulsions • Muscle-wasting diseases • Alcoholism • Drug abuse • Extensive exertion • Cholesterol-lowering statin medications • Principle pseudoperoxidase activity of hemoglobin • Catalyze a reaction between the heme component • Two charts corresponding to different reactions • Free hemoglobin shows uniform color • Intact RBCs show a speckled pattern on pad -Menstrual contamination, strong oxidizing agents, bacterial peroxidases – Ascorbic acid >25 mg/dL – High SG/crenated cells – Formalin – Captopril – High concentrations of nitrite – Unmixed specimens • Normal degradation product of hemoglobin • Body recycles iron, protein 36 UA PPT Flashcards • • 536) Early urine bilirubin indicate_______. 537) Unconjugated bilirubin is ________. 538) Conjugated bilirubin is_________. 539) What are forms of conjugated bilirubin? 540) What is clinical significance of bilirubin? 541) The reagent strip reactions of bilirubin is_______. 542) What is the reaction interference? 543) What is Ictotest? 544) What is Urobilinogen? 545) What is the difference between Urobilinogen and Stercobiliogen? Protoporphyrin is broken down into bilirubin Bilirubin is bound to albumin – Kidneys cannot excrete • Unconjugated bilirubin • Conjugated bilirubin • Unconjugated bilirubin to the liver • Forms conjugated bilirubin • Excreted in feces -Liver disease. Water insoluble. Water soluble. – From liver to intestines – Reduced to urobilinogen, stercobilinogen, and urobilin by intestinal bacteria • Conjugated bilirubin appears in urine with bile duct obstruction • Obstruction • Hepatitis, cirrhosis • Hemolytic disease • Principle is a diazo reaction • Report: neg, small (1+), moderate (2+), large (3+) • Colors may be difficult to interpret – Easily influenced by other pigments present in the urine • Atypical colors can be problem for automated readers • False-positive – Urine pigments – Pyridium (phenazopyridine) – Drugs indican, iodine • False-negative – Old specimens (biliverdin does not react) – Ascorbic acid >25 mg/dL – Nitrite • Combine with diazonium salt and block bilirubin reaction • Confirmatory for bilirubin • Use specified mat for test; mat keeps bilirubin on surface for reaction • Positive reaction = blue-to-purple color • Interfering substances are washed into the mat, and only bilirubin remains on the surface Is when bilirubin in intestine converted to Urobilinogen and Stercobilinogen. Urobilinogen is reabsorbed into circulation. Stercobilinogen is not reabsorbed into circulation. 37 UA PPT Flashcards 546) Is Urobilinogen filtered by the Kidney? 547) What are clinical significance of Urobilinogen? 548) What clinical significance exhibit urobilinogen in 1% of nonhospitalized and 9% of hospitalized population? 549) What is the result of urobilinogen in the urine with bile duct obstruction? 550) What are the principles for Multistix Ehrlich’s aldehyde reaction? 551) What are the principles for Chemstrip – diazo (azo-coupling)reaction? 552) What are the reaction interferences with Ehrlich reactive compounds? 553) What are the reaction interferences for both tests? 554) What are the reaction interferences for Chemistrip> 555) Rapid screening test for the presence of urinary tract infection (UTI)whith the presence of nitrie are: 556) Why is the reagent strip reaction for nitrite done? 557) What is the Greiss reaction result? • Yes, There is always a small amount of urobilinogen filtered by the kidneys and is found in the urine <1 mg/dL • Early detection of liver disease, greater than 1 mg/dL • Liver disorders, hepatitis, cirrhosis, carcinoma • Hemolytic disorders – Excess bilirubin being converted to urobilinogen and ↑ urobilinogen recirculated to liver • Negative bilirubin and strong positive urobilinogen are seen in hemolytic disorders Elevated results which is frequently caused by constipation No urobilinogen is seen; strip will give a normal result; reagent strips cannot report a negative reading - p-dimethylaminobenzaldehyde (Ehrlich reagent); report in Ehrlich units (EU) 1 EU = 1 mg/dL - Normal readings 0.2 to 1, abnormal 2, 4, 8 - Light to dark pink urobilinogen + p-dimethylaminobenzaldehyde -acid→ red color - 4-Methoxybenzene-diazonium-tetrafluoroborate; more specific than Ehrlich reaction; report in mg/dL - White to pink urobilinogen + diazonium salt-acid→red azodye - porphobilinogen, indican, sulfonamides, methyldopa, procaine, chlorpromazine, p-aminosalicylic acid - urobilinogen is highest after meals (increased bile salts), old specimens and formalin preservation decrease results - false-negative with high nitrite interferes with diazo reaction - Pyelonephritis (tubules) - Evaluation of antibiotic therapy - Monitoring of patients at high risk for urinary tract infection - Cystitis (initial bladder infection) - Screening of urine culture specimens (in combination with LE test) To test ability of bacteria to reduce nitrate (normal constituent) to nitrite (abnormal) -nitrite reacts with aromatic amine to form a diazonium salt that then reacts with tetrahydrobenzoquinoline to form a pink azodye 38 UA PPT Flashcards 558) Reagent strip reaction correspond with what? 559) What are the interference for nitrite test that give false-negative reactions? 560) What are the interference for nitrite test that give false-positive reactions? 561) Leukocyte Esterase (LE) provides: 562) What is the purpose of Leukocyte Esterase (LE)? 563) What is the advantage of Leukocyte Esterase (LE)? 564) Is Leukocyte Esterase (LE) a quantitative test? 565) What is the clinical significance for Leukocyte Esterase (LE)? 566) What test is better predictor than nitrite test for screening of urine culture specimens? 567) With what other infections is the LE present? 568) What are the reagent strip reactions with LE? 569) What is the longest time of all the reagent strip reactions for LE? 570) How are the results reported? 571) Is trace reading significant for LE test? a quantitative bacterial culture criterion of 100,000 organisms/mL - Insufficient contact time between bacteria and urinary nitrate - Lack of urinary nitrate - Large quantities of bacteria converting nitrite to nitrogen - Presence of antibiotics - High concentrations of ascorbic acid - Nonreductase-containing bacteria - High specific gravity - Negative results in the presence of even vaguely suspicious clinical symptoms should always be repeated or followed by a urine culture - Highly pigmented urine - Pink edge or spotting on reagent strip is considered negative - Old specimens (bacterial multiplication) - Check automated readers manually for color interference Standardized means for the detection of leukocytes LE test detects the presence of esterase in the granulocytes and monocytes detects presence of lysed leukocytes No; must to do microscopic test if positive It is positive in: - Bacterial and nonbacterial urinary tract infection - Inflammation of the urinary tract Leukocyte Esterase (LE) test Trichomonas, Chlamydia, yeast, interstitial nephritis LE catalyzes hydrolysis of acid esterase on pad to aromatic compound and acid; aromatic compound reacts with diazonium salt on pad for purple color 2 minutes - Negative - Trace - Small: 1+ - Moderate: 2+ - Large: 3+ Trace readings may not be significant and should be repeated on a fresh specimen 39 UA PPT Flashcards 572) What are the interference for LE test that give false-positive reactions? 573) What are the interference for LE test that give false-negative reactions? 574) What is specific gravity based on? 575) How does specific gravity work? 576) What indicator measures pH change and what colors can we see? 577) What are the reaction interference for specific gravity? 578) What is other interference reaction from large molecules, glucose and urea and radiographic dye and plasma expanders? 579) Macroscopic screening is performed based on what results? 580) List the performed macroscopic tests. 581) List special population for the macroscopic screening in urine. 582) Clinical and Laboratory Standards Institute (CLSI) states that all decisions should be based on the needs of: 583) Why specimen preparation should be examine when fresh or preserved? 584) What happens when urine specimen is refrigerated ? 585) Less contamination (epithelial cells) from comes from specimen that is a: 586) Before decanting to the centrifuge tube 587) specimen must be: 588) What is the requirement for the urine specimen volume? - Formalin - Strong oxidizing agents - Highly pigmented urine, nitrofurantoin - High concentrations of protein, glucose, oxalic acid, ascorbic acid - Crenation from high specific gravity - Inaccurate timing: must have 2 min - Presence of the antibiotics; gentamicin, cephalosporins, tetracyclines It is based on pKa (dissociation constant) of a polyelectrolyte in alkaline medium - Polyelectrolyte ionizes releasing H+ in relation to concentration of urine - ↑concentration = more H+ released bromthymol blue; blue (alkaline) through green to yellow (acid) - Slight elevation from protein -Decreased readings: urine pH 6.5 or higher *Interferes with indicator; add 0.005 to the reading; readers automatically add this difference in refractometer reading physical and chemical Color, clarity, blood, protein, nitrite, leukocyte esterase, and possibly glucose pregnant women; pediatric, geriatric, diabetic, immunocompromised, and renal patients - Requested by the physician - Laboratory-specified population - Any abnormal physical or chemical result - RBCs, WBCs, casts disintegrate in dilute, alkaline urine Refrigeration precipitates crystals, also can obscure other elements midstream clean-catch specimen thoroughly mix - Centrifuge 10 to 15 mL urine (reagent strips fit into 12 mL) - Quantities <12 mL should be documented - Too little volume = fewer formed elements - Some laboratories correct for volume 40 UA PPT Flashcards 589) Standardized speed and time, and capped specimen is required for: 590) What are the specifications for centrifugation? 591) What are the characteristics of sediment standardization? 592) Commercial systems: KOVA in sediment standardization includes: 593) What postcentrifuge sediment include? 594) What is the concentration factor of postcentrifuge sediment? 595) What is important in postcentrifuge sediment? 596) What include glass slide method of volume and sediment examination? 597) Chambers capable of containing a standardized chamber volume, size of the viewing area, and approximate number of low-power and high-power viewing areas are part of: 598) Commercial systems are based on: 599) Commercial systems are recommended together with standardization of all phases of the methodology by what organization? 600) What commercial systems require? 601) Commercial systems include slides that: 602) Examination of sediment require: 603) What can be seen under low power of sediment examination? centrifugation - 5 min at relative centrifugal force (RCF) of 400 is ideal - RCF corrects for variations in the diameter of centrifuge heads; revolutions per minute does not - RCF = 1.118 × 10−5 × radius in centimeters × RPM2 - Preparation of sediment - Volume of sediment examined (0.5 to 1.0 mL) - Methods of visualization - Reporting of results Calibrated centrifuge tubes, special slides to control volume, decanting pipettes, grids for better quantitation 0.5 to 1.0 mL of sediment after decantation volume of urine centrifuged/sediment volume with the probability of detecting low quantities of formed elements - Aspirate rather than pour off urine (pipettes available for this) - Mix sediment gently, not vigorously - 20 μL in 22 × 22 glass cover slip - Do not overflow cover slip; heavier elements (casts) flow outside Commercial systems the area of the field of view using a standard microscope CLSI - Capped, calibrated centrifuge tubes - Decanting pipettes to control sediment volume - Control the amount of sediment examined - Produce a consistent monolayer of sediment for examination - Provide calibrated grids for more consistent quantitation - Minimum 10 low (10×) and 10 high (40×) fields - Use fine adjustment continuously for best view casts, general composition; scan edges for casts with glass slide method 41 UA PPT Flashcards 604) What can be seen under high power of sediment examination? 605) How is the initial focusing performed? 606) Reporting the microscopic examination must be: 607) How do we report casts results? 608) How do we report epithelial cells, crystals, etc., in semiquantitative terms? 609) Converting the average number of elements per lpf or hpf to elements per mL is done by: identification of type of the sediment Use low power, reduced light and focus on epithelial cell, not artifacts that are in a different plane Consistent within laboratory average per lpf - Few, moderate, many - 1+, 2+, 3+, 4+ - Follwed by /lpf or /hpf 1. Calculating the area of an lpf or hpf for the microscope in use using the manufacturer-supplied field of view diameter and the formula πr2 = area Diameter of hpf = 0.35 mm 3.14 × 0.1752 = 0.096 mm2 2. Calculating the maximum number of lpfs or hpfs in the viewing area; area under a 22 mm × 22 mm cover slip = 484 mm2 484 = 5040 hpfs .096 3. Calculating the number of hpfs per milliliter of urine tested using the concentration factor and the volume of sediment examined 5040____ = 5040 0.02 mL x 12 .24 610) How does sediment appear in the sediment examination techniques? 611) What is often difficult to see under bright-field microscopy? 612) Describe the reaction of SternheimerMalbin stain in the sediment. 613) What includes Sternheimer-Malbin stain? 614) What enhances nuclear detales of the sediment? = 21,000 hpf/mL of urine 4. Calculating the number of formed elements per milliliter of urine by multiplying the number of hpfs per milliliter by the average number of formed elements per field 4 WBC/hpf × 21,000 = 84,0 WBC/mL - Cells and casts in various stages of development and degeneration - Distortion of cells and crystals by the chemical content of the specimen - The presence of inclusions in cells and casts - Contamination by artifacts Low refractive index elements - Increases refractive index - Stains nuclei, cytoplasm, inclusions - crystal violet /Safranin O - Sedi-Stain, KOVA stain, etc. 0.5% solution of toluidine blue 42 UA PPT Flashcards 615) What enhances WBC nuclei and lyses RBC’s? 616) What stains lipids (triglycerides and neutral fats; cholesterol polarizes)? 617) What stain identifies bacterial casts? 618) What stain identifies urinary eosinophils? 619) What stain identifies hemosiderin granules seen with hemoglobinuria? 620) What is the purpose of Cytodiagnostic urine testing? 621) Preparation of permanent slides using what technique? 622) Papanicolaou stain is use to stain what? 623) What microscope is the most commonly used microscope? 624) How does Brightfield microscope help in urinalysis? 625) What other variety of microscopy are in the field? 626) What distinguishes Phase-contrast microscopy from other? 627) What distinguishes Polarizing microscopy from others? 628) What distinguishes Interferencecontrast from others? 629) What makes up the Compound brightfield microscope? 630) The two-lens system has what use? Acetic acid Oil Red O and Sudan III Gram stain - Hansel stain - Methylene blue and eosin Y: better than Wright stain Prussian blue stain Purpose is frequently performed to detect and monitor renal disease/malignancies. Cytocentrifugation – Transplant rejection – Viral, fungal, and parasitic infections – Cellular inclusions – Pathologic casts Inflammatory conditions Brightfield It allows.. – – – Reduced light is essential Magnification is 10× and 40× Par focal means minimal adjustment when changing objectives (use fine adjustment) – Lower light using the rheostat – Condenser can be raised up and down – Do not use the aperture diaphragm Others include phase contrast, polarizing, dark field, fluorescence, and interference contrast – Increases refractive index – – – – – Crystals and lipids Ability to split light into two beams Crystals are multicolored Cholesterol produces Maltese cross formations Three-dimensional images – – – – – – Two-lens system Illumination system Body consisting of Mechanical stage In the oculars, the objectives The coarse- and fine-adjustment knobs 43 UA PPT Flashcards 631) The Illumination system has what use? Light source, condenser, and field and iris diaphragms 632) The body of the microscope consist – Base of? – Body tube – Nosepiece Mechanical stage 633) Binocular is use for what purpose? Adjusts for interpupillary distance 634) Field of view is determined by what? The eyepiece and is the diameter of the circle of view when looking through the oculars. 635) What objective lens is use for UA Magnifications of 10x (low power,dry) and 40x (high sediment examination? power, dry). 636) Final magnification of an object is the The objective magnification times the ocular product of? magnification. 637) Name the objective characteristics of – Type of objective, magnification, numerical aperture, the microscope? microscope tube length, and cover-slip thickness to be used – Length of the objectives attached to the nosepiece varies with magnification – Changing the distance between the lens and the slide when they are rotated 638) What is parfocal? Only minimum adjustment when switching among objectives. 639) The distance between the slide and Controlled by the coarse and fine focusing knobs. the objective is? 640) Coarse focus does what? Initial focusing 641) Fine focus does what? Sharpen image, focusing after changing magnification. 642) The microscope is consist of what? – Base – Equipped with rheostat – Regulates intensity – Filters vary illumination and wavelength – Diaphragm contained in the light source controls the diameter of the light beam – Condenser located below the stage to focus the light – All have adjustments for optimal lighting 643) What is Köhler illumination? Provide optimal viewing of the illuminated field. 644) Steps for care of the microscope 1. Carry microscope with two hands, supporting the base with one hand. 2. Always hold the microscope in a vertical position. 3. Only clean optical surfaces with a good quality lens tissue and commercial lens cleaner. 4. Do not use the 10× and 40× objectives with oil. 5. Clean the oil immersion lens after use. 6. Always remove slides with the low-power objective raised. 7. Store the microscope with the low-power objective in position and the stage centered. 44 UA PPT Flashcards 645) Urine sediment constituents consist of? • • • • 646) What the identification of yeast? 647) What the identification of oil droplets? 648) What the identification of air bubbles? 649) What the identification of starch? 650) What are the characteristics of RBC? 651) What does Dysmorphic RBCs cause? 652) How does Dysmorphic RBCs help doctor? 653) Damage to glomerular membrane cause damage to what? 654) Number of cells represents what? 655) What is the normal value? 656) Macroscopic versus microscopic hematuria? 657) What the normal size of WBCs? 658) What WBC is normal most abundant? 659) WBCs are identify under what power? 660) What are characteristics of glitter cells? 661) What conditions are eosinophils associated with? 662) What special about Hansel stain? Small amounts of constituents can be normal or pathogenic based on the clinical picture Many urines have just a rare epithelial cell Some constituents are easily distorted – Concentrations, pH, and presence of metabolites Normals are not clearly defined Look for buds Refractility Refractility and possibly in a different plane Refractile, polarizes • Smooth, nonnucleated, biconcave disks ~7 µm • Crenated in hypersthenuric urine • Ghost cells in hyposthenuric urine • Identify using high power – Glomerular bleeding – Strenuous exercise – Acanthocytic, blebs Fragmented, hypochromic Aid in diagnosis Vasular injury to the genitourinary tract Extent of damage 0-3 to 5/hpf – Cloudy, red urine, advanced disease, trauma, acute infection, coagulation disorders Clear urine, early glomerular disease, malignancy, strenuous exercise, renal calculi confirmation 12 µm Neutrophils High power – Hypotonic urine – Brownian movement – Swell; granules sparkle – Pale blue if stained Nonpathologic – Drug-induced interstitial nephritis Renal transplant rejection – Percent per 100 to 500 cells – >1% significant Concentrate sediment, centrifuge, or cytocentrifuge 45 UA PPT Flashcards 663) What are mononuclear cells? 664) What lymphocytes resemble? 665) Mononuclear may need to refer to what testing? 666) What is the normal hpf in female? 667) Increased WBCs in urine is known as? 668) What symptoms does infection cause? 669) What clinical finding can you? 670) What must you report in clinical significance? 671) What are three types of epithelial cells? 672) What are classification of epithelial cells? 673) What are some significance of squamous epithelial cells? 674) Clue cells are what type of cell? 675) An example of vaginal infection? 676) Coccobacillus species are commonly found in? 677) What are the three form of Transitional Epithelial cells? 678) Transitional epithelial cells are differentiate from RTE how? 679) What does syncytia mean? 680) What causes syncytia? 681) What are the shapes of the renal tubular epithelial cells and where are they found? – Lymphocytes, monocytes, macrophages, histiocytes are rare – Differentiate from renal tubular epithelial (RTE) cells • Staining May resemble RBCs; seen in early transplant rejection cytodiagnostic <5 hpf Pyuria Cystitis, pyelonephritis, prostatitis, and urethritis. Glomerulonephritis, lupus erhthematosus, interstitial nephritis, tumor. Report presence of bacteria. 1. 2. 3. – Squamous Transitional (urothelial) RTE Squamous: vagina, male and female urethra – First structures observed – Transitional: bladder, renal pelvis, calyces, ureters, upper male urethra RTE: renal tubules • Largest cell in urine • Good for focusing microscope • Rare, few, moderate, many • lpf or hpf per laboratory • Normal sloughing Contamination if not midstream clean-catch Squamous cell with pathologic significance Gardnerella vaginalis Seen in urine but more common in vaginal wet preparation 1. Spherical: absorb water in bladder and become large and round 2. Caudate: appear to have a tail 3. Polyhedral: multiple sides Centrally located nucleus Syncytia = clumps Catheterization Malignancy Columnar = proximal convoluted tubule (PCT) Round, oval = distal convoluted tubule (DCT) Cuboidal = collecting duct 46 UA PPT Flashcards 682) What are the characteristics of the PCT cells? 683) What are the characteristics of the DCT cells? 684) What are the characteristics of the collecting duct RTEs? 685) Which renal tubular cells are the most clinically significant and why? 686) What are Oval Fat Bodies? 687) What conditions are associated with Oval Fat Bodies? 688) If bacteria if found in the urine, which type is more common: rods or cocci? 689) What urine conditions are ideal for yeast growth? 690) What is the most common parasite found in urine? 691) What is the significance of spermatozoa in urine? 692) What are some characteristics of mucus in urine? 693) What are the characteristics of casts in the urine? Larger than other RTEs Columnar, convoluted, rectangular May resemble casts Coarsely granular cytoplasm Notice presence of nucleus Round or oval shaped, smaller May resemble WBCs or spherical transitional cells Observe the eccentrically placed nucleus to differentiate from spherical transitional Cuboidal, never round -At least one straight edge -Eccentric nucleus Three or more cells in clump is renal fragment; often large sheets RTE cells are the most clinically significant urine epithelial cells; indicate tubular necrosis; fragments indicate severe destruction -Heavy metals, drug toxicity, hemoglobin, myoglobin, viral infections, pyelonephritis, transplant rejection, salicylate poisoning RTE cells that have absorbed lipid in the filtrate Lipiduria: nephrotic syndrome, acute tubular necrosis, diabetes, crush syndromes Rods are most common Diabetic urine: ↑ glucose and acid ideal for yeast growth Most common: Trichomonas vaginalis Pear-shaped flagellate Swims across field rapidly infertility: sperm expelled into bladder instead of urethra. May cause positive protein Protein from RTE, glands, squamous cells Threadlike, low refractive index Confuse with casts Irregular, composed of uromodulin protein Female specimens, no clinical significance Elements unique to the kidney Formed in DCT and collecting duct Parallel sides, rounded ends, inclusions Detect under low power, ID high power Scan edges of glass cover slip Low light is essential Report number per lpf Many pathologic and nonpathologic causes 47 UA PPT Flashcards 694) What is Uromodulin Protein? 695) How is Uromodulin formed? 696) What are the physical characteristics of hyaline casts? 697) What pathologic conditions are associated with hyaline casts? 698) How can RBC casts be differentiated from RBC clumps? 699) What is the clinical significance of RBC casts? 700) How is tubular necrosis confirmed? 701) What is mostly seen in WBC casts? 702) When are WBC casts seen? 703) What are bacterial Casts? 704) What do bacterial casts resemble? 705) How do you look for bacterial cells? 706) Where are bacterial cells seen? 707) What are mixed cellular casts? 708) How do you look for mixed cellular casts? 709) Where are epithelial casts formed? 710) What pulls from damaged tubules in epithelia casts? 711) Where are the majority of cells on in epithelial casts? 712) In epithelia casts a stain is done to differentiate from WBC. Why? Uromodulin protein secreted by RTE of DCT and collecting duct Consistent excretion normally -↑ stress and exercise Formation of protein fibrils into matrix Urine stasis, acid pH, Na, and Ca Uromodulin protein not detected by reagent strips ↑ protein is from renal disease Aggregated uromodulin fibrils attached to RTEs Interweaving to loose network, traps elements More interweaving to form solid matrix Attachment of elements to matrix Detachment of fibrils from RTEs Excretion of cast Normal parallel sides or convoluted, wrinkled, cylindroid, occasional adhering cell or granule glomerulonephritis, pyelonephritis, chronic renal disease, congestive heart failure Look for cast matrix Bleeding within the nephron, casts are more specific than free RBCs in urine Glomerular damage or nephron capillary damage Glomerular damage: dysmorphic RBCs and elevated protein May be seen following strenuous exercise Look for RTE cells Mostly neutrophils and lobed nucleus and granules WBC casts are seen with infection and inflammation of the tubules Pyelonephritis: WBC casts, bacteria Acute interstitial nephtitis: WBC casts, no bacteria Pure bacteria or mixed with WBCs Granular casts By looking for free WBCs and bacteria, and by confirming with gram stain In pyelonephritis Glomerular nephritis: RBCs and WBCs By looking for predominant type of cell In DCT Fibrils forming cast On the cast matrix to show single nucleus 48 UA PPT Flashcards 713) What are the clinical significance in epithelial casts? 714) What kind of stain does the epithelial casts might appear as? 715) In epithelial casts what do you want to look for to distinguish fragments? 716) What are fatty casts seen with? 717) Oval fat bodies may attach to matrix and are: 718) What kind of stain does fatty casts look like? 719) How do fatty casts look like under a microscope? 720) Nephritic syndrome, diabetes, crush trauma, and tubular necrosis are all associated with: 721) In mixed cellular casts where are RBC and WBC casts located? 722) In mixed cellular casts where are the WBC and bacterial casts located? 723) What aids in identifying mixed cellular casts? 724) What do granular casts look like? 725) Granule origin is in RTE lysosomes, excreted in normal metabolism, more after exercise and activity, and disintegration of cellular casts and free cells. True or False 726) What power are granular casts detected under? 727) What power are granular casts ID under? 728) Granules are disintegrated to form: 729) Where do you want to look when differentiating granular casts from clumps of debris and crystals. 730) Waxy casts are: 731) When are waxy casts well seen? 732) What are waxy casts? 733) Extreme urine stasis and renal failure are associated with: 734) What are broad casts? 735) All types of casts are broad. True or false Tubular damage, heavy metals, viral infections, drug toxicity, graft Bilirubin stained The Matrix Oval fat bodies (OFBs) and fat droplets Highly refractile Lipid stains Polarized Fatty casts In the glomerulonephritis In the pyelonephritis Staining or phase microscopy Coarse and finely granular True Low power High power Waxy casts Look for matrix Brittle, highly refractile, and fragmented with jagged ends and notches. With staining Degenerated hyaline and granular casts Waxy casts The destruction and widening of the DCTs formed in the upper collecting duct True 49 UA PPT Flashcards 736) What are the most common broad casts? 737) In broad casts where is the bilirubin stained from. 738) Renal failure casts is associated with: 739) What is caused by medications or treatments in urinary crystals? 740) Urinary crystals are not clinically significant but are reported. True or False 741) How are urinary crystals reported? 742) What are urinary crystals? 743) What must urinary crystals differentiate from? 744) What do urinary crystals indicate? 745) In urinary crystal formation what are the precipitation of urine solutes? 746) What are urinary crystal formation based on? 747) What temperature are urine crystal specimens kept. 748) What is needed in fresh specimens? 749) What do most urinary crystals have when identifying them? 750) What is the most valuable ID for urine crystals? 751) What are the classifications of urine crystals? 752) Where are all abnormal crystals found? 753) Polarized microscopy characteristics for urine crystals are valuable in: 754) What do temperature and pH contribute to for urine crystals? 755) What forms in refrigerated acid urine? 756) Amorphous urates will_____ with heat. A. Increase B. Decrease C. Dissolve D. Form Granular and waxy Viral hepatitis Broad casts Latrogenic True Rare few, moderate, many True geometrically formed structures or as amorphous material Few abnormal crystals Liver disease, inborn errors of metabolism, and damage to tubules Salts, organic compounds and medications Temperature, solute concentration, and pH Refrigerated High specific gravity Characteristic shapes and colors Urine pH Normal acid, normal alkaline In acid urine ID Formation and solubility Amorphous urates C. dissolve 50 UA PPT Flashcards 757) Amorphous phosphates form in refrigerated alkaline urine will ____ in acetic acid and so will ___ A. Increase, urine B. Decrease, crystals C. Dissolve, RBCs D. Form, crystals 758) What has yellow-brown granules, clumpy, and resemble casts? 759) What is the pH in amorphous urates? 760) Why does the urine sediment have a pink color in amorphous urates? 761) What do uric acid crystals look like? 762) Uric acid crystals resemble cystine crystals but they are always: 763) What increases in uric acid crystals? 764) Uric acid crystals are chemotherapy for what disease? 765) What is a major component of calcium oxalate? 766) An example that has Monohydrate calcium oxalate crystals is: 767) What appears to be similar to amorphous phosphates? 768) What happens to the amorphous phosphates after being refrigerated? 769) How does normal crystals look like in alkaline urine? 770) What do normal crystals in alkaline urine have? 771) What does normal crystals in alkaline urine cause? 772) Normal crystals in alkaline urine are: 773) What does calcium phosphate look like? 774) What does calcium carbonate look like? 775) What is produced with addition of acetic acid in calcium carbonate? 776) What do ammonium biurate crystals look like? 777) Ammonium Biurate Crystals are: 778) Where do ammonium biurate crystals form in? 779) What do cystine crystals look like? 780) What are cystine crystals similar to? C. dissolve, RBCs amorphous urates 5.5 The pigment uroerythrin attaching on surface of granules Yellow-brown color, rhombic, whetstones, wedges,, rosettes Polarized Purines Leukemia Renal calculi Antifreeze poisoning Amorphous urates Alkaline pH and heavy white precipitate forms Colorless, prism, coffinlid shape Triple phosphate High alkaline urine, UTIs Polarized Flat rectangles and thin prisms in rosettes Small, dumbbell, spherical shapes Gas Yellow-brown, spicule covered spheres, thorny apples only urates in alkaline urine in old specimens and with urea splitting bacteria Hexagonal, thin and thick plates Uric acid 51 UA PPT Flashcards 781) UA polarizes but only thick cystine crystals: 782) What is seen in cystinuria? 783) What does cystine crystals confirm? 784) What do cholesterol crystals look like? 785) What temperature must cholesterol crystals specimens be kept at? 786) What accompanies nephritic syndrome? 787) What is radiographic dye crystals similar to? 788) Is radiographic dye crystals polarized or not polarized? 789) What does radiographic dye crystals have? 790) What does tyrosine crystals look like? 791) What are tyrosine crystals seen with? 792) What disorder does tyrosine crystals inherited from? 793) What does Leucine crystals look like? 794) Crystals that are clumped needles or granules and has characteristic yellow color is: 795) What crystal has a positive reagent strip for bilirubin? 796) What is bilirubin crystals? 797) Sulfonamide crystals can cause tubular damage if crystals are formed where? 798) What are the characteristics of sulfonamide crystals? 799) Which crystals appear as colorless needles that tend to form bundles after refrigeration? 800) Name the types of Urinary Sediment Artifacts that can be seen when performing a Microscopic Examination? 801) What is ‘Renal Disease” Polarizes Inability to reabsorb cystine Cyanide nitroprusside Rectangular plates with characteristic notched corners Refrigerated Fatty casts and OFBs Cholesterol crystals Polarized High SG with refractometer Fine yellow needles in clumps or rosettes Leucine crystals Amino acid disorders Yellow-brown spheres with concentric circles and radial stirations Bilirubin crystals Bilirubin crystals Viral hepatitis with tubular damage Nephron Needles, rhombics, whetstones, sheaves of wheat, rosettes with colors ranging from colorless to yellow brown Ampicillin crystals • • • • 802) Name the 3 classifications renal disease? • • • • Material fibers, meat and vegetable fibers, and hair Starch, oil droplets, air bubbles, pollen grains, vegetable fiber, hair, diaper fiber Disorders throughout the body can affect renal function and produce abnormalities in the urinalysis The kidneys are consistently exposed to potentially damaging substances Glomerular disorders Tubular disorders Interstitial disorders 52 UA PPT Flashcards 803) What are the two types of Glomerular disorders? 804) Name the immunologic disorders. 805) Name the Nonimmunologic 806) General term for sterile, inflammatory process affecting the glomerulus that causes blood, protein, and casts in urine. 807) What are the 4 types of glomerulonephritis that progress through various disorders? 808) What test can be performed to diagnose Acute Poststreptococal Glomerulonephritis (AGN)? 809) What are some of the indications of AGN? 810) What is the more serious acute form that can cause renal failure and Systemic immune disorders such as: a. Macrophages damage capillary walls b. Fibrin = permanent damage to capillary tufts Urinalysis similar to AGN progresses to more abnormal, elevated protein, low glomerular filtration rate (GFR) May have increased fibrin degradation products (FDP), cryoglobulins and IgA immune complex depositions 811) What disorder causes: Morphological changes resembling crescentric GN • • – Majority are of immunologic disorders Nonimmunologic Immune complexes from immunologic reactions throughout the body – Increased serum immunoglobulins are deposited on the glomerular membranes – Immune system mediators: complement migrate and produce change and damage to membranes – Chemicals and toxins, deposition of amyloid material and acute phase reactants, electrical charge interference, membrane thickening Glomerulonephritis Acute glomerulonephritis to chronic glomerulonephritis to nephrotic syndrome to renal failure. • Rapid anti–group A streptococcal enzyme tests – Ease in diagnosis – Decline in incidence • Group A streptococcal infections from organisms with M protein in the cell wall • Fever, edema around the eyes, oliguria, and hematuria • Immune complexes deposit on glomerular membranes • Hematuria, proteinuria, oliguria – Red blood cell (RBC) casts, dysmorphic RBCs – Hyaline and granular casts – White blood cells – Anti–group A streptococcal enzyme tests Rapidly Progressive (Crescentic) Glomerulonephritis Goodpasture’s Syndrome 53 UA PPT Flashcards 812) Autoimmune disorder against glomerular and alveolar basement membranes 813) Cytotoxic antibody following viral respiratory diseases 814) Antiglomerular basement membrane antibody 815) Hemoptysis, hematuria, proteinuria, RBC casts 816) Chronic glomerulonephritis to endstage renal failure is common 817) What causes the immune response, producing granulomas in Wegener’s Granulomatosis? 818) What is the disease process of Wegener’s Granulomatosis? 819) What antibody is key to diagnosing Wegener’s Granulomatosis? 820) What test can be performed to diagnose Wegener’s Granulomatosis? 821) This disease is seen in children following upper respiratory infections who’s symptoms include: 822) Raised, red patches on skin 823) Blood in sputum and possibly stools 824) Renal involvement is the most serious complication of the disorder 825) Proteinuria and hematuria, RBC casts 826) 50% complete recovery 827) Follow patients for more serious renal problems 828) Name the types of Urinary Sediment Artifacts that can be seen when performing a Microscopic Examination? 829) Systemic lupus erythematosus, Sjögren’s syndrome, secondary syphilis, hepatitis B, gold and mercury treatments, malignancy can aid in the diagnosis of…. 830) What type of immunoglobulin immune complexes cause pronounced thickening of glomerulare basement membrane? Neutrophils initiate the immune response. • Inflammation and granulomas in small blood vessels of kidney and respiratory system • Pulmonary symptoms first, then hematuria, proteinuria, RBC casts, elevated BUN and creatinine levels Antineutrophilic cytoplasmic antibody (ANCA) Immunofixation for p-ANCA/c-ANCA Henoch-Schönlein Purpura • • Material fibers, meat and vegetable fibers, and hair Starch, oil droplets, air bubbles, pollen grains, vegetable fiber, hair, diaper fiber Systemic lupus erythematosus, Sjögren’s syndrome, secondary syphilis, hepatitis B, gold and mercury treatments, malignancy can aid in the diagnosis of…. What type of immunoglobulin immune complexes cause pronounced thickening of glomerulare basement membrane? 54 UA PPT Flashcards 831) Name the disorder: 832) Type 1: increased cellularity in the subendothelial cells of the mesangium a. Thickening of capillary walls 833) Type 2: extremely dense deposits in the glomerular basement membrane a. Poor prognosis 834) Hematuria, proteinuria, ↓ complement 835) Autoimmune disorders, infections, malignancies 836) What is the disorder that progresses into: 837) Fatigue, anemia, hypertension, edema, oliguria gradually worsening 838) Hematuria, proteinuria, glycosuria (tubular damage), many types of casts including broad and waxy casts 839) Markedly decreased GFR 840) What is Berger’s disease? What is the other name for this disease? 841) Acute onset from systemic shock (low blood pressure) or glomerulonephritis complication causes… 842) Name the causes of Nephrotic Syndrome 843) A patient with proteinuria would have how many g/day of protein in the urine? 844) What are the clinical findings for Minimal Change Disease (Lipid Nephrosis)? 845) This disease is similar to nephritic syndrome but affects only certain numbers and areas of glomeruli; podocytes are damaged 846) IgM and C3 immune deposits 847) Moderate to heavy proteinuria; microscopic hematuria 848) Heroin and analgesic abuse, HIV 849) This is an inherited sex-linked and autosomal disorder affecting basement membrane. 850) Males more severely affected 851) Macroscopic hematuria with respiratory infections by age 6 years 852) Membrane laminated with thinning; no immune complexes Name the disorder: • Type 1: increased cellularity in the subendothelial cells of the mesangium – Thickening of capillary walls • Type 2: extremely dense deposits in the glomerular basement membrane – Poor prognosis • Hematuria, proteinuria, ↓ complement • Autoimmune disorders, infections, malignancies What is the disorder that progresses into: • Fatigue, anemia, hypertension, edema, oliguria gradually worsening • Hematuria, proteinuria, glycosuria (tubular damage), many types of casts including broad and waxy casts • Markedly decreased GFR What is Berger’s disease? What is the other name for this disease? Acute onset from systemic shock (low blood pressure) or glomerulonephritis complication causes… Name the causes of Nephrotic Syndrome A patient with proteinuria would have how many g/day of protein in the urine? What are the clinical findings for Minimal Change Disease (Lipid Nephrosis)? This disease is similar to nephritic syndrome but affects only certain numbers and areas of glomeruli; podocytes are damaged • • IgM and C3 immune deposits Moderate to heavy proteinuria; microscopic hematuria • Heroin and analgesic abuse, HIV This is an inherited sex-linked and autosomal disorder affecting basement membrane. • Males more severely affected • Macroscopic hematuria with respiratory infections by age 6 years • Membrane laminated with thinning; no immune complexes • Mild to persistent hematuria, later nephrotic 55 UA PPT Flashcards 853) Mild to persistent hematuria, later nephrotic syndrome, renal failure for some 854) Patients with this disease have elevated serum uric acid and gout at an early age, occurs before renal symptoms. 855) Formerly Tamm-Horsfal protein is the only protein produced by the kidney 856) Inherited disorder that results in an abnormal buildup of uromodulin in the tubular cells causing their destruction 857) This is the most common cause of end-stage renal disease. 858) Glomerular basement membrane thickening 859) Increased proliferation of mesangial cells 860) Increased deposition of cellular and acellular material within matrix of Bowman’s capsule and around capillary tufts 861) Deposition associated with glycosylated proteins from poorly controlled diet 862) Sclerosis of vascular structure 863) Reason for early microalbumin testing 864) Describe Ischemia 865) Ischemia and Nephrotoxic agents such as aminoglycosides, amphotericin B, ethylene glycol, heavy metals, mushroom poisoning, hemoglobin, myoglobin can cause this___________. 866) This Hereditary and Metabolic disorder have these symptoms: 867) Generalized proximal convoluted tubule reabsorption failure a. Inherited with cystinosis and Hartnup disease b. Acquired: heavy metals, outdated tetracycline c. Complication of multiple myeloma, renal transplant d. Glycosuria and electrolyte imbalance 868) What are the two types of Nephrogenic Diabetes Insipidus syndrome, renal failure for some • • • Patients with this disease have elevated serum uric acid and gout at an early age, occurs before renal symptoms. Formerly Tamm-Horsfal protein is the only protein produced by the kidney Inherited disorder that results in an abnormal buildup of uromodulin in the tubular cells causing their destruction This is the most common cause of end-stage renal disease. • Glomerular basement membrane thickening • Increased proliferation of mesangial cells • Increased deposition of cellular and acellular material within matrix of Bowman’s capsule and around capillary tufts • Deposition associated with glycosylated proteins from poorly controlled diet • Sclerosis of vascular structure • Reason for early microalbumin testing Describe Ischemia Ischemia and Nephrotoxic agents such as aminoglycosides, amphotericin B, ethylene glycol, heavy metals, mushroom poisoning, hemoglobin, myoglobin can cause this___________. This Hereditary and Metabolic disorder have these symptoms: – Generalized proximal convoluted tubule reabsorption failure – Inherited with cystinosis and Hartnup disease – Acquired: heavy metals, outdated tetracycline – Complication of multiple myeloma, renal transplant – Glycosuria and electrolyte imbalance What are the two types of Nephrogenic Diabetes Insipidus 56 UA PPT Flashcards 869) Urine: pale yellow, low specific gravity (SG), possible negative results for other tests describes wheat disease? Urine: pale yellow, low specific gravity (SG), possible negative results for other tests describes wheat disease? 870) This affects only the reabsorption of glucose 871) Inherited as autosomal recessive 872) Decreased number of glucose transporters in tubules 873) Decreased affinity of transporters for glucose 874) Glycosuria with normal blood glucose level 875) In tubulointerstitial disease infections and inflammations affecting what? 876) What is the most common renal disease? 877) Urinary tract infection (UTI) is associated with 878) Is cystitis (bladder infection) common in tubulointerstitial disease? 879) Cystitis untreated progresses where? 880) What are the lab findings in cystitis? • • • • • This affects only the reabsorption of glucose Inherited as autosomal recessive Decreased number of glucose transporters in tubules Decreased affinity of transporters for glucose Glycosuria with normal blood glucose level the interstitium and the tubules urinary tract infection (UTI) tubulointerstitial diseases Yes, it is very common to upper urinary tract Many WBCs, bacteria, increased pH, mild proteinuria, hematuria 881) WBSs in urine are called pyuria 882) In acute pyelonephritis ascending emptying of bladder movement of bacteria affecting 883) In acute pyelonephritis ascending Calculi, pregnancy, reflux of urine from bladder to movement of bacteria is associated with ureters 884) What are the clinical signs of the acute Rapid onset, urinary frequency, burning, lower back pain pyelonephritis? 885) Differentiation between cystitis WBC casts. and pyelonephritis is aided by the ( In acute pyelonephritis WBC casts are present) presence of 886) Characteristics: more serious, Chronic pyelonephritis permanent damage to renal tubules, chronic renal failure, most often diagnosed in children: 887) Renal disorder that can affect Chronic pyelonephritis emptying of collecting ducts 888) Early urinalysis is similar to acute Chronic pyelonephritis pyelonephritis in 889) Microscopic results in chronic Later granular, waxy, and broad casts; increased protein, pyelonephritis are characterized by : hematuria, ↓ SG 890) Allergic reaction causing inflammation Acute interstitial nephritis of interstitium and tubules 891) Medication allergy to penicillin, Acute interstitial nephritis 57 UA PPT Flashcards methicillin, ampicillin, cephalosporins, NSAIDs, thiazide diuretics are associated with 892) Treatment for acute interstitial nephritis: 893) Urinalysis: Pyuria (pus: neutrophils), eosinophiluria, hematuria, proteinuria,↑ WBCs, WBC casts, no bacteria are the clinical manifestations of 894) In acute interstitial nephritis the stain used for eosinophils is 895) Renal failure can have two forms: 896) Chronic renal failure is 897) 898) Renal function tests: GFR <25 mL/min, ↑↑ BUN and creatinine levels, electrolyte imbalance, isosthenuria, proteinuria, and renal gycosuria are typically found in 899) In chronic renal failure urinalysis findings are characterized by 900) Acute renal failure is characterized by 901) Causes of acute renal failure: steroids Acute interstitial nephritis Hansel stain Acute and chronic forms progression from original disorders to end-stage renal disease chronic renal failure ↑ granular, waxy, broad casts Sudden onset, and often is reversible Decreased blood flow (prerenal), acute disease (renal), renal calculi and tumors (postrenal) 902) Urinalysis related to cause acute renal RTE cells = decreased blood flow failure: RBCs = glomerular damage WBCs and casts = infection/inflammation Urothelial cells = possible bladder tumor 903) Prerenal causes of acute renal Decreased blood pressure/cardiac output, hemorrhage, failure: burns, surgery, septicemia 904) Renal causes of acute renal failure: Acute glomerulonephritis, acute tubular necrosis, acute pyelonephritis, acute interstitial nephritis 905) Postrenal causes of acute renal Renal calculi, tumors, crystallization of ingested failure: substances 906) What is renal lithiasis? Renal calculi (kidney stones) in calyces and pelvis of kidney, ureters, bladder 907) What are the general characteristics Staghorn, round and smooth, barely seen of the renal calculi in renal lithiasis? 908) What are the clinical manifestations of Severe back pain radiating from lower back to legs when renal lithiasis? passing 909) How is renal lithiasis treated? By lithotripsy or surgical removal 910) What is lithotripsy? High-energy shock waves break up stones 911) How are the stones formed in renal Formation conditions similar to crystals; affected by lithiasis? pH, concentration, urine stasis. No exact cause of 58 UA PPT Flashcards formation is known 912) When is the occurrence of renal Increased in the summer because of dehydration lithiasis increased? 913) What types of stones are related to 75% calcium oxalate or phosphate renal lithiasis? Magnesium ammonium phosphate (stuvite) UTI and ↑ pH, like triple phosphate crystals Uric acid: increased purine diet Cystine: hereditary cystinosis 914) What neurotransmitter is produced from tryptophan? 915) Where is serotonin produced from tryptophan? 916) How is serotonin carried to muscles in the body? 917) What happens to excess serotonin in the body? 918) What would be an indicator of a tumor in the argentaffin cells of the intestine? 919) What kind of urine specimen can be used to test for 5-Hydroxyindoleacetic acid? 920) What foods should a patient avoid 72hours prior to a urine test for 5Hydroxyindoleacetic acid? 921) How should a 24-hour urine sample for 5-Hydroxyindoleacetic acid be preserved? 922) What is common of all cystine disorders? 923) What is an inherited disorder affecting renal reabsorption? 924) What amino acids are affected by cystinuria? 925) When are calculi formation seen in Cystinuria? 926) What is usually the only amino acid found during analysis of calculi from Cystinuria patients? 927) What urine screening test is used to screen for cystinuria? 928) What color is present if a cyanidenitroprusside urine screening test is positive? 929) What does a positive cyanidenitroprusside urine screening test Serotonin Intestinal argentaffin cells Platelets Excreted in the urine as 5-Hydroxyindoleacetic acid (5HIAA) Increased 5-HIAA in urine from excess serotonin production Random specimen Bananas, pineapples, tomatoes, phenothiazines, and acetanilids In HCl or boric acid noticeable sulfur odor Cystinuria Cystine, lysine and possibly arginine and ornithine Early in life Cystine cyanide-nitroprusside red-purple color excess cystine is present 59 UA PPT Flashcards indicate? 930) What are two possible causes of falsepositives on cyanide-nitroprusside urine screening? 931) What is the purpose of sodium cyanide in the cyanide-nitroprusside urine screening test? 932) What is the purpose of sodium nitroprusside in the cyanidenitroprusside urine screening test? 933) Which cystine disorder ranges in severity from a fatal disorder developed in infancy to a benign form appearing in adulthood? 934) What two categories can Cystinosis be broken down into? 935) What is the defect in Cystinosis? 936) Where can crystalline cystine deposits be found in cystinosis? 937) What causes Fanconi syndrome in cystinosis patients? 938) What are the symptoms of Cystinosis in a non-nephropathic patient? 939) What laboratory results would be consistent with Cystinosis? 940) What is the treatment option for patients with Cystinosis? 941) Which amino acid is affected in Homocystinuria? 942) What is the cause of Homocystinuria? 943) What symptoms can be seen in patients with Homocystinuria? 944) Which Cystine disorder is included in newborn screening programs? 945) What is the name for intermediate compounds in the production of heme? 946) What are the primary porphyrins? 947) What are a-aminolevulinic acid (ALA) and porphobilinogen precursors of? 948) Disorders in what stage of the heme pathway can be seen in urine? 949) In porphyrin disorders, where can coproporphyrin and protoporphyrin be detected? ketonuria and homocystinuria It reduces cystine color indicator cystinosis Nephropathic and non-nephropathic cystine cannot pass lysosomal membrane to be released into cytoplasm forming crystalline cystine deposits in the body cornea, bone marrow, lymph nodes and organs crystalline cystine deposits in renal tubules some ocular problems, otherwise benign aminoaciduria, reducing symptoms and cystine crystals Renal transplant and cystine-depleting medications Methionine a defect in metabolism of methionine, causing excess methionine failure to thrive, cataracts, mental retardation, thromboemboli, death Homocystinuria porphyrin uroporphyrin, coproporphyrin, protoporphyrin Porphyrins precursors; ALA, porphobilinogen, urobilinogen feces/bile 60 UA PPT Flashcards 950) If a patient has free erythrocyte protoporphyrin disorders from lead poisoning, where would this be detected? 951) What is the collective term for porphyrin disorders? 952) Which type of porphyria is caused by a missing gene in the metabolic pathway? 953) What clinical symptoms are seen in inherited porphyrias? 954) What are common ways that porphyrias can be acquired? 955) What can be seen on the diaper of a baby with a porphyria disease? 956) What test helps detect ALA and porphobilinogen in urine? 957) What happens to ALA during an Ehrlich reaction? 958) What is the name of a group of inherited disorders preventing the metabolism of glycoaminoglycans in the connective tissue? 959) What happens to polysaccharides in mucopolysaccharide disorders? 960) What substances found in urine are indicators of a mucopolysaccharide disorder? 961) What family of disorders do Hurler syndrome, Hunter syndrome and Sanfilippo syndrome fall under? 962) What is the treatment for mucopolysaccharidoses? 963) Which mucopolysaccharidosis causes corneal damage? 964) Which mucopolysaccharidosis is inherited as a sex-linked recessive trait? 965) What is a urinary screening test for Mucopolysaccharidoses? 966) What is a positive result on Metachromatic staining of a urine sample? 967) How long after adding Cetytrimethylammonium bromide to urine sample is the turbidity read? 968) For Mucopolysaccharide Paper test, what is filter paper dipped into before adding urine? In blood porphyrias inherited porphyria neurologic/psychiatric, cutaneous/photosensitivity or both lead poisoning, alcoholism, iron deficiency, chronic liver and renal disease port wine color after air exposure Ehrlich reaction It reacts with acetyl acetone to form porphobilinogen mucopolysaccharide disorders they are incompletely metabolized and accumulate in connective tisue dermatan sulfate, keratan sulfate, heparin sulfate Mucopolysaccharidoses bone marrow transplantation and gene therapy Hurler syndrome Hunter syndrome acid-albumin and cetyltrimethyammonium bromide turbidity test a blue color that cannot be washed away with dilute acidified methanol 5 minutes 0.59% azure A dye in 2% acetic acid 61 UA PPT Flashcards 969) Name a purine disorder. 970) What are the symptoms of Leschnyhan disease? 971) What is a symptom normally seen in the diaper of a baby with Lesch-nyhan disease? 972) What is the term for carbohydrate disorders that result in carbohydrates in urine? 973) Most meliturias do not cause problems except for? 974) Disorders in galactose-1-phosphate uridyl transferase (GALT) cause which carbohydrate disorder? 975) What disorder causes failure to thrive, severe mental retardation, cataracts and liver disorders? 976) What changes to diet can help sufferers of galactosuria? 977) When is Lactosuria usually discovered? 978) Fructosuria can be detected by which screening test? 979) When is Pentosuria usually discovered? 980) Overflow 981) Overflow can be described as Lesch-Nyhan disease motor defects, mental retardation, self-destruction, gout, renal calculi orange sand in diaper melituria galactosuria galactosuria Galactosuria removal of lactose During pregnancy or lactation Resorcinol screening test after ingestion of large amounts of fruit Disruption of a normal metabolic pathway over production of a normal or abnormal substance to the point that the tubules are not able to prevent it from escaping into the urine 982) Overflow is caused by inherited lack of specific enzyme for protein, fat, or carbohydrate metabolism—inborn error of metabolism 983) What happens in renal disorders? tubules fail to reabsorb substance 984) Overflow vs. renal disorders Overflow: increased levels in blood and urine Renal disorders: Increased levels seen in urine only 985) What is renal disorder? Malfunctions in the tubular reabsorption mechanism 986) Renal disorders classified by Inherited overflow functional defect: Acquired metabolic overflow Renal 987) Disorders caused by inherited overflow Phenylketonuria Tyrosinemia Maple syrup urine disease Organic acidemias Cystinosis Porphyria Mucopolysaccharidoses Galactosemia Lesch-Nyhan disease 62 UA PPT Flashcards 988) Disorders caused by acquired metabolic InfantileTyrosinemia overflow Melanuria 5-Hydroxyindole-acetic acid Porphyria 989) Disorders caused by renal defect Hartnup disease Cystinuria 990) Current state-mandated screening 30 or more detects how many inborn errors of metabolism? 991) What can Phenylalanine/Tyrosine Disorders can cause abnormal urinalysis results disorders cause? 992) What are the primarily follow-up tests Urine tests for inborn errors of metabolism? 993) Specimen collected for newborn heel stick blood screening is performed on 994) When is the newborn screening before infant leaves hospital at age of >24 hrs performed? 995) What appear first in the blood? Metabolites 996) How is the newborn screening by tandem mass spectrophotometry, MS/MS analyzed? 997) Phenylketonuria, tyrosyluria and Amino Acid Disorders (Aminoacidurias) alkaptonuria are 998) How often does Phenylketonuria 1 in 10,000 to 20,000 births (PKU) occur? 999) 1000) Phenylketonuria (PKU) is genetically Inherited autosomal recessive; heterozygotes normal classified as (must inherit 2 defective genes) 1001) What happens if phenylalanine is not Severe brain damage and mental retardation can occur reduced in the diet early in life? 1002) Milk contains what? Phenylalanine 1003) PKU management of disease Diet to eliminate phenylalanine (aspartame) 1004) In amino acid disorders such as PKU, Phenylalanine hydroxylase is missing there is an absence or deficiency of what enzyme? 1005) What are the testing methods for Urine test; Urine and 5% ferric chloride produces a phenylketonuria? permanent green-blue color 1006) Tyrosyluria causes what kind of Inherited or transiently acquired (metabolic defect) defect? 1007) How can newborns acquire Newborns may acquire tyrosyluria as their livers may be tyrosyluria? underdeveloped (Premature transient tyrosinemia) 1008) Hereditary defects are classified as Type 1, Type 2 and Type 3 1009) What enzyme deficiency is Type 1 Fumarylacetoacetate acid hydrolase defect? 1010) What are the clinical manifestations of Renal tubular disease and liver failure in infants Type 1 defect? 1011) What enzyme deficiency is Type 2 Enzyme deficiency is tyrosine aminotransferase defect? 63 UA PPT Flashcards 1012) What are the clinical manifestations of Type 2 defect? 1013) What enzyme deficiency is Type 3 defect? 1014) What are the clinical manifestations of Type 3 defects? 1015) What is used for tyrosyluria screening test? 1016) What is the second pathway for tyrosine? 1017) What is melanin? 1018) Melanin deficiency results in what? 1019) Increased levels of melanin are strongly suggestive of 1020) What is 5,6-dihydroxyindole? 1021) What is alkaptonuria? 1022) Black alkaline urine, possible blackstained diapers suggest 1023) How does alcaptonuria manifests later in life? 1024) How is alkaptonuria diagnosed? 1025) Branched chain amino acid disorders are 1026) What are the two groups of branched chain amino acid disorders? 1027) The newborn patients with branched chain amino acid disorders have what? 1028) What is the genetic classification of Maple syrup urine disease (MSUD)? 1029) What amino acid levels are elevated in blood and urine in MSUD? 1030) Characteristic odor to urine in maple syrup urine disease (MSUD): 1031) In MSUD, dietary regulation by day ___ shows good outcomes Corneal erosion and lesions on hands and feet Enzyme deficiency is p-hydroxyphenylpyruvate oxidase Mental retardation if no dietary restrictions (milk) Screening tests using MS/MS, and are available for tyrosinemia types 1, 2, and 3 Melanuria -Melanin, thyroxine, epinephrine, protein, and tyrosine sulfate Pigment for dark hair, skin Albinism malignant melanoma Dark urine; Initially a colorless precursor produced which is oxidized to melanogen (also colorless) and further oxidized to melanin (brown-black) Third major defect in the phenylalanine-tyrosine pathway. Enzyme deficiency, caused by a failure to inherit the gene to produce the enzyme homogentisic acid oxidase - used in catabolism of phenylalanine and tyrosine Alcaptonuria Brown pigment accumulates in blood, tissues, and urine. May lead to arthritis, liver, cardiac disorders. No mental retardation. Urine turns blue with ferric chloride, yellow precipitate with Clinitest, black with silver nitrate and ammonium hydroxide; quantitative tests available Amino acids with a methyl group that branches from the main aliphatic carbon chain; Leucine, isoleucine, valine Maple syrup urine disease (MSUD); early degradation products accumulate Organic acidemias; accumulation of organic acids further down in pathway positive ketones Inborn error of metabolism, autosomal recessive. Rare disease. leucine, isoleucine, and valine strong odor of maple syrup and thick, dark appearance 11 64 UA PPT Flashcards 1032) In maple syrup urine disease 2,4dinitrophenylhydrazine produces what? 1033) What is the procedure manual for 2,4Dinitrophenylhydrazine (DNPH) test? 1034) Organic acidemias are 1035) 1036) The symptoms for organic acidemias are: 1037) Three more common organic acidemias: 1038) How can be sovaleric, propionic, and methylmalonic acidemias detected? 1039) Increased urinary excretion of the metabolites indican and 5hydroxyindoleacetic acid (5-HIAA) characterize which disorders? 1040) This disorder can accompany various intestinal disorders 1041) Indicanuria is most often associated with which disease? 1042) What happens to Tyrptophan in indicanuria? 1043) In indicanuria, exposure of urine to air causing urine to turn to what color? 1044) Hartnup disease is known as 1045) Hartnup disease requires what dietary supplements? 1046) Inherited disorder that affects intestinal reabsorption of indole and renal tubular reabsorption = Fanconi syndrome 1047) What is the lining of the brain and spinal cord called? 1048) What is the outer layer of meninges called? 1049) Which layer of meninges touches the surface of the brain and spinal cord? 1050) What is the name of the middle meninges? 1051) Where is cerebrospinal fluid yellow precipitate turbidity 1. Place 1 mL of urine in a tube. 2. Add 10 drops of 0.2% 2,4-DNPH in 2N HCl. 3. Wait 10 minutes. 4. Observe for yellow or white precipitate. Other branched chain disorders include isovaleric, propionic, and methylmalonic aminoacidemias/acidurias. vomiting, metabolic acidosis, hypoglycemia, ketonurina, increased blood ammonia levels. Isovaleric acidemia - (isovaleryl co-enzyme A deficiency. Urine and sometimes patient smell like sweaty feet.) Propionic acidemia and Methylmalonic academia(no conversion of valine, threonine, methylmalonate to succinyl coenzyme A) by newborn screening programs using MS/MS Tryptophan disorders Tryptophan Disorders-Indicanuria Hartnup disease Tyrptophan is converted to indole in the gut, reabsorbed into the blood, excreted in the urine, which causing a bluish urine, or “blue diaper syndrome.” Indigo blue blue diaper syndrome Niacin Hartnup disease meninges dura mater pia mater arachnoid choroid plexuses of the four ventricles 65 UA PPT Flashcards produced? 1052) At what rate is CSF produced in a typical adult? 1053) How much CSF does a typical adult body contain? 1054) How much CSF is in a typical neonate? 1055) Between which layers can CSF fluid be found flowing? 1056) What happens to CSF in arachnoid granulations/villae? 1057) How is CSF formed? 1058) What is the blood-brain barrier composed of? 1059) How do molecules cross the bloodbrain barrier? 1060) Which structure prevents the transfer of chemicals and harmful substances into CSF? 1061) What are two diseases that disrupt the blood-brain barrier? 1062) Where is CSF typically collected from on a patient? 1063) Which department does the first tube of CSF from a spinal tap typically go to for testing? 1064) Why is the first tube from a spinal tap not used for microbiology testing? 1065) What is the determining factor for how much CSF should be taken out during a spinal tap? 1066) The following considered for specimen collection and handling of what type of body fluid? 1067) Usually STAT requests 1068) Handle carefully to avoid repeat taps 1069) Preservation 1070) The following preservation are used for specimen collection of what type of body fluid? 1071) Hematology 1072) Refrigerate 1073) Microbiology 1074) Room temperature 1075) Chemistry/serology 1076) Frozen 1077) What is appearance of CSF? 20 mL/min 90 to 150mL 10 to 60mL arachnoid and pia mater reabsorbed into blood selective filtration of blood very tight-fitting endothelial cells active transport blood-brain barrier meningitis and multiple sclerosis between third to fifth lumbar vertebrae Chemistry/serology possibility of skin contamination in first tube based on patient volume and opening pressure CSF CSF Crystal clear, cloudy/turbid, milky, xanthochromic, hemolyzed/bloody 66 UA PPT Flashcards 1078) In CSF body fluid Cloudy = ---------; and milky = -------1079) The following are appearance of what type of CSF which is seen in particular medical condition. 1080) Pink, orange, yellow 1081) RBC degradation products 1082) Also jaundice, ↑ ↑ protein, carotene 1083) Pathologic = cerebral hemorrhage Infection-Lipid or protein 1084) Define traumatic tap in collecting CSF 1085) True or false 1086) Traumatic tap Differentiates from cerebral hemorrhage 1087) How we can differentiate between a traumatic tap and a subarachoid hemorrhage? Blood vessel punctured during tap True 1088) Clots present in traumatic tap or hemorrhage? 1089) damage to blood-brain barrier is defined as 1090) web-like pellicle after refrigeration is seen in what type of infection? 1091) Is clot formed in Nonbloody CSF and TB meningitis? 1092) The following are characteristics of what term of CSF? 1093) Not present in a recent traumatic tap 1094) Indicates older hemorrhage 1095) D-dimer test for hemorrhage 1096) How often RBC cell count in CSF? 1097) Why STAT test should be done immediately? 1098) Normal adult ------- WBCs/µL 1099) Neonates -------- mononuclear cells/µL 1100) What type of cell counters can be used in Neubauer counting chamber? 1101) What system is used for body fluid counting? 1102) What is formula for Standard Neubauer calculation (cells/µL)? 1103) True or False 1104) Standard Neubauer calculation formula (cells/µL) Can be used for diluted and undiluted samples Xanthochromic Uneven blood distribution in tubes with traumatic tap Erythrophagocytosis, hemosiderin granules Hemorrhage = even distribution in all tubes Traumatic tap = decreasing tubes 1 through 3 Clots present = traumatic tap (plasma) Hemorrhage does not have enough fibrinogen Nonbloody CSF TB meningitis yes Xanthochromia seldom Because Granulocytes lyse within 1 hour 0 to 5 Up to 30 Automated cell counters Body fluid specific automation Number of cells counted × dilution Number of cells counted × volume of 1 square = cells/µL True 67 UA PPT Flashcards 1105) Give an example of calculating CSF cells count 1106) Following are considered in what cell count? 1107) Clear specimens count undiluted unless overlapping cells are seen. 1108) Load with transfer pipette. 1109) Dilute with normal saline if necessary. 1110) What is the diluting solution for a manual WBC count? 1111) The following are considered to be done for what blood cell count? 1112) undiluted rinse transfer pipette with acetic acid, gently rotate pipette 1113) ----------stain helps to see WBCs 1114) What controls are available for spinal fluid RBC and WBC? 1115) How often all diluent should be checked for contamination? 1116) How often cytocentrifuge speed and timing should be checked? 1117) The following are sterilize of what type of counting chamber 1118) Soak chambers in bactericidal solution for 15 minutes; rinse; clean with isopropyl alcohol 1119) Why identifying the type or types of cells present in the CSF is valuable? 1120) True or False 1121) The differential count on CSF should be performed on a stained smear and the cells in counting chamber. 1122) Why specimen should be concentrated prior to the preparation of the smear? 1123) What method are available for specimen concentration? 1124) When the differential count is performed for CSF count------- cells should be counted, classified, and reported in terms of ---------1125) The following is the principle of--------for CSF differential count 1126) Forces cells onto a slide in a monolayer 1127) Filter paper absorbs moisture cells counted × dilution × 1 μL cells/µL 1 μL (0.1 × 10) (volume counted) </exeq) Total cell count = 3% acetic acid WBC count Methylene blue Liquid commercial control Every two weeks monthly Nondisposable chamber It is diagnostic aid False It should be done only in stain smear. To ensure the maximum number of cells are available for examination Sedimentation, filtration, centrifugation, and cytocentrifugation 100- percentage Cytocentrifugation 68 UA PPT Flashcards a. mL CSF to 1 drop 30% albumin 1128) Positively charged slides to attract cells 1129) Albumin -------- the cell yield and ------the cellular distortion. 1130) In cytocentrifugation ------- control of 0.2 mL ------- and two drops of ------stained for bacterial contamination. 1131) What type of cells found in normal CSF? 1132) Does adult have more lymphocyte or monocyte? What is the ratio? 1133) What is the ratio for children? 1134) True or False 1135) Occasional neutrophils are normal in CSF 1136) increased amounts of normal cells is defined as: 1137) What is associated with determining the cause of meningitis? 1138) Increase number of neutrophil indicate what type of meningitis? 1139) High percentage of Lymphocytes is considered indicative of what type of meningitis? 1140) Following are associated with what type of CSF cell? 1141) Primarily in bacterial meningitis 1142) Often contain phagocytized bacteria 1143) Increased early viral, fungal, tubercular, parasitic 1144) Vacuoles may be present 1145) This cell is seen with bone marrow contamination from tap in 1% of specimens 1146) ------------- may resemble NRBCs 1147) What structure and cells may be seen following traumatic tap? 1148) Reactive lymphocyte are frequently present during ---------1149) --------- has 50 or fewer lymphocytes/μL, both normal and reactive 1150) Increased lymphocytes are seen in cases of -----------,----------1151) Increased eosinophils is associated with what infections? Increase- decrease Daily-saline-albumin Normal lymphocytes and monocytes Adult usually has predominate of lymphocyte normal lymphocytes: monocytes = 70:30 It is reversed of adult ratio True Pleocytosis Pleocytosis of normal cells Bacterial meningitis viral, tubercular, fungal, parasitic meningitis neutrophil Nucleated RBCs (NRBC) Neutrophils with pyknotic nucleii Capillary structures and epithelial cells Viral infection. Multiple sclerosis HIV infection and AIDS Parasitic and fungal infections (primarily Coccidioides immitis) 69 UA PPT Flashcards 1152) Introduction of foreign material, including medication and shunts into the CSF causes to increase of what cells? 1153) What is the purpose of macrophages in the CSF? 1154) What type of cells might be seen following repeated taps? 1155) Increasing of what type of cells is an indicative of a previous hemorrhage? 1156) This cells type appear within 2 hours to phagocytize RBCs 1157) Define unconjugated bilirubin 1158) When nonclinically significant cells are seen? 1159) The following belong to pathologically or nonpathologically significant cells? 1160) Choroidal cells 1161) Epithelial lining of choroid plexus, singular and in clumps, uniform cells 1162) Ependymal cells lining ventricles and neural canal; less defined cell membranes in clumps 1163) Spindle cells lining arachnoid seen in clumps 1164) What are malignant cells of hematologic origin in CSF? 1165) These cells are seen in CSF as a serious complication of acute leukemias. 1166) ------------may be more prominent than in blood smear. 1167) --------- cells are also seen in the CSF indicating Dissemination from lymph organs and nuclei may appear 1168) Cleaved and prominent nucleoli are present. 1169) What are the two types of malignant cells of nonhematologic origin? 1170) What are two reasons for abnormal CSF test relults? 1171) In the cerebrospinal protein test, what are the normal values for total protein? 1172) What is the significance of elevated levels of cerebrospinal protein? 1173) What are the two primary methodologies for testing CSF? eosinophils remove cellular and other debris Macrophages Macrophages Macrophages RBCs degraded to hematoidin crystals representing unconjugated bilirubin Seen after diagnostic procedures Nonpathologically significant cells Lymphoblasts, monoblasts, and myeloblasts Lymphomas Lymphoblasts, monoblasts, and myeloblasts Nucleoli Lymphoma Metastatic carcinoma cells Primary tumors Alterations in the permeability of the blood-brain barrier. Increased production or metabolism by the neural cells in response to a pathologic condition. 15 to 45 mg/dL damage to blood-brain barrier, IG production within CNS, decreased clearance, degeneration of neural tissue Turbidity Automated instrumentation 70 UA PPT Flashcards 1174) Name five reasons for calculating protein fractions. 1175) What is the equation for IgG index? 1176) What is the purpose of electrophoresis as an immunophoretic technique? 1177) What is the electrophoresis result for Multiple Sclerosis? 1178) What is the significance of Myelin basic protein? 1179) What is the significance of CSF glucose? 1180) Name two causes of decreased CS glucose. 1181) What is the clinical significance of CSF Lactate? 1182) Why is CSF Glutamine tested? 1183) What type of CSF sample is used in Microbiology tests? 1184) Latex agglutination tests are available for: 1185) Where is the parasite Naegleria fowleri found? 1186) What is the primary reason for serologic testing of CSF 1187) Name four areas specialized in clinical Andrology. Comparisons between serum and CSF levels of albumin and IgG CSF/serum albumin index Blood-brain barrier integrity CSF IgG index Comparison of the CSF/serum albumin index with the CSF/serum IgG index Values for CSF albumin and globulin adapted for automated instruments CSF IgG (mg/dL)/serum IgG (g/dL) CSF albumin (mg/dL)/serum albumin (g/dL) Detection of oligoclonal bands no bands in serum, bands in CSF Presence in CSF indicates demyelination of myelin sheath around axons of neurons Values that are decreased relative to plasma values Elevated CSF glucose values are always a result of plasma elevations bacterial meningitis Tubercular meningitis Diagnosis and management of meningitis Bacterial, TB and fungal levels >25 mg/dL Viral <25 mg/dL More reliable than CSF glucose Levels remain elevated until treatment becomes effective, then fall rapidly Can result from any condition that decreases oxygen flow to the tissues Monitor severe head injuries Indirect test for the presence of excess ammonia in the CSF Gram stain and cultures must be performed on sediment from centrifuged CSF Group B streptococcus, Haemophilus influenzae, S. pneumocystis Neisseria meningitidis, and Escherichia coli ponds, lakes, and some pools Primary test is for neurosyphilis, third stage Assisted reproductive technology (ART) Abnormal results on the routine semen analysis Specialized andrology laboratories Fertility testing In vitro fertilization (IVF) 71 UA PPT Flashcards 1188) List the four components for semen. Testes and epididymis Seminal vessels Prostate Bulbourethral glands 1189) What are the functions of the seminal vessels? Produce majority of fluid (60% to 70%); transport medium Provide fructose and flavin for sperm metabolism Sperm are not motile without this fluid 1190) What are the physiological processes in the prostate gland? Produce acidic fluid (20% to 30%) Contains acid phosphatase, citric acid, zinc, and proteolytic enzymes Enzymes coagulate semen prior to ejaculation and cause liquefaction after ejaculation 1191) Why must a semen sample be a complete specimen? First portion of the ejaculate is missing, then -Sperm count will be decreased -pH is falsely increased -Specimen will not liquefy Last portion of ejaculate is missing, then -Semen volume is decreased -Sperm count is falsely increased -pH is falsely decreased -Specimen will not clot 1192) What is the recommendation from the The WHO recommends that two or three samples be WHO in regards to semen collection? collected not less than 7 days or more than 3 weeks apart? 1193) For home semen collection when Deliver to the laboratory within 1 hour; keep specimen at should the specimen be delivered and to 37 degrees C the laboratory and what temperature should the specimen be kept at? 1194) What three things should be recorded - Patient name and date of birth in regards to semen specimen - Period of abstinence collection? Time of collection and receipt 1195) How should a semen specimen be a) Collected by masturbation collected? 1196) What three things should be kept in • Standard precautions must be observed at all mind in regards to semen specimen times during analysis. handling? • Specimens are discarded as biohazardous waste. b) Sterile materials and techniques must be used. 1197) These eight things are measured in a a) Macroscopic/microscopic, appearance, volume, fertility evaluation: viscosity, pH, sperm concentration and count, motility, and morphology 1198) What is the normal color of semen? b) Normal is gray-white, translucent 72 UA PPT Flashcards 1199) What is the normal odor of semen? 1200) What indicates an infection in a semen sample? What two things should be done to verify? 1201) What does a red appearance indicate in a semen sample? 1202) What does a yellow appearance indicate in a semen sample? 1203) What results from urine contact with semen? 1204) Slide 16…. 1205) What’s the normal volume of a semen specimen? 1206) What is the effect of extended abstinence on semen volume? 1207) How is the volume of a semen sample measured? 1208) What could cause a decrease in volume in semen? 1209) What is a normal viscosity appearance? 1210) What qualifies as a highly viscous semen sample? 1211) What is the rating system for viscosity of semen? 1212) When should the pH be measured for a semen sample? 1213) What is the normal pH of semen? 1214) What pH of semen indicates an infection? 1215) What three things could result in a decrease in pH in semen? 1216) How is semen pH measured? 1217) Sperm concentration and count is a valid measurement of what? 1218) What is the formula for sperm concentration? 1219) What is sperm count? 1220) What is the formula for total sperm count? 1221) What is the reference value for sperm count? 1222) What is considered borderline for sperm count? 1223) What is the formula for normal count for sperm? 1224) What’s the normal count of sperm? c) Musty odor d) White turbidity; culture and LE reagent strip e) Blood cells, abnormal f) Urine, prolonged abstinence, medications g) Urine is toxic to sperm resulting in no motility h) i) 2 to 5 mL j) Increased volume may be seen following periods of extended abstinence k) In a graduated cylinder l) Infertility, incomplete collection m) Droplets with thin threads from a pipette are normal n) Form threads longer than 2 cm are highly viscous o) Rate 0 (watery) to 4 (gel-like) or low, normal, high p) Measure within 1 hour of ejaculation q) Normal: 7.2-8.0 r) Over 8.0 s) Increased prostate fluid, ejaculatory duct obstruction, or poorly developed seminal vesicles t) Check with pH pad of a urinalysis reagent strip u) Fertility v) Concentration= number sperm/mL w) Count= number sperm per ejaculate x) Sperm concentration x specimen volume y) >20 to 250 million sperm per milliliter z) 10-20 million aa) Concentration x volume bb) >40 million/ejaculate 73 UA PPT Flashcards 1225) What is used to count sperm concentration? 1226) What does Neubaur chamber consist of? 1227) What is the common dilution for Neubaur chamber? 1228) What is the diluting fluid for Neubaur chamber? 1229) How are sperm counted using Neubaur chamber? 1230) What is the multiplication factor for sperm concentration? 1231) What is the formula for sperm count? 1232) For sperm motility, sperm should display this movement: 1233) For sperm motility how should the specimen be prepped and what is the time in which the specimen should be examined? 1234) How many fields should be used to evaluate sperm motility? 1235) Instead of counting sperm per HP field, this alternative can be used: 1236) For sperm motility, how should grading be done? 1237) What’s the minimum motility acceptable for sperm motility? 1238) How is sperm motility graded by the World Health Organization (WHO)? 1239) What instrumentation is available for sperm motility analysis? 1240) True/False: 1241) Sperm morphology is critical to fertilization: 1242) What four things should be evaluated in sperm morphology? 1243) What are the classic characteristics of the head of a sperm? 1244) How long is the neckpiece of a sperm what two things does it attach too? 1245) What is the midpiece of the sperm cc) Performed in Neubauer chamber dd) Five small squares, corners, and center of large center square ee) 1 to 20 ff) Sodium bicarbonate and formalin, must immobilize sperm gg) Count both sides of chamber, sides must agree within 10%; use the average; multiply sperm counted by 1,000,000=sperm/mL hh) Must multiply sperm per uL by 1000 to reach sperm/mL ii) Sperm/mL x volume jj) Forward, progressive movement kk) Well-mixed, liquefied semen specimen; examine within 1 hour, undiluted on glass slide with cover slip ll) Progressive, forward motion in 20 HP fields mm) Examine 200 sperm per slide and count the percentages of the different motile categories using a manual cell counter nn) Using a scale of 0 to 4, with 4 indicating rapid, straight-line movement and 0 indicating no movement oo) A minimum of 50% with a rating of 2.0 after 1 hour is considered normal pp) Motility is graded as progressive motility (PM), nonprogressive motility (NP), and immotility (IM); motility must be specified as total motility (PM and NP) or progressive motility (PM) qq) Computer-assisted semen analysis (CASA) rr) True ss) Head, neck, midpiece, tail tt) Oval with acromosal cap at end and covering half of the head; 5um long and 3 um wide; contains enzymes for ovum penetration uu) 7.0 um long; attaches head to midpiece and tail vv) Sheath of mitochondria for tail movement 74 UA PPT Flashcards surrounded by? 1246) How long is the flagellar tail? 1247) What magnification should be used to observe sperm morphology? 1248) Which three stains can be used for sperm morphology? 1249) How many sperm morphology should be counted? 1250) What are the abnormalities in head sperm structure? 1251) What are the abnormalities in sperm tail structure? 1252) What three things are included with Kruger’s criteria is sperm morphology? ww) 45 um xx) Observe on thin smear under oil immusion yy) Wright’s, Giemsa, Shorr, or Papanicolaou Count 200 and report number of abnormal zz) Double heads, giant and amorphous heads, pinheads, tapered heads, and constricted heads Abnormal sperm tails are frequently doubled, coiled, or bent Measuring head, neck, and tail size Measuring acrosome size Evaluating for the presence of vacuoles 1253) Why is important to have strict criteria Strict criteria evaluation is an integral part of assisted in sperm morphology evaluation? reproduction evaluations 1254) >? % normal forms when using routine 30% criteria: 1255) >?% normal forms when using strict 14% critieria: 1256) What are three thing that should be White blood cells (WBCs) and spermatids (immature considered when calculating round sperm) bodies? Differentiate on morphology smear Count number of each separately in 100 cells 1257) What is the formula used in sperm C= (N x S)/100 morphology round body calculation? 1258) What does N represent in the round N is the number of spermatids or neutrophils counted bodies formula? per 100 mature sperm 1259) What does S represent in the round S is the sperm concentration in millions per milliliter bodies formula? 1260) What’s the normal value of round Normal: <1,000,000 bodies in sperm morphology? 1261) What is the stain used in sperm Eosin-nigrosin stain vitality? 1262) What color do normal cells stain and Dead cells stain red; normal are blue-white what color do dead cells stain? 1263) What formula is used in sperm Count number/100 cells vitality? 1264) What is the normal percentage in Normal: 75% living sperm vitality? 1265) What does sperm vitality correspond Motility to? 1266) What test is sperm vitality used in? Seminal fructose tests 1267) Seminal fluid fructose test can be Low sperm concentration; low to absent fructose level in useful in evaluating these three things? the semen, lack of the support medium 1268) Which 5 things are considered for lack Abnormalities of the seminal vesicles 75 UA PPT Flashcards of support medium in the seminal fluid fructose test? 1269) Ture/False: 1270) Anitsperm antibodies are present in both men and women: 1271) When are antisperm antibodies more commonly seen in men? 1272) How does the immune system see sperm? 1273) What is the result of damaged sperm? 1274) When should antibodies be suspected in regards to male and female samples? 1275) How are female samples prepared for antisperm antibodies? 1276) What method category is used for antisperm antibodies in males? 1277) What is a specific test used in antisperm antibodies analysis, and how does that method work? 1278) What is the normal result in antisperm antibodies? 1279) What does the immunobead test demonstrate? 1280) What are bead coated with in the immunobead test? 1281) What does microscopic examination show in the immunobead test? 1282) What is the function of the head and the tail? 1283) What is the normal for antisperm antibodies? 1284) What indicates a prostate infection in a semen sample? 1285) If >1 million WBCs are found what three organisms are tested for? 1286) What chemistry tests are done and what does a decrease in each indicate? Bilateral congenital absence of the vas deferens Obstruction of the ejaculatory duct Partial retrograde ejaculation Androgen deficiency True Surgery, vasectomy reversal, trauma Sperm normally do not encounter the immune system, so body considers them foreign Damaged sperm create female antibodies Suspect male antibodies when clumps of sperm are seen; female no clumping Mix female serum with sperm and check for agglutination Immunoassay Mixed agglutination reaction (MAR) test – Incubate sperm with antihuman globulin (AHG) and IgG-coated latex particles AHG combines with particles and antibody-coated sperm forming clumps <10% motile sperm attach to particles Demonstrates antibodies to head, neck, midpiece, and tail Antihuman globulin Microscopic examination shows where on sperm antibodies are attacking Tail= movement Head= penetration Normal: beads on <20% of sperm >1 million WBCs Culture and test for Mycoplasma hominis, Chlamydia trachomatis, Ureaplasma urealyticum neutral α-glucosidase, zinc, citric acid, acid phosphatase – ↓ Neutral α -glucosidase = epididymis ↓ Zinc, citric acid, acid phosphatase =↓ prostatic fluid >/= 20 mU/ejaculate 1287) What is the normal neutral aglucosidase value for semen? 1288) What is the normal Zinc value for >/= 2.4 umol/ejaculate semen? 1289) What is the normal citric acid value for >/= 52 umol/ejaculate 76 UA PPT Flashcards semen? 1290) What is the normal acid phosphatase value for semen? 1291) Synovial fluid functions as _____ 1292) Synovial fluid supplies nourishment to _____ 1293) Crystals that are found in synovial fluid during attacks of gout are most likely: 1294) Synovial fluid is produced by: 1295) What are the classifications of disorders (arthritis) 1296) Is Lupus Erythematosus (LE) inflammatory or noninflammatory? 1297) What type of disorder ‘microbial infection’ is? 1298) The concentration of which chemicals found in synovial fluid differs most noticeably from the plasma concentration? 1299) A turbid synovial fluid with yellowgreen color indicates: 1300) Can Neutrophils be seen in normal synovial fluid? 1301) Can ‘increased ingestion of dairy products’ cause crystals to be present in the synovial fluid? 1302) A cloudy, yellow-green synovial fluid with 100,000 white blood cells (WBCs), a predominance of neutrophils, and a decreased glucose should be classified as: 1303) What is the normal knee fluid amount level, if inflamed? 1304) Are normal and diseased, both fluids clot? 1305) A turbid synovial fluid with clear and pale yellow (egg white) color indicates: 1306) Synovial fluid functions as _____ 1307) Synovial fluid supplies nourishment to__ 1308) Crystals that are found in synovial fluid during attacks of gout are most likely: 1309) Synovial fluid is produced by: 1310) What are the classifications of >/= 200 units/ejaculate Lubrication for the movable joints: diarthroses cartilage Monosodium urate Ultrafiltration of plasma Noninflammatory; Inflammatory; Septic; and Hemorrhagic Inflammatory Septic Protein Infection No No Septic 3.5 mL - >25 mL No. diseased fluid clots, while normal fluid does not Normal Lubrication for the movable joints: diarthroses cartilage Monosodium urate Ultrafiltration of plasma Noninflammatory; Inflammatory; Septic; and 77 UA PPT Flashcards disorders (arthritis) 1311) Is Lupus Erythematosus (LE) inflammatory or noninflammatory? 1312) What type of disorder ‘microbial infection’ is? 1313) The concentration of which chemicals found in synovial fluid differs most noticeably from the plasma concentration? 1314) A turbid synovial fluid with yellowgreen color indicates: 1315) Can Neutrophils be seen in normal synovial fluid? 1316) Can ‘increased ingestion of dairy products’ cause crystals to be present in the synovial fluid? 1317) A cloudy, yellow-green synovial fluid with 100,000 white blood cells (WBCs), a predominance of neutrophils, and a decreased glucose should be classified as: 1318) What is the normal knee fluid amount level, if inflamed? 1319) Are normal and diseased, both fluids clot? 1320) A turbid synovial fluid with clear and pale yellow (egg white) color indicates: 1321) An arthrocentesis is performed on a patient with lupus erythematosus that produces a cloudy yellow fluid with 2000 WBCs, of which 55% is neutrophils. This fluid should be classified as: 1322) A clear, pale yellow synovial fluid with good viscosity and a WBC count of 1000 should be classified as: 1323) To determine if an unknown fluid is synovial fluid, the fluid can be tested: 1324) In the Ropes’ or mucin clot test, normal synovial fluid forms a solid clot when added to: 1325) The recommended diluting fluid for synovial fluid cell counts is: 1326) To perform a cell count on highly viscous synovial fluid, what type of filter paper need to be used? Hemorrhagic Inflammatory 1327) On highly viscous synovial fluid, to Count all nine large squares Septic Protein Infection No No Septic 3.5 mL - >25 mL No. diseased fluid clots, while normal fluid does not Normal Inflammatory Noninflammatory By adding acetic acid and observing clot formation 2% to 5% glacial acetic acid Normal saline/methylene blue Moist filter paper using line petri dish 78 UA PPT Flashcards count less than 200 WBCs/μL: 1328) On highly viscous synovial fluid, to count greater than 200 WBCs/μL in the above count: 1329) In differential count, how to incubate? 1330) Vacuolated macrophages containing ingested neutrophils seen in synovial fluid are called: 1331) Neutrophils with small, dark granules containing RA factor (IgM) see in synovial fluid are called: 1332) Crystal examination is done in the cases of: 1333) Crystals frequently seen in patients’ joints with chronic inflammation are: 1334) In crystal examination, what is the initial examination? 1335) Crystal may be seen in: 1336) Synovial fluid for crystal examination should be: 1337) Crystals that appear to be needle shaped; seen intra- and extracellularly; may be seen sticking through cytoplasm are: 1338) Crystals that appear to be rhombic, square shaped, or short rods; often seen in vacuoles of neutrophils are: 1339) Which crystal is highly birefringent and appears brighter than CPPD? 1340) Compensated Polarized Light align _____ crystals with slow vibration 1341) What color does MSU molecules produce under compensated light? 1342) In which axis, CPPD molecules run under compensated light? 1343) Synovial fluid protein is normal when: 1344) Mention two types of most common autoimmune causes of arthritis: 1345) What is the reference value for the upper limit of synovial fluid volume? 1346) What should the color of synovial fluid be? 1347) What should the clarity of synovial fluid be? 1348) What should the viscosity of synovial fluid be? 1349) What is the reference value of the Count the four corner squares; and the five small squares used for a RBC count Incubate with hyaluronidase, then cytocentrifuge Reiter’s cells/neutrophages Ragocytes (RA cells) Acute and chronic cases; metabolic disorders; and decreased renal functions Cholesterol Initial examination is wet preparation unstained under low and high power Differential Examined unstained under direct and red compensated polarized light MSU crystals CPPD crystals MSU Crystals Yellow color (negative birefringence) CPPD molecules run perpendicular to long axis Less than 3 g/dL RA and LE < 3.5 mL Colorless to pale yellow Clear Able to form a string 4-6 cm long < 200 cells/µL 79 UA PPT Flashcards leukocyte count in synovial fluid? 1350) What is the reference value for the amount of neutrophils in the WBC differential? 1351) What is the reference value for the amount of crystals that should be present in synovial fluid? 1352) What is the reference value for glucose in synovial fluid? 1353) What is the reference value for total protein in synovial fluid? 1354) List 3 things infections in synovial fluid can be caused by. 1355) What microbiology stain is routinely performed on synovial fluid? 1356) Culturing microbiological infections of synovial fluid require what agar? 1357) List 4 primary organisms typically involved in synovial fluid infection: 1358) In microbiology tests for synovial fluid, fungal and Tuberculosis (TB) cultures are determined by: 1359) Why are the majority of serologic tests performed on serum and synovial fluid? 1360) What are the most common autoimmune causes of arthritis? 1361) Arthritis is a frequent complication of this disease: 1362) In patients suspected with Lyme Disease, serum should be tested for what antibodies? 1363) What two serologic tests can be done to assess the extent of inflammation in synovial fluid? 1364) What is the purpose of serous fluid? 1365) The ultrafiltrate of plasma forms: 1366) In the capillaries lining the membranes, serous fluid is formed due to what 2 pressures? 1367) Normally, oncotic pressure on both sides of the membrane are: 1368) What type of pressure primarily causes the production of serous fluid? 1369) Small amounts of excess serous fluid are absorbed by what type of < 25% of the differential None should be present < 10mg/dL lower than the blood glucose plasma difference < 3g/dL Inflammation, trauma and systemic infections Gram stain Chocolate agar Staphylococcus, Streptococcus, Haemophilus influenzae, and Neisseria gonorrhoeae Patient history To serve as confirmatory tests RA (Rheumatoid Arthritis) and LE (Lupus Erythematosus) Lyme disease Borrelia burgdorferi Test for C-reactive protein and fibrinogen To provide lubrication between the two membranes (parietal and visceral) Serous fluid Hydrostatic and oncotic (protein) pressure same Hydrostatic pressure Lymphatic capillaries 80 UA PPT Flashcards capillaries? 1370) What term is used to describe the disruption of serous fluid formation or reabsorption that causes fluid buildup 1371) List 6 causes of serous fluid effusion 1372) How is congestive heart failure, salt and fluid retention a pathological cause of effusion? 1373) How is nephrotic syndrome, hepatic cirrhosis, malnutrition or protein-losing enteropathy a pathological cause of effusion? 1374) How is are microbial infections, membrane inflammations or malignancy a pathological cause of effusion? 1375) How are malignant tumor, lymphomas, infection and inflammation or thoracic duct injury a pathological cause of effusion? 1376) How is serous fluid collected? 1377) Serous fluid is collected in what cavities? 1378) How much serous fluid should be collected? 1379) Serous fluid collected in an EDTA tube goes to what department? 1380) Serous fluid collected in heparinized or plyanethol sulfonate (SPS) tube goes to what departments? 1381) Clotted or heparinized serous fluid should be tested by what departments? 1382) When should serous fluid be kept on ice? 1383) For serous fluid being tested by microbiology or cytology departments, fluid should be concentrated how? 1384) Chemical tests for serous fluid are compared with tests are compared to what other type of test? 1385) The primary classification of serous fluids involve what 2 categories? 1386) Systemic disorders disrupting filtration and reabsorption, congestive heart Effusion Hydrostatic pressure increased from congestive heart failure, Oncotic pressure decreased from hypoproteinemia, Increased capillary permeability from inflammation, Infection, Malignancy, Lymphatic obstruction from tumors Increased capillary hydrostatic pressure disrupts mechanisms of serous fluid formation and reabsorption. Decreased oncotic pressure disrupts mechanisms of serous fluid formation and reabsorption. Increased capillary permeability disrupts mechanisms of serous fluid formation and reabsorption. Lymphatic obstruction disrupts mechanisms of serous fluid formation and reabsorption. Needle aspiration Pleural cavity (Thoracentesis), Heart cavity (Pericardiocentesis), and Peritoneal cavity (Paracentesis) Abundant fluid should be collected > 100mL Hematology Microbiology, Cytology Chemistry, Serology For specimens being tested for pH Centrifuging 100mL Blood tests drawn at the same time Transudates and Exudates Transudates 81 UA PPT Flashcards failure or nephrotic syndrome cause what category of serous fluid? 1387) Conditions affecting membranes, inflammation, infection or malignancy cause what category of serous fluid 1388) Which requires little further testing? Transudates or Exudates? 1389) Differentiation of transudates and exudates is important for: 1390) Which are seldom tested further? Transudates or exudates? 1391) Microbiology, cytology and tests for general symptoms for transudates or exudates? 1392) Differentials are routinely performed on what type of serous fluid specimens? 1393) Differentials performed on cytocentrifuged serous fluid specimens involve looking at what 3 types of cells? 1394) Additional tests to differentiate transudate versus exudate uses pleural fluid cholesterol. Transudates and exudates will have what values? 1395) Additional tests to differentiate transudate versus exudate uses fluidserum cholesterol ratio. Transudates and exudates will have what values? 1396) Additional tests to differentiate transudate versus exudate uses serumbilirubin ratio. Transudates and exudates will have what values? 1397) Normal pleural fluid should appear: 1398) Turbid pleural fluid indicates: 1399) Milky pleural fluid indicates: 1400) Bloody pleural fluid indicates: 1401) How is hemothorax and membrane damage differentiated using pleural fluid? 1402) How is a chylous and pseeudochylous differentiated? 1403) In hematology differentials of serous fluid, what are the 7 types of cells can be observed? 1404) Which type of cells are the highest Exudates Transudates Further testing Transudates Exudates Cytocentrifuged specimens WBCs, normal tissue cells, and malignant cells Pleural fluid cholesterol <60 mg/dL versus >60 mg/dL Fluid-serum cholesterol ratio <0.3 versus >0.3 Fluid-serum bilirubin ratio <0.6 versus >0.6 Clear, pale yellow WBCs, inflammation, infection Chylous material from thoracic duct leakage, pseudochylous material from chronic inflammations Hemothorax (trauma), hemorrhagic effusion (membrane) damage Do a hematocrit on pleural fluid; >50% blood HCT is a hemothorax (more blood), while membrane damage will have low blood Sudan III stain will show chylous, which is triglycerides, while pseudochylous is cholesterol and will polarize and show crystals in a wet bright-field view Neutrophils (primary), lymphocytes, macrophages, eosinophils, mesothelial cells, plasma cells and malignant cells Macrophages (scavengers) 82 UA PPT Flashcards number in hematology differentials of serous fluid? 1405) Increased neutrophils in serous fluid indicates: 1406) Increased lymphs in serous fluid indicates: 1407) Eosinophils may be seen in serous fluid in what circumstances? 1408) What cells may be multinucleated in a serous fluid observation? 1409) What type of cell is described: Single cell layer lines membranes, common to see in serous fluid, pleomorphic, dark blue cytoplasm, round nuclei, normal and reactive; has a “fried egg appearance” 1410) A lack of mesothelial cells is significant in what disease and why? 1411) List the primary cancer cells that may be found in pleural fluid 1412) Describe adenocarcinoma cells 1413) Describe small cell or oat cell carcinoma cells 1414) Describe mesothelioma cells 1415) In inflammations and infections, glucose levels in pleural fluid are: 1416) pH of pleural fluid < 7.0 indicates the need for: 1417) pH of pleural fluid < 6.0 indicates: 1418) Pleural fluid adenosine deaminase is elevated in what two conditions? 1419) Pleural fluid amylase is elevated in what two conditions? 1420) Microbiology tests for pleural fluid involve: 1421) Serology tests on pleural fluid are done for: 1422) Tumor markers in pleural fluid for metastatic malignancy are: 1423) Carcinoembryonic antigen tumor marker for metastatic malignancy is specific for what type of malignancy? 1424) CA125 tumor marker for metastatic malignancy is specific for what type of malignancy 1425) What is the volume of pericardial fluid? Bacterial infection, pancreatitis, pulmonary infarction TB, viral infections, autoimmune disorders, malignancy Trauma introducing air and blood, allergic reactions, parasites Reactive mesothelial cells Mesothelial cells Tuberculosis (TB), because exudate covers membranes Adenocarcinoma cells, small or oat cell carcinoma cells, mesothelioma cells Large and irregular Small like lymph cells Large decreased Chest tubes Esophageal rupture (gastric fluid) TB and malignancy Esophageal rupture and malignancy Gram stains, aerobic and anaerobic cultures of fluid, TB smears and cultures Autoimmune disorders Carcinoembryonic antigen and CA125 GI malignancy Uterine and ovarian malignancy 10-50mL (normally small amount) 83 UA PPT Flashcards 1426) Permeability of membranes from infection (pericarditis, endocarditis), malignancy, trauma produces what type of pericardial fluid? 1427) Hypothyroidism, uremia and immune disorders produce what type of pericardial fluid? 1428) Pericardial fluid is detected by 1429) What is the appearance of normal pericardial fluid? 1430) Turbid pericardial fluid indicates: 1431) Bloody pericardial fluid indicates: 1432) Milky pericardial fluid indicates: 1433) Pericaridal fluid transudate vs exudate is differentiated using 1434) WBCs > 1000uL in pericardial fluid indicates: 1435) Malignant cells found in pericardial fluid are due to: 1436) Pericardial fluid Gram stains and cultures for endocarditis are often done when endocarditis is caused by: 1437) Pericardial fluid TB smears and cultures are done on persons with: 1438) In patients who have had asbestos exposure, what is the primary malignant cell seen in the pleural fluid? 1439) Effusion between peritoneal membranes is called? 1440) Fluid collected from the peritoneal membranes is called by what name? 1441) Transudates in peritoneal fluid are of what origin/disease? 1442) What are the 3 causes of exudates in peritoneal fluid? 1443) Why is a peritoneal lavage performed? 1444) True or False: Blunt trauma injuries can be a reason to perform a peritoneal lavage. 1445) Complete the following statement in regards to a peritoneal lavage. Normal saline injected into cavity, withdrawn, and a _____ ______ is performed. 1446) A RBC count greater than _____ indicates blunt trauma? 1447) In lieu of a peritoneal lavage, what Exudates Transudates Cardiac tamponade (compression) heard by a physician Clear, pale yellow Infection, malignancy (also blood streaked) Accidental puncture, anticoagulants Chylous and pseudochylous material Fluid-serum protein and LD ratios Bacterial endocarditis Lung or breast metastasis previous respiratory infections AIDS Metastatic giant mesothelioma cell Ascites Ascitic fluid Hepatic origin (cirrhosis) Bacterial peritonitis from intestinal perforation, ruptured appendix, and malignancy To detect early abdominal bleeding and need for surgery True RBC count >100,000 Radiographic procedures 84 UA PPT Flashcards other procedure is available to physicians to assess blunt trauma and abdominal bleeding? 1448) Are transudates and exudates easier or more difficult to determine in peritoneal fluid versus pleural or pericardial fluid? 1449) What method is the best way to determine transudate versus exudate? 1450) How do you determine the serumascites gradient? 1451) Determine if the fluid is a transudate or exudate. Serum albumin is 3.8 and the fluid albumin is 1.2 1452) What is the normal appearance of peritoneal fluid? 1453) If a peritoneal fluid is turbid, what might this suggest? 1454) If peritoneal fluid has a green-brown color, what is most likely present in the fluid? 1455) A milky appearance in peritoneal fluid is indicative of what? 1456) What is the normal WBC count in a peritoneal fluid? 1457) In a peritoneal fluid, what does an absolute neutrophil count of >50% of the total WBC count indicate? 1458) Lymphocyte counts in peritoneal fluid is elevated in what disease? 1459) Glucose levels below that of plasma levels in peritoneal fluid is a sign of what 2 things? 1460) In what 2 diseases is peritoneal amylase elevated? 1461) Increased peritoneal alkaline phosphatase is indicative of what problem? 1462) What 2 laboratory values from a peritoneal fluid will be elevated in both a ruptured bladder and accidental perforation? 1463) What are the 3 routine microbiology tests done on peritoneal samples? 1464) True or False: If an anaerobic culture More difficult Serum-ascites gradient Measure both the serum and fluid albumin levels, then subtract the fluid level from albumin level. If the difference (gradient) is >1.1 than you have a transudate (hepatic origin) 3.8-1.2 = 2.6 (>1.1 = hepatic transudate) Clear and pale yellow Bacterial or fungal infection Bile Chylous and pseudochylous with trauma and lymphatic blockage 350 cells/uL Infection TB Peritonitis and malignancy Pancreatitis and gastrointestinal perforation Intestinal perforation BUN and creatinine Gram stain, aerobic and anaerobic cultures True 85 UA PPT Flashcards is ordered on peritoneal fluid, the anaerobic blood culture bottle should be inoculated at the bedside. 1465) If TB is suspected, what 3 additional microbiology tests should be performed on peritoneal fluid? 1466) What 2 tumor markers are tested when a GI tumor is suspected? 1467) If a patient presents with a positive CA125 tumor antigen but a negative CEA, what is the likely source causing the positive CA125 antigen? 1468) A positive CEA antigen test suggests the tumor source is from what location? 1469) What is the amnion? 1470) Name the 5 functions of amniotic fluid 1471) During the first trimester, approximately how much of the amniotic fluid is derived from maternal circulation? 1472) The peak in amniotic fluid seen in the third trimester is the result of what fluid? 1473) How does the fetus compensate for the increased urine buildup during the third trimester? 1474) What is tested by physicians to determine fetal lung maturity? 1475) Name the 3 components that make up the volume of amniotic fluid. 1476) Define polyhydramnios 1477) What volume is considered to be polyhydramnios? 1478) Name 4 diseases/disorders that can cause polyhydramnios 1479) Define oligohydramnios 1480) What volume of amniotic fluid causes oligohydramnios 1481) Name the cause for oligohydramnios 1482) The chemical composition of amniotic fluid is similar to what other fluid? 1483) Sloughed fetal cells in the amniotic fluid may be used for what type of fetal testing? Acid-fast smear, adenosine deaminase, and a culture for TB CEA and CA125 A tumor on the ovaries, fallopian tubes, or endometrium Gastrointestinal A membranous sac that surrounds the fetus Provides protective cushion for fetus, allows fetal movement, stabilizes fetal temperature exposure, permits proper lung development, exchanges water and chemicals among the fluid, fetus and maternal circulation 35mL Fetal urine The fetus increases swallowing Lung surfactants in the amniotic fluid Fetal urine, lung fluid, and maternal circulation Excess amniotic fluid from failure of the fetus to swallow >1200mL Neural tube disorders, structural/chromosomal abnormalities, cardiac arrhythmias, and infections Decreased amniotic fluid from increased fetal swallowing <800mL Umbilical cord compression Maternal fluid Cytogenetic analysis 86 UA PPT Flashcards 1484) What 9 biochemical substances produced by the fetus are present in amniotic fluid? 1485) Fetal urine causes an increase in what biochemical substances? 1486) What biochemical substance can be used to estimate fetal age? 1487) Creatinine levels of >2.0mg/dL indicates the fetus has reached what gestational age? 1488) A gestational age of <36 weeks is indicated when the creatinine levels are between what range? 1489) Why would a physician need to know if a fluid was maternal urine or amniotic fluid? 1490) Name the chemical tests to differentiate maternal urine from amniotic fluid 1491) What creatinine and urea values indicate a fluid is amniotic fluid? 1492) A physician performs an amniocentesis and sends the specimen to the lab for stat urea and creatinine testing. The results are creatinine 8mg/dL and urea 250mg/dL. Is the fluid amniotic fluid? What might the physician suspect happened? 1493) True/False: The presence of glucose and protein, or both in fluid from an amniocentesis is more closely associated with amniotic fluid vs. maternal urine 1494) In what test is a glass slide examined microscopically for “fern-like” amniotic crystals? 1495) What abnormal blood tests might cause a physician to suggest an amniocentesis? 1496) If a pregnant woman presents to her physician and has a history of genetic disorders and/or abnormal chromosome analysis, would her physician recommend an amniocentesis? 1497) A pregnant woman undergoes a routine ultrasound and the physician notes abnormal fetal body Bilirubin, lipids, enzymes, electrolytes, urea, creatinine, uric acid, proteins, and hormones Creatinine, urea, and uric acid Creatinine >36 weeks 1.5-2.0mg/dL To determine premature membrane rupture or accidental puncture of maternal bladder from amniocentesis. Creatinine, glucose, protein, and urea <3.5mg/dL creatinine and <30mg/dL urea The fluid is most likely maternal urine, not amniotic fluid. The physician may have accidentally punctured the maternal bladder. True Fern test Maternal alpha fetal proteins, human chorionic gonadotropin, and unconjugated estriol Yes Amniocentesis 87 UA PPT Flashcards measurements. What may the physician suggest? 1498) Can a physician perform an amniocentesis later in the pregnancy? If yes, why? 1499) The collection of what substances in amniotic fluid indicates the genetic material of the fetus? 1500) Name the 4 methods in which fetal cells are tested for chromosomal abnormalities. 1501) What method is utilized to analyze biochemical substances produced by the fetus? 1502) What is the maximum amount of amniotic fluid that may be collected during an amniocentesis? 1503) What should a physician do to prevent contamination in the analysis of the amniotic fluid? 1504) Should amniotic fluid specimens be protected from light? 1505) Is an amniotic fluid specimen considered a routine or stat specimen? 1506) If fetal lung maturity testing is requested, what special handling requirement is necessary? 1507) What temperature prolongs the viability of cytogenetic specimens? 1508) State the normal color of amniotic fluid 1509) If an amniotic fluid sample is bloody, what may be the cause? 1510) What blood test would a physician order to determine fetal versus maternal cells? 1511) What substance may be present in amniotic fluid if it is a bright yellow color? 1512) A dark green amniotic fluid indicates the presence of what substance? 1513) Fetal death may be indicated by what colored amniotic fluid? 1514) How is Liley graph used to test for Fetal Distress? 1515) What does Liley graph consist of? 1516) Name 3 zones and theirs indication on Yes, because a doctor may need to determine fetal lung maturity for a possible early delivery due to HDN or infection Fetal epithelial cells Karyotyping, FISH, fluorescent mapping spectral karyotyping, and DNA testing Thin-layer chromatography 30mL Discard the first 2-3mL collected Yes. Protect from light for bilirubin analysis for HDN Stat Deliver test to lab on ice Room temperature Colorless Traumatic tap, abdominal trauma, intra-abdominal hemorrhage Kleihauer-Betke Bilirubin Meconium Dark red-brown Plots ∆ A450 against gestational age 3 zones based on hemolytic severity _ Zone I: mildly affected fetus 88 UA PPT Flashcards Liley graph? _ Zone II: requires careful monitoring _ Zone III: severely affected fetus, may require induction of labor or intrauterine exchange transfusion 1517) Alpha-fetoprotein (AFP) used to indicate neural tube defects in Fetal Distress. What is it produced by? 1518) What does an increase in maternal blood or amniotic fluid indicate? 1519) When an increased levels are found? By fetal liver, prior to 18 weeks of gestation 1520) What is the procedure in measuring neural tube defect? 1521) What is normal value based on? Measure maternal blood first, then amniotic fluid 1522) What is multiples of the median (MoM)? A laboratory’s reference level for a given week of gestation 1523) What is abnormal MoM? 1524) Does MoM need to be reported? 1525) What isacetylcholinesterase (AChE)? More than two times the median (MOM) Yes It’s a amniotic fluid that are more specific for neural disorders Do not perform on a bloody specimen 1526) What is the special requirement when performing AChE? 1527) What is the most common complication of early delivery that can be used to test for Fetal Lung Maturity (FLM)? 1528) Respiratory distress syndrome (RDS) happens due to what? 1529) What is lung surfactant? 1530) How does lung surfactant work? 1531) Test availability for FLM? 1532) What is the important of LecithinSphingomyelin (L/S) Ratio? 1533) What is Lecithin? 1534) When does increased production occur? 1535) What is the function of Sphingomyelin? 1536) When is Sphingomyelin produced? 1537) What is the reference range and Possible anencephaly or spinal bifida When skin fails to close over neural tissue Based on weeks of gestation (maximum AFP 12 to 15 weeks) Respiratory distress syndrome (RDS) Lack of lung surfactant A substance what keeps the alveoli open during inhaling and exhaling Decreases the surface tension on the alveoli so they can inflate more easily Manny Considered the reference method Primary component of the lung surfactants After the 35th week Serves as a control for the rise in lecithin Produced at a constant rate after the 26th week L/S ratio is 1.6 prior to week 35 and rises to 2.0 or 89 UA PPT Flashcards interpretation for it? greater for alveolar stability after week 35 Preterm delivery is considered safe with an L/S ratio of 2.0 or higher 1538) What is the test method for L/S ratio? 1539) What tests can be used to replace L/S ratio ? Thin-layer chromatography Quantitative Phosphatidyl Glycerol Immunoassays and Lamellar Body Density procedures 1540) What is the other test needed for lung maturity? 1541) How to read Phosphatidyl Glycerol? Lung surface lipid phosphatidyl glycerol 1542) What is Amniostat-FLM? An immunologic agglutination test for PG using antibody specific for phosphatidyl glycerol that can replace the L/S ratio Blood and meconium do not interfere with the test 1543) What is the positive aspect for Phosphatidyl Glycerol test? 1544) Where can Foam Stability be performed? 1545) What is the procedure for Foam Stability? Normally parallels lecithin, except in diabetics, so must be included in L/S ratio At the bedside Amniotic fluid is mixed with 95% ethanol, shaken for 15 seconds, and allowed to sit undisturbed for 15 minutes 1546) How to read Foam Stability? A continuous line of bubbles around the outside edge indicates the presence of a sufficient amount of surfactant to maintain alveolar stability (alcohol is an antifoaming agent, and fluid can overcome this) 1547) What need to be added to increasing amounts of 95% ethanol? 1548) What a value >47 indicates? 1549) What is the special note for Foam Stability test? 0.5 mL amniotic fluid 1550) What is Lamellar bodies? Storage form of surfactant (Approximately 90% phospholipid and 10% protein) 1551) What is Lamellar bodies secreted by? Type II pneumocytes of the fetal lung to the aveolar space at about 24 weeks of gestation 1552) What is the reference range for Lamellar bodies? Increase in amniotic concentration from 50,000 to 200,000/mL by the end of the third trimester 1553) 1554) What is the Lamellar body diameter From 1.7 to 7.3 fL or 1 to 5 µm FLM Correlates well with L/S ratio and tests for phosphatidyl glycerol 90 UA PPT Flashcards ranges in size? 1555) How can LBCs be obtained? 1556) What are the Advantages of LBC? 1557) What is the restriction of LBC? 1558) What is the protocol for Performing LBC? 1559) What are feces? 1560) What are the 3 fecal analysis? 1561) What disease fecal analysis can be used to detect? 1562) What does Fecal specimen contains? Using the platelet channel of automated hematology analyzer – Rapid turnaround time – Low reagent cost – Wide availability – Low degree of technical difficulty – Low volume of amniotic fluid required – Excellent clinical performance Specimens contaminated with meconium or mucous cannot be used a. 1. Mix the amniotic fluid sample by inverting the capped sample container five times. 2. Transfer the fluid to a clear test tube to allow for visual inspection. 3. Visually inspect the specimen. Fluids containing obvious mucus, whole blood, or meconium should not be processed for an LBC. 4. Cap the tube and mix the sample by gentle inversion or by placing the test tube on a tube rocker for 2 minutes. 5. Flush the platelet channel; analyze the instrument’s diluents buffer until a background count deemed acceptable by the laboratory is obtained in two consecutive analyses. 6. Process the specimen through the cell counter and record the platelet channel as the LBC. The end product of digestion – Macroscopic – Microscopic – Chemical • • • • • • • Gastrointestinal (GI) bleeding Liver and biliary duct disorders Maldigestion/malabsorption syndromes Pancreatic diseases Inflammation Diarrhea and steatorrhea Detection and identification of pathogenic bacteria, viruses, and parasites Bacteria, cellulose, undigested foodstuffs, GI secretions, bile pigments, cells from the intestinal walls, electrolytes, and water 91 UA PPT Flashcards 1563) How many gram of feces are excreted in a 24h period? 1564) What is the primary site for the final breakdown and reabsorption of proteins, carbohydrates, and fats? 1565) What can aid small intestine in the break down and reabsorption of proteins, carbohydrates, and fats? 1566) How many ml of ingested fluid, saliva, gastric, liver, pancreatic, and intestinal secretions enter the digestive tract each day 1567) Majority of fluids involved in digestion are? 1568) What is diarrhea? 1569) 1570) What are the 4 factors of diarrhea? 100 to 200 g of feces Small intestine Pancreatic enzymes and bile salts Approximately 9000 mL Reabsorbed, with only about 150 mL excreted in feces Excess water (>3000 mL) reaching large intestine, or 200 g stool weight per day with increased liquid and more than three movements per day – – – – Illness duration Mechanism Severity Stool characteristics 1571) What is chronic Diarrhea? 1572) What is acute Diarrhea? 1573) What are the 3 Mechanisms of diarrhea? 1574) What are Laboratory tests for diarrhea? 1575) What does Ph <5.6 indicates? 1576) What can be used to calculate fecal osmotic gap? >4 week duration <4 week duration Secretory, osmotic, altered motility 1577) Total fecal osmolarity Close to serum osmolarity (290 mOsm/kg) 1578) What is Osmotic gap? 290 [2 × (fecal Na + fecal K)] 1579) What is Osmotic diarrhea? >50 mOsm/kg 1580) What is Secretory diarrhea? <50 mOsm/kg 1581) What happens when an increased in secretory and negligible in osmotic diarrhea 1582) An increase secretion of water and electrolytes indicate what? Electrolytes loss Fecal electrolytes, osmolarity, and pH sugar malabsorption Sodium, potassium, osmolarity Bacterial, viral, and protozoan infections 92 UA PPT Flashcards 1583) What are these bacteria? Escherichia coli, Clostridium, Vibrio cholerae, Salmonella, Shigella, Staphylococcus, Campylobactor, Cryptosporidium 1584) What can affect the Secretory Diarrhea? Drugs, laxatives, inflammatory bowel disease/colitis, endocrine disorders, malignancy, collagen vascular disease 1585) What can exert osmotic pressure across the intestinal mucosa in osmotic diarrhea? 1586) What happens when there is incomplete digestion or reabsorption of food? 1587) What is Maldigestion? Poor absorption 1588) What is Malnutrition? 1589) What are the issues involving Osmotic Diarrhea? Impaired reabsorption Lactose intolerance, celiac sprue (malabsorption), amebiasis, antibiotics, laxatives, antacids 1590) What can cause Irritable bowel syndrome (IBS)? 1591) What is the motility rate that can indicate Rapid Gastric Emptying (RGE) (or Dumping Syndrome) 1592) The types of dumping syndrome can be based on what? 1593) What are the 2 types of Dumping Syndrome? 1594) What are the diseases that involve with altered motility? Hypermotility and constipation; food, chemicals, stress, and exercise <35 minutes 1595) What is Steatorrhea? Increased fats in the stool >6 g/day 1596) What can cause Steatorrhea? Pancreatic insufficiency and malabsorption and lack of bile salts (triglyceride digestion) 1597) What disease decrease pancreatic enzymes for lipid breakdown? 1598) What does D-xylose test for? 1599) Low level of D-xylose in urine indicates what? 1600) What is the special note regarding Dxylose test? Cystic fibrosis, pancreatitis, and malignancy increases water retention in large intestine Impaired digestion of foods Timing of symptoms Early: 10 to 30 minutes Late: 2 to 3 hours Gastrectomy, gastric bypass, postvagotomy, duodenal ulcer, diabetes mellitus Malabsorption Malabsorption D-xylose does not need to be digested but must be reabsorbed to appear in the urine 1601) What are the procedures for specimen _ Use clean container and transfer to laboratory 93 UA PPT Flashcards collection? container _No toilet water contamination _ Acceptable for some occult blood test kits 1602) Can we use Ova and parasite containers for different purpose? No, Ova and parasite containers are used only for that purpose. 1603) What is the time requirement for Quantitative collections? 1604) What is Quantitative collections? 72 hours 1605) What is the macroscopic screening for stool? – Color – Appearance: formation (GI disturbances can often be changes in the brown color and formed consistency of the normal stool ) 1606) Brown color of feces indicate what? Urobilin 1607) Pale, acholic stools indicate what? Bile duct blockage, barium sulfate 1608) How does blood appear in feces? Bright red to dark red to black, depending on area of digestive tract that is bleeding Upper tract bleeding, medications, iron, bismuth, charcoal 1609) Black color of feces indicate what? Time required to pass through intestine 1610) Red color of feces indicate what? 1611) Green color of feces indicate what? Lower tract bleeding, beets Antibiotics, bilirubin to biliverdin 1612) A watery feces appearance indicate what? 1613) A hard feces appearance indicate what? 1614) A ribbon-like feces appearance indicate what? 1615) What are the characteristics of Steatorrhea? 1616) What does mucus coated feces indicate? 1617) What does blood-streaked mucus indicate? 1618) What should we do when we see mucus in stool? 1619) What does fecal microscopic exam for? 1620) What do neutrophil present in? Diarrhea 1621) What do Salmonella, Shigella, Constipation Obstruction Pale, bulky, frothy, foul odor Intestinal irritation, inflammation, colitis, straining Intestinal wall damage, dysentery, malignancy Always report mucus Fecal leukocytes, primarily neutrophils. In bacterial dysentery, Dysentery from bacterial toxins, food poisoning. Bacterial dysentery because they invade the intestinal 94 UA PPT Flashcards Campylobacter, Yersinia, and E. coli O157 cause? 1622) What is the microscopical characteristic of Staphylococcus and Vibrio in stool? 1623) What is food poisioning? 1624) For microscopic examination of fecal matter, a smear is made with ____ or ____ stain. 1625) Under hp, how many neutrophils per field is signigicant? 1626) Under oil immersion, any neutrophils have a _____ % significance. 1627) Lactoferrin latex agglutination is good for _____ specimens, refrigerated or frozen. 1628) Lactoferrin is in the granules of what? 1629) In the methylene blue staining procedure for fecal leukocytes, the lab tech places mucus or a drop of liquid stool on the slide and adds ____ drops of Loffler methylene blue, mixes with a wooden stick and allows to stand for ____ minutes before examination. 1630) When testing fecal matter for muscle fibers, the patient must eat what before collection? 1631) What disorders can cause undigested striated mucsle fibers? 1632) Muscle fibers in feces can be seen on a slide prepared with what? 1633) When examining a slide for muscle fibers, the technician will count the numbers of fibers that exhibit what? 1634) Undigested fibers exhibit _________ 1635) Partially digested fibers exhibit_______ 1636) Digested fibers exhibit______ 1637) When counting muscle fibers, only the ____ are counted and more than ____ per slide is abnormal. 1638) When performing screening for steatorrhea, which lipids are included? 1639) What stain is used for steatorrhea screening? 1640) In the two-part test, neutral fat will appear as ______ and ____ per hpf is wall Do not have leukocytes Staphylococcus versus invasive dysentery Wright or Gram Three 70% older Neutrophils Two drops; 2-3 minutes Red meat Pancreatic insufficienncy and cystic fibrosis 10% alcoholic eosin Well preserved striations vertical and horizontal striations striations in only one direction no striations undigested; 10 neutral fats (triglycerides), fatty acid salts (soaps), free fatty acids, and cholesterol Sudan III or IV, oil red 0 large red-orange droplets; 60; split fat 95 UA PPT Flashcards indicative of steatorrhea and _____ is more indicative. 1641) In the neutral fat stain procedure,one part stool is homogenized with how many parts water? 1642) In the neutral fat stain procedure what stain is used and what is counted? 1643) In the split fat stain, _____ form after heating and cooling and have characteristic _____. 1644) In the split fat staining procedure, the emulified stool is mixed with _____ and stained with two drops of ______ before being heated. 1645) The test principle of fecal occult blood testing is? 1646) The guaiac test will turn what color in the presence of bood? 1647) Guaiac is less sensitive than urinalysis reagent because why? 1648) Commercial kits for fecal occult blood testing have strict dietary rules including ____ for three days prior. 1649) When performing the guaiac test in the lab, the outside areas of the stool might cause a false positive. Why? 1650) Aspirin, anti-inflammatory meds, red meat, horseradish, raw broddoli, and melons may lead to a _____ occult blood test. 1651) High levels of vitamin C may cause a _____ occult blood test 1652) Immunochemical Fecal Occult Blood Test (iFOBT) is more sensitive because it tests for specific _____, there is no need for ____, and is more sensitive to _____. 1653) Hemoquant tests for ____ from hemoglobin degradation that is not detected by guaic 1654) Quantitative fecal fat testing to confirm steatorrhea includes ____ collection in a preweighed container that requires ____ to slow down bacterial action. 1655) Reporting of fecal fat is done as grams of fat or the coefficient of fat retention based on 100 g/d intake of fat Two Sudan III; count orange droplets per high-power field cholesterol crystals; flat shape and notched corners 36% acetic acid; Sudan III pseudoperoxidase activity of hemoglobin Blue Up to 2.5 ml of blood in stool is normal No red meat Hemorrhoids might affect these areas of the stool False positive False negative human hemoglobin, dietary restrictions, lower GI bleeding porphyrin 3-day; refrigeration Doefficient of fat retention= dietary fat - fecal fat/dietary fat (100) 96 UA PPT Flashcards represented by which calculation? 1656) Normal values of quantitative fecal fat are? 1657) A rapid (5 minutes) for analyzing quantitative fecat fat is what? 1658) What test for quantitative fecal fat provides rapid estimate, requires a single 5g specimen that is homogenized and acidified and spun in a regular hematocrit tube? 1659) How does a technician measure the steatocrit after spinning? 1660) What is the normal adult steatocrit value? 1661) Near-infrared reflectance spectrophotometry scans surface of stool with light between what wavelengths? 1662) The APT test for fetal hemoglobin checks for what? 1663) Afte emulsifying material in water to release hemoglobin in the APT test, the technician centrifuges and adds 1% NaOH to pink supernatant. If pink color remains, then that equals_____. If it changes to a yellow-brown then that equals ______. 1664) Maternal thalassemia major has what? 1665) In th APT test procedure, the controls use what specimens? 1666) Measuring pancreatic fecal enzymes can help diagnose what disorders? 1667) What test for enzymes is not very sensitive and involves stool dissolving gelatin on x-ray paper? 1668) ____ is more sensitive than the classic trypsin test, less degraded, and spectrophotometric measuring is available. 1669) _____ is an isoenzyme of elastase produced by the pancreas, is present in high concentrations and resistant to degradation, is not affected by gastric motility, and differentiates pancreatic form nonpancreatic causes of steatorrhea. 1 to 6 g/d or coefficient of fat retention of at least 95% Hydrogen nuclear magnetic resonance spectrocopy (1H NMR) Acid steatocrit Fatty layer/fatty layer + solid layer (100) less than 31% 1400 and 2600 nM Bloody stools and vomit from neonates who may have swallowed maternal blood during delivery Pink color= alkali-resistant fetal Hgb yellow-brown = maternal Hgb Increased Hgb cord blood and adult blood pancreatic insufficiency and cystic fibrosis Trypsin test Chymotrypsin Elastase-1 97 UA PPT Flashcards 1670) Why does increased stool carbohydrates cause osmotic diarrhea? 1671) Common causes of increased stool carbohydrates include? 1672) To test for maldigestion, what test can be performed? 1673) To test for malabsorption, what test can be performed? 1674) Common fecal testing on infants include pH to detect what? 1675) Normal stool pH is 7 to 8, pH below 5.5 indicates what? 1676) The Clinitest can help distinguish between carbohydrated-caused diarrhea and ____ diarrhea. 1677) A positive Clinitest should be followed by a ______ 1678) What is the most common conditions in female patients? 1679) Swab in a tube containing ____ to ____ of sterile physiologic saline and agitated. 1680) What is the appearance of vaginitis? 1681) What is the pH of women with vulvovaginal candidiasis? 1682) Where is squamous epithelial cells located on human body? 1683) Alteration in the normal flora can cause overgrowth of ___________ 1684) What are the characteristics of trichomonas vaginalis? 1685) Differentiation of yeast cells can be made using the ___ test 1686) KOH test uses ___ of KOH solution 1687) Gold standard in identifying the causative organisms of BV is? 1688) Trichomonas is incubated for ___ days at __C in a CO2 atmoshere 1689) What is used to identify the causative pathogen for vaginitis? 1690) Which activity is observed for vaginal secreations for G. vaginalis? 1691) The most common cause of vaginitis, affecting ___% to __% of women of child bearing age. Excess water is needed to remove the carbohydrates The inability to reabsorb or lack of digestive enzymes Lactose tolerance test D-oxylose tolerance test Fermentation of excess carbohydrates by intestinal bacteria Increased carbohydrates viral-caused Tolerance test vaginitis 0.5 to 1.0 ml Predominance of large, rod shaped, gram-positive lactobacilli 4.5 Linings of vagina and female urethra Opportunistic flora Atrial flagellated protozoan, oval shaped, four anterior flagella and undulating membrane that extends half of the the length of the body. KOH 10% Gram stain 5 days, 37 C DNA testing using DNA hybridization probe Proline aminopeptidase activity 40-50% 98 UA PPT Flashcards 1692) what is the recommended treatment for trichomoniasis? 1693) What are some Candida Nonalbican species? 1694) What are some changes in the vaginal environment that permits the overgrowth of Candida? tinidazole 1695) What are some Clinical symptoms of Candidiasis? Genital itching or burning, Dyspareunia, Dysuria and Abnormal thick, white, and curd-like vaginal discharge 1696) What does Candidiasis look like/Characteristics of Candidiasis on Saline and KOH wet prep and Gram stain. 1697) How can species of Candida be confirmed and identified 1698) Candidiasis can be treated with which over the counter medications? 1699) What are some prescribed medications for Candidiasis? 1700) What is an abbreviation for Desquamative Inflammatory Vaginitis? 1701) What is Desquamative Inflammatory Vaginitis? budding yeast and pseudohyphae forms, large numbers of WBCs, lactobacilli, and large clumps of epithelial cells 1702) What is the lab result for Desquamative Inflammatory Vaginitis? Testing reveals large numbers of WBCs, RBCs, occasional parabasal and basal cells, squamous epithelial cells, and reduced or absent lactobacilli 1703) How is Desquamative Inflammatory Vaginitis treated? 1704) What is Atrophic Vaginitis? With 2% clindamycin, Hormone replacement therapy 1705) Atrophic Vaginitis microscopic evaluation is similar with what other illness? 1706) What is the treatment of atrophic vaginitis. 1707) What is the leading cause of neonatal Desquamative Inflammatory Vaginitis? (DIV) C. glabrata, C. parapsilosis, C. Tropicalis, and C. krusei Broad-spectrum antibiotics, oral contraceptives, or estrogen replacement therapy; hormonal changes that occur with pregnancy; ovulation; and menopause. Immunocompromised patients and those with conditions such as diabetes mellitus, iron deficiency, and HIV infection Through culture and DNA hybridization probe Butoconazole, clotrimazole, tioconazole, and miconazole Oral fluconazole orintravaginal butoconazole, Nystatin, and terconazole. DIV Profuse purulent vaginal discharge, vaginal erythema, and dyspareunia Found in postmenopausal women, thinning of thevaginal mucosa due to decreased estrogen and glycogen; Vaginal dryness and soreness, dyspareunia, inflamed vaginal mucosa, and purulent discharge. Estrogen replacement Preterm delivery- delivery before the completion of 37 99 UA PPT Flashcards mortality and morbidity in the United States? 1708) What are some complications from vaginitis syndromes. weeks gestation. Premature rupture of fetal membranes and a high risk of preterm labor. 100