File - Medical Nutrition Therapy Portfolio
advertisement
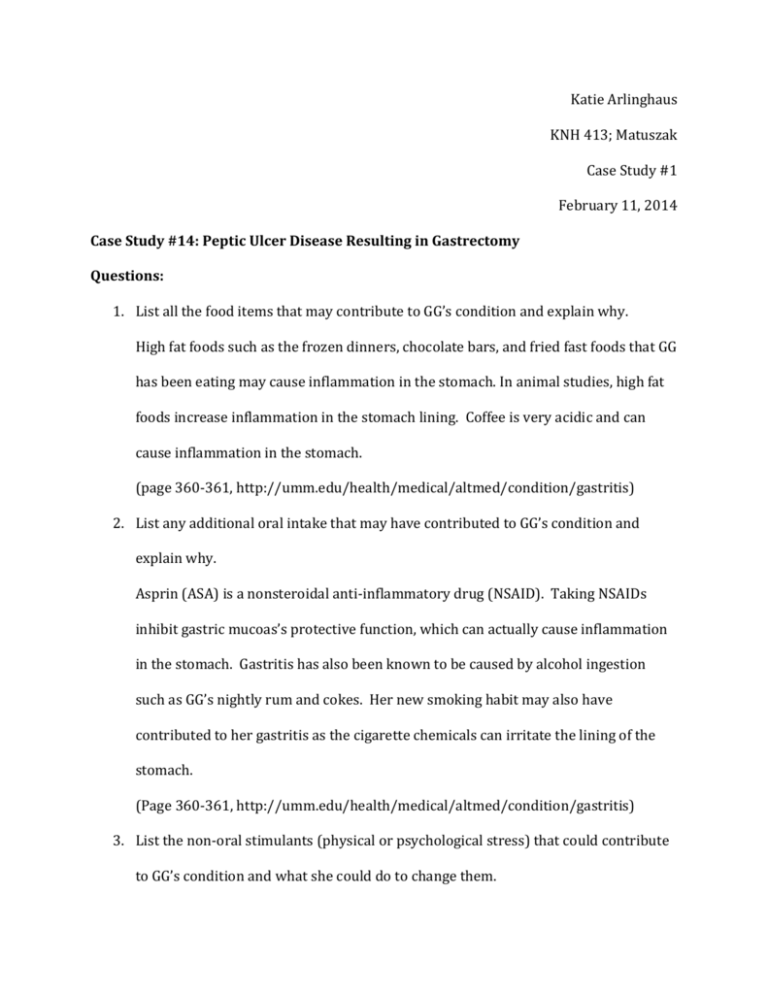
Katie Arlinghaus KNH 413; Matuszak Case Study #1 February 11, 2014 Case Study #14: Peptic Ulcer Disease Resulting in Gastrectomy Questions: 1. List all the food items that may contribute to GG’s condition and explain why. High fat foods such as the frozen dinners, chocolate bars, and fried fast foods that GG has been eating may cause inflammation in the stomach. In animal studies, high fat foods increase inflammation in the stomach lining. Coffee is very acidic and can cause inflammation in the stomach. (page 360-361, http://umm.edu/health/medical/altmed/condition/gastritis) 2. List any additional oral intake that may have contributed to GG’s condition and explain why. Asprin (ASA) is a nonsteroidal anti-inflammatory drug (NSAID). Taking NSAIDs inhibit gastric mucoas’s protective function, which can actually cause inflammation in the stomach. Gastritis has also been known to be caused by alcohol ingestion such as GG’s nightly rum and cokes. Her new smoking habit may also have contributed to her gastritis as the cigarette chemicals can irritate the lining of the stomach. (Page 360-361, http://umm.edu/health/medical/altmed/condition/gastritis) 3. List the non-oral stimulants (physical or psychological stress) that could contribute to GG’s condition and what she could do to change them. GG’s life is extremely stressful right now. Her husband left, her son was diagnosed with ADHD, she returned to school, she is working part time, and has had to take out loans. In fact, her stress caused her to begin many of the unhealthy intake habits described above. Furthermore her psychological stress is preventing her from being able to sleep, which only adds physical stress. GG needs to try to reduce the stress in her life. She was right that she needed a break. However, getting drunk is not a break and will not fix her stress. Instead, she needs to find a way to reduce her stress. Maybe she can reduce her class load or hours at work. It might also be beneficial for her to talk to a physiatrist or some type of counselor to learn healthy strategies to mitigate her stress. She can and should follow the doctor’s advice to stop smoking, drinking, and taking aspirin but since these habits began as her way to manage her stress, she will need to find a new healthier way to manage and decrease it. (http://digestive.niddk.nih.gov/ddiseases/pubs/gastritis/) 4. List the symptoms of GG’s gastritis. GG’s gastritis symptoms include severe upper abdominal pain, increased pain in her RLQ, and a burning stomach. (http://digestive.niddk.nih.gov/ddiseases/pubs/gastritis/) 5. Was a bland diet necessary? Explain and list the principles of the diet plan that you think GG should follow. A bland diet is not necessary; although, it was previously thought to be the proper treatment for gastritis. GG should avoid alcohol, cigarettes, and NSAIDs. For some people, gastritis will subside on its own after discontinuing use of these. Diet wise, GG should avoid beverages such as cola, coffee, tea cocoa, and fruit juices with citric acid. She should also avoid high fat foods and cooking methods; this includes high fat dairy, protein, and pastry products as well as fried foods. GG should try to incorporate fiber rich foods into her diet. (http://umm.edu/health/medical/altmed/condition/gastritis, page 161) 6. What is the mechanism of action of the following medications GG is receiving: Carafate, AlternaGel, and Pepcid? Carafate is a brand name for the generic sucralfate, which is a cytoprotective agent. It protects the stomach mucosa against injury by acting as an acid buffer, forming protective barriers, and increasing gastric mucous secretion. AlternaGel is an aluminum hydroxide. This is used to neutralize HCl in the stomach, which will relieve some of the heartburn like symptoms of gastritis. Pepcid is a brand name for the generic famotidine. Famotidine is in a class of medications called H2 blockers. It works by decreasing the amount of acid made in the stomach. (http://www.nlm.nih.gov/medlineplus/druginfo/meds) 7. List the nutrient-drug interactions that are associated with these medications. Carafate has been shown to increase blood calcium levels and decrease phosphorus levels. AlternaGel has been shown to interfere with normal calcium metabolism. Aluminum can form compounds with phosphates, removing them from the body. It can also interfere with thiamine absorption, and should, therefore, not be taken at meal times. Pepcid has been shown in some studies to reduce the absorption of vitamin B12. (http://www.healthcentral.com/static/pp/pdf_guides/nutrient.pdf) 8. What are GG’s IBW and percent of IBW? GG’s IBW is 110lbs (she is 5’ 2”. 100lbs for the first 5’+ 5 lbs for each additional inch=100+(5*2)=110). Her percent IBW= (current weight/IBW)*100=98/110=89% 9. Estimate her daily energy needs using the Harris-Benedict equation and appropriate stress factor. Harris-Benedict: REE=655.1+9.6(weight kg)+1.9(height cm)-4.7(age years) (using IBW): REE=655.1+9.6(110lb/2.2kg)+1.9(62in*2.54cm)-4.7(27) REE=655.1+9.6(50kg)+1.9(157.48cm)-4.7(27years)=1,307.41kcal EER=1,307kcal*1.15 stress factor GG needs 1,503kcal a day. (Page 241) 10. What might be the cause of the LUQ pain along with her usual pain (consider the enzymes that are elevated)? Alkaline phosphatase (ALP) is a group of enzymes that are highly active in the liver, which is located in the left upper quadrant (LUQ) of the abdomen. GG has an elevated level of ALP. This could be the cause of her LUQ pain. Her high amylase level may also be a cause of her LUQ pain because high levels of amylase can often be traced to the pancreas, an intestinal obstruction, or kidney disease, all of which are in the LUQ. (http://www.beaconforhealth.org/PDF/BloodTests.pdf) 11. In the second set of lab values, glu, BUN, Cr, ser alb, Na, K, Cl, hgb, and hct all dropped. This probably means that GG was: a. bleeding. b. eating poorly in the hospital. c. dehydrated when the first labs were drawn. d. over hydrated when the second set of labs was drawn. (http://wvuhealthcare.com/wvuh/Healthcare-Services/Multiphasic-BloodAnalysis/Multiphasic-Blood-Analysis, http://www.beaconforhealth.org/PDF/BloodTests.pdf) 12. In the second set of lab values, serum amylase, AST, and ALT all dropped. This probably means that: a. enzymes were elevated due to alcohol. b. her medications caused them to drop. c. GG was dehydrated when the first labs were drawn. d. GG was over hydrated when the second set of labs was drawn. (http://wvuhealthcare.com/wvuh/Healthcare-Services/Multiphasic-BloodAnalysis/Multiphasic-Blood-Analysis, http://www.beaconforhealth.org/PDF/BloodTests.pdf) 13. Refer to the two lab tables again, and note that two days after admission, GG’s Alk Phos and CPK remained essentially unchanged. Why? a. these enzymes are not affected by alcohol or hydration b. her medications caused them to drop c. dehydrated when the first labs were drawn d. over hydrated when the second set of labs was drawn (http://wvuhealthcare.com/wvuh/Healthcare-Services/Multiphasic-BloodAnalysis/Multiphasic-Blood-Analysis, http://www.beaconforhealth.org/PDF/BloodTests.pdf) 14. What diagnostic test(s) (not lab values) indicate(s) that GG has an ulcer? The diagnostic tests they ran on GG that indicate that she has an ulcer include esophagogastroduodenoscopy, BUT positive for H. pylori, and the positive ELISA test for H. pylori. (http://www.nytimes.com/health/guides/disease/peptic-ulcer/diagnosis.html) 15. Briefly sketch the anatomical position where GG’s ulcer can be found. 16. Define: a. H2 antagonist: are sometimes also referred to as H2 blockers. This type of medication suppresses acid secretion to ultimately promote healing of the ulceration. b. Proton pump inhibitor: agents that block the transport of hydrogen ions into the stomach and hence are useful in the treatment of gastric hyperacidity. (http://www.medilexicon.com/medicaldictionary.php, Page 162) 17. What is the mechanism of action of the following medications GG is receiving: Nexium, amoxicillin, and clarithromycin? Nexium is a esomeprazole drug, which is in the protein pump inhibitor class of medications. It works by decreasing the amount of acid made in the stomach. Amoxicillin is in a class of medications called penicillin-like antibiotics. It works by stopping the growth of bacteria such as H. pylori. Clarithromycin is in a class of medications called macrolide antibiotics, which work by stopping the growth of bacteria such as H. pylori (http://www.rxlist.com/nexium-drug.htm, http://www.nlm.nih.gov/medlineplus/druginfo/meds 18. GG was not receiving counsel at the time the major bleeding started. If you had the opportunity to counsel GG just before the bleeding, in what areas would you feel competent to counsel her and in what areas would you refer her to someone else? Investigate the agencies in your area that are available to provide assistance to someone like GG. I would feel confident to counsel her with her dietary needs. I would have to refer her to a counselor to deal with the stress items in her life. I would refer her to the Oxford Community Counseling and Crisis Center first. This would be the first place GG could go (for free) and they would be able to provide her with additional resources and options. The Women’s Health Issue in Miami-Valley Sisterhood and the Butler County Community Action Agency offer free medical care programs, which may be useful if her medical needs persist. The legal aid society provides free legal information that she might find helpful as she navigates this with her husband. (http://www.needhelppayingbills.com/html/butler_county_assistance_progr.html) 19. What is the significance of the dark stools? Dark stools maybe indicative of Melena. The dark stools of melena are caused by bleeding in the upper GI. Hemoglobin in the blood is altered by digestive chemicals and intestinal bacteria turning it dark. The bleeding often comes from an ulcer. (http://www.nlm.nih.gov/medlineplus/ency/article/003130.htm) 20. Give the pathophysiology for the cause of the following abnormal values: BUN, NH3, and WBC. GG’s BUN level could be high due to dehydration from GG vomiting. High BUN levels also indicate that urea nitrogen levels are higher than normal, which suggests that the kidneys or the liver are not functioning properly. GG’s alcohol consumption would have easily irritated the functioning of her liver and kidney. Her elevated BUN level could also be due to absorption of degraded blood during intestinal transit and prerenal azotemia from hypovolemia. High levels of NH3 indicate that her liver is not functioning properly. Ammonia is formed in the body when protein is broken down. The liver converts the ammonia to urea, which is then taken out of the body by urine. Since GG’s ammonia level was high, it is clear that the liver is not doing this (probably because of her alcohol intake). WBC raises when one is under stress or when one has an infection. It makes sense therefore, that GG would have a high WBC as she is under severe stress and has an ulcer. http://www.nlm.nih.gov/medlineplus/ency/article/003643.htm 21. GG was probably dehydrated on admission since she had been drinking. This means that some of her lab values were probably higher/lower (circle one) than indicated. (http://wvuhealthcare.com/wvuh/Healthcare-Services/Multiphasic-BloodAnalysis/Multiphasic-Blood-Analysis, http://www.beaconforhealth.org/PDF/BloodTests.pdf) 22. After admission GG received packed cells and IV fluids. How would that affect the next set of lab values? All of her electrolytes would normalize because she would no longer be dehydrated. Her hemocrit, hemoglobin, RBC, etc would increase from the packed cells. (http://www.healthline.com/health/intravenous-rehydration#Intro) 23. Define the following terms: a. Packed Cells: a preparation of blood cells separated from the liquid plasma; "packed cells are given to severely anemic patients in order to avoid overloading the circulatory system with too much fluid" b. Abdominal tap: procedure used to remove fluid from the area between the belly wall and the spine. This space is called the abdominal cavity. c. Perforated ulcer: an ulcer extending through the wall of an organ. d. Fistula: An abnormal passage from one epithelial surface to another epithelial surface. e. Exploratory Laparotomy: Incision into the loin f. Billroth I: excision of the pylorus and antrum and partial closure of the gastric end with end-to-end anastomosis of stomach and duodenum. g. Vagotomy: Division of the vagus nerve. (http://www.medilexicon.com/medicaldictionary.php) 24. Sketch a Billroth I. 25. Compare a Billroth I to a Billroth II as to anatomical changes as well as to dietary changes, if any. A Billroth I operation is the excision of the pylorus and antrum and partial closure of the gastric end with end-to-end anastomosis of stomach and duodenum, whereas a Billroth II operation excision of the pylorus and antrum with closure of the cut ends of the duodenum and stomach, followed by a gastrojejunostomy. After a Billroth procedure digestion and absorption pathways are interrupted. Vitamin B12, iron, calcium, and vitamin D deficiencies are of particular concern. Dumping syndrome is also very concerning. Meals should be small and frequent and beverages shouldn’t be consumed with meals. (http://www.medilexicon.com/medicaldictionary.php, page 364-365) 26. Calculate GG’s energy and protein needs. After surgery GG’s energy and protein needs increase. She will need 30-40kcal/kg body weight and 1-1.8g/kg body weight of protein. Using her ideal body weight: 110lb/2.2kg = 50kg 30kcal*50kg=1,500kcal 40kcal*50kg=2,000kcal 1g*50kg=50g protein 1.8g*50kg=90g protein GG needs 1,500-2,000kcal and 50-90g protein a day. (tulane.edu/som/departments/surgery/.../Nutrition.ppt) 27. List the principles of a postgastrectomy diet and briefly describe the scientific basis for each principle. Postgrastrectomy diet or “anti-dumping diet” includes a slightly higher fat and protein content. Simple sugars, clear liquids, are avoided to prevent hyperosmolality and hypoglycemia associated with the dumping syndrome. Generally postgastrectomy patients are not able to tolerate lactose so dairy products are generally avoided on this diet. This makes it even more important for patients to take vitamin D and calcium supplements. Liquids should be consumed between meals so prevent dumping syndrome as liquids can cause quick movement through the small intestine. A slow progression of solid food is necessary to prevent dumping syndrome. If patients do not make progress towards solid foods nutrition support should be suggested. Furthermore, patients should slowly progress to eating five to six small meals a day. (Page 366-367) 28. Is it possible that GG’s diet will ever change or do you believe she will be on a postgastrectomy diet for the rest of her life? Explain your answer. She will have a modified diet for the rest of her life. The postgastrectomy diet should be her starting basis for her diet. However, patients generally stray as tolerated. It will be important for her to always eat small meals. This is all assuming that GG successfully transitions to solid foods and that she is able to successfully eat 5 to 6 meals a day. (http://www.medicine.virginia.edu/clinical/departments/medicine/divisions/dige stive-health/nutrition-support-team/nutrition-articles/radiganarticle.pdf) 29. If GG were to be hospitalized for an extended period of time and required a tube feeding via duodenum or jejunum, what characteristics would be appropriate for the tube feeding you would use? It would be appropriate to use a nasoduodenal placement, a nasojejunal placement, or a jejunostomy tube. Nasoduodenal and nasojeunal placements are good when there is normal small intestine function but have to bypass the stomach as primary site of feeding. The tube can be inserted bedside, but there is often discomfort for the patient and tube displacement. The jejunostomy option allows for the need to bypass components of the GI tract and is for longer-term feeding access. There is an increased tolerance for early initiation of enteral feeding. The disadvantage to the jejunostomy is that it requires a surgical procedure. There is risk of irritation and infection for the insertions site and a clogging risk. However, because GG is going to be hospitalized for an extended period of time the jejunostomy tube seems to be most appropriate for her. (Page84-86) 30. Using the table below, compare several of the enteral nutritional supplements that would be appropriate for GG. Product Producer Fibersource HN Nestle Isosource HN Nestle Promote Abbot Compleat Nestle Nutren 1.0 Nestle Form Tube Feeding Formula Complete Liquid feeding formula Tube or oral feeding Tube feeding formula Liquid tube feeding formula Cal/ mL g/L Na mg K mg mOsm /kg water Pro CHO Fat 1.2 53 160 39 300 20 490 Vol to meet RDA in ml 1165 1.2 53 160 39 280 470 490 1165 6 205 1.0 63 130 26 310 500 380 1000 13.6 197 1.07 48 128 40 250 385 340 1313 6 214 1.0 40 127 38 220 310 370 1500 14 212 (Page A-99, http://www.nestlehealthscience.us/products) g of fiber /L 10 Free H 2O /L in mL 203 Works Cited Aronson, Linda. "Blood Test Results - But What Does It Mean? ." Beacon Library. Beacon for Health, n.d. Web. 7 Feb. 2014. <http://www.beaconforhealth.org/PDF/BloodTests.pdf>. "Butler County Assistance Programs." Butler County. N.p., n.d. Web. 7 Feb. 2014. <http://www.needhelppayingbills.com/html/butler_county_assistance_progr.html >. "Drug and Nutrient Interactions." The People's Pharmacy. Graedon Enterprises, n.d. Web. 7 Feb. 2014. <http://www.healthcentral.com/static/pp/pdf_guides/nutrient.pdf>. "Gastritis." University of Maryland Medical Center. University of Maryland , n.d. Web. 6 Feb. 2014. <http://umm.edu/health/medical/altmed/condition/gastritis>. "Gastritis." Peptic Ulcer Disease. Merck Manual, n.d. Web. 7 Feb. 2014. <http://www.merckmanuals.com/professional/gastrointestinal_disorders/gastriti s_and_peptic_ulcer_disease/gastritis.html>. "Intravenous Rehydration." Healthlines RSS News. N.p., n.d. Web. 7 Feb. 2014. <http://www.healthline.com/health/intravenous-rehydration#Intro>. "Medical Dictionary, Medical Terminology." Medical Dictionary. N.p., n.d. Web. 4 Feb. 2014. <http://www.medilexicon.com/medicaldictionary.php>. "National Digestive Diseases Information Clearinghouse (NDDIC)." Gastritis. US Department of Health and Human Services, n.d. Web. 7 Feb. 2014. <http://digestive.niddk.nih.gov/ddiseases/pubs/gastritis/>. Nelms M, Sucher K, Lacey, K., Habash, D., Roth S. Nutrition Therapy and Pathophysiology. 2nd ed.Belmonte, CA: Thomson Brooks/Cole, 2010. Parrish, Carol Rees. "Post-Gastrectomy: Managing the Nutrition Fall-Out." Nutrition Issues in Gastroenterology. N.p., n.d. Web. 7 Feb. 2014. <http://www.medicine.virginia.edu/clinical/departments/medicine/divisions/dig estive-health/nutrition-support-team/nutrition-articles/radiganarticle.pdf>. "Peptic Ulcer." NY Times Health. NY Times, n.d. Web. 7 Feb. 2014. <http://www.nytimes.com/health/guides/disease/peptic-ulcer/diagnosis.html>. "Products." Nestle Health Science. Nestle, n.d. Web. 7 Feb. 2014. <http://www.nestlehealthscience.us/products>. "WBC count: MedlinePlus Medical Encyclopedia." U.S National Library of Medicine. U.S. National Library of Medicine, n.d. Web. 5 Feb. 2014. <http://www.nlm.nih.gov/medlineplus/ency/article/003643.htm>.