Integrating Medical Students into the Office Setting.
advertisement

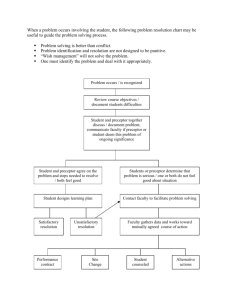
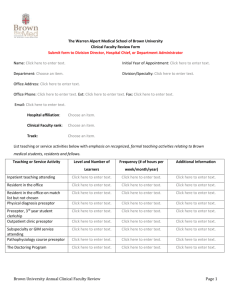
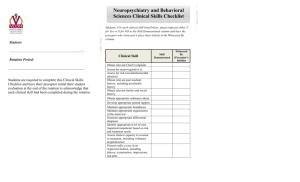
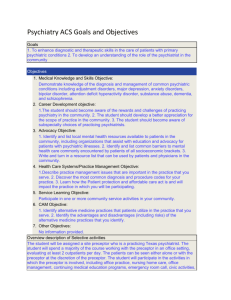
INTEGRATING MEDICAL STUDENTS INTO THE OFFICE SETTING Basics Program for New Faculty Day 2: November 14, 2013 Dr. Steve Kahane, MD CCFP, FCFP, Assistant Professor, DFCM Dr. David Palmer, MD CCFP, Assistant Professor, DFCM Find this presentation online This presentation can be downloaded from www.dfcmopen.com/item/basics-medstudents-office. About this presentation This module is one of a series from the Department of Family and Community Medicine, University of Toronto. It is part of a three-day workshop that is provided to new family physician teachers, that is, faculty members in our Department Presentation Overview In this presentation and accompanying checklists, you will learn how to welcome and orient medical students into your practice. We describe how to prepare patients and staff for medical students, how to adjust your schedule for teaching and plans for what to do when you are behind. The checklists summarize and help you the the orientation process with your medical students. INTEGRATING MEDICAL STUDENTS INTO THE OFFICE SETTING Slides adapted from original iteration of The Basics Program Dr. Merilee Brown, MD CCFP Dr. Steve Kahane, MD CCFP University of Toronto DFCM FACULTY/PRESENTER DISCLOSURE • Faculty: Steve Kahane and David Palmer • Relationships with commercial interests: • Not Applicable DISCLOSURE OF COMMERCIAL SUPPORT • This program has received NO Commercial support • This program has received NO in-kind support • Potential for conflict(s) of interest: – Not Applicable MITIGATING POTENTIAL BIAS • Not Applicable OBJECTIVES • Describe how to welcome & orient students into your practice • Describe how to prepare patients for medical students • How to prepare staff for medical students • Describe how to adjust your schedule for teaching • Plans for what to do when you are behind • Provide checklists summarizing the orientation process WELCOME & ORIENTATION • Student Orientation Checklist • Contact student prior to start date – email/phone • What should student bring? – stethoscope, tools, dress code, ID badge • Plan student’s schedule, dates in office • Get student’s contact information, give your info • Any special needs? WELCOME & ORIENTATION Student Orientation Checklist Orientation Topics: General Learner work space, reference materials * Dress code: name tag, lab coat? * Hours/ days patient care provided, schedule Parking, phone system, email * Introduce staff, each one’s responsibilities * Unique learning opportunities (clinical activities, patient population, provider interests) Orientation to community Community characteristics * Community resources, arranging visits to them * Where to buy groceries, do laundry * Overview of rotation Relate rotation to learner’s career plans Introduction to learner Rotations completed * Experience and skills mastered Areas needing work Expectations of School or Residency Course objectives Criteria included in evaluation form Learner Objectives Specific knowledge, skills, and attitudes to develop Grade expectations Rotation objectives Requirements based on practice’s unique learning opportunities Specific knowledge, skills, attitudes you notice learner needs to work on * Topics that office staff might go over with learners Preceptor Expectations: Daily routine Hours/ days learner in the office Learner’s level of responsibility and autonomy in providing patient care Hospital rounds, night/weekend call Times preceptor is off; what to do Amount of reading expected Office policies Directions for writing chart notes, dictating, writing Rxs, referrals How pts selected for learner to see Length of time to spend with each pt Hospital policies Values Show respect to pts & staff; how? Professionalism Get to know patients Preceptor/learner interaction Format for case presentations Regular time & process for feedback Integrate teaching and learning styles Learner needs to explain needs Criteria to evaluate learner (“what it takes to get honors”) Learner self-evaluation before discussing preceptor’s evaluation If a problem arises Absentee policy, how to notify office A contact for questions or problems How to reach preceptor in emergency From http://www.mahec.net/pdp/e-Learning_Tools.asp WELCOME & ORIENTATION Meet and Greet: •15-30 min before first clinic starts •Complete student information form •Review student’s experiences, rotations, career goals, interests, hobbies •Review course objectives •Review preceptor expectations •Student objectives – expectations, specific learning needs, goals •Review evaluation criteria •Review office policies, procedures WELCOME & ORIENTATION Student Information Form STUDENT NAME: ___________________________________________________________________________ MEDICAL SCHOOL: _________________________LEVEL OF TRAINING: ______________________________ DATES OF ROTATION: _______________________________________________________________________ CONTACT INFORMATION: PHONE:____________________________________________________________ PAGER:____________________________________________________________ EMAIL:_____________________________________________________________ WHAT I DID BEFORE MEDICAL SCHOOL: _______________________________________________________ ROTATIONS/ELECTIVES COMPLETED:_________________________________________________________ AREAS OF MEDICAL INTEREST: ______________________________________________________________ AREAS OF INTEREST OUTSIDE MEDICINE:______________________________________________________ AREAS THAT I FEEL CONFIDENT ABOUT MY SKILLS:_____________________________________________ AREAS OF DEFICIENCY/AREAS I WANT TO WORK ON:____________________________________________ WHAT I HOPE TO DO AFTER I COMPLETE MY TRAINING: __________________________________________ ___________________________________________________________________________________________ OBJECTIVES FOR THIS ROTATION:_____________________________________________________________ ___________________________________________________________________________________________ LANGUAGES SPOKEN:_______________________________________________________________________ IS THERE ANYTHING THAT YOU DO NOT EAT? __________________________________________________ DO YOU HAVE ANY SPECIAL NEEDS I NEED TO ACCOMMODATE (CHILD CARE SCHEDULES, TIMES NEEDED OFF, ETC.)?___________________________________________________________________ WELCOME & ORIENTATION Office Walk-Through: •Orient to office space, exam rooms, supplies, patient flow, bathroom, place for student’s stuff, desk space •Introductions – staff, MDs, Allied Health Care •Orient to charts – paper/EMR (?login and password) •Record keeping - Soap notes, format •Orient to requisitions, diagnostic imaging, labs •How to track student results, follow-up on tests? Mailbox? •Exam room set-up 1 or 2+ rooms? •Where will the student stand in rooms? Extra chair? •Video camera for taping student interviews •Access to Information: Internet, library, guidelines, handouts PREPARE PATIENTS • • • • • • • • • Avoid Surprises! Signs – front desk, exam rooms Reception to advise patients when booking Reception to ask patients when arriving Nurse to ask patients when going into exam rooms Physician to ask patients before seeing them Students to ask patients as they enter room Patients can refuse – have a backup plan Negotiate with patients – observe only, see student first, see with preceptor, see on own SAMPLE WALL SIGN The University of Toronto has recognized this practice for training of family physicians. During your visits to the clinic, you may be cared for by a family practice physician in training. These doctors work under the supervision of a faculty staff physician. Please speak with the staff if you have any questions. Thank you for your cooperation. The Department of Family and Community Medicine University of Toronto Faculty of Medicine 500 University Avenue Toronto, ON M5G 1V7 SAMPLE WALL SIGN PREPARE PATIENTS Introduce the student: • “Hello Mr. Jones. This is Kim Rogers; she is a 3rd year medical student from U of T working with me today. Would you mind if she observes our visit today?” Have student introduce themselves: • “Hello Mr. Jones, I am Dr. John Smith. I am a Resident from U of T working with Dr. Palmer. He has asked me to see you first, and then he will come in to review after we are finished. Is this ok with you?” PREPARING THE STAFF • • • • Tell your staff ahead of time! Educate staff about student and teaching Describe benefits of having student Describe how the student will be involved – observer, seeing from your list, or own list • Any need to change booking methods? • Give student’s schedule to staff • Give student’s contact information to staff PREPARING THE STAFF • Get feedback from staff on how to integrate trainees – they know your schedule best! • Get feedback from staff on trainee for evaluations • Tell other MDs about students and teaching • Ask other MDs or Allied health care team if student can see interesting cases, procedures, spend time with them • Staff attitudes toward teaching are critical PATIENT SCHEDULING Getting Organized: •Extra 15-30 min/half-day … •3 exam rooms ideal (2 for you, 1 for student) •Students take longer (20-30 min/patient) •Medical Students: 1-2 per hour •Residents: 2-5 per hour Type of Schedule? •Separate student schedule or work from yours? •Leave empty space in schedule or book full? •Review schedule with your staff ahead of time •See examples of booking PATIENT SCHEDULING Selecting Patients: •Review your schedule with student before start of clinic •Preceptor selects cases for students - avoid certain patients •Student selects cases - based on needs, objectives Seeing Patients: •Student shadows preceptor (often at beginning) •Student sees patients independently •Focus or prime student - take history, limited exam, task •Student sees patient with preceptor – have student perform a skill while you watch (BP, take history), be a fly on the wall •Set time limits, review tasks, plan when/how to review case •You see 1 or 2 patients, while student sees 1, then review PATIENT SCHEDULING Other things to consider: •Book specific types of patients for student day •Pull learner in for interesting cases •Continuity of care - get student to see patients in follow-up, rebook with student •How will the student follow-up on cases, results? (ie. add student’s name to lab requisition, put results aside, mailbox, EMR) •Consider other office activities – spend time with Office Manager, Reception, Nursing, Dietitian, etc •Teach them basics of billing, diagnostic codes •FHG, FHO, FHT, etc. •Scheduling and work-life balance PATIENT SCHEDULING Sample Schedule: No change, student shadowing 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am HTN DM Cholesterol Well Baby Sprain Flu Depression (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) Dr. David Palmer - Integrating Medical Students into the Office Setting PATIENT SCHEDULING Sample Schedule: No change, but select patients for student 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am HTN DM Cholesterol Well Baby Sprain Flu Depression (Student + Preceptor) (Student) (Preceptor) (Student + Preceptor) (Student + Preceptor) (Student) (Preceptor) Dr. David Palmer - Integrating Medical Students into the Office Setting PATIENT SCHEDULING Sample Schedule: Leave empty space 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am 10:10 am 10:20 am HTN (Student) DM (Preceptor) Cholesterol (Preceptor) Well Baby Sprain Flu (Student) (Preceptor) (Preceptor) Depression (Student) Dr. David Palmer - Integrating Medical Students into the Office Setting PATIENT SCHEDULING Sample Schedule: Separate rooms (“Double Book, Book, Review”) 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am Room 1 (Student) URI Room 2 (Preceptor) HTN DM Review Cholesterol Sprain Flu Review Well Baby Depression Dr. David Palmer - Integrating Medical Students into the Office Setting ENSURING PATIENT FLOW • • • • • • • Trainee doesn’t have to see every patient Student sees case, then break to read around it Avoid difficult or problem patients Focus / limit your teaching (One Minute Preceptor) Basic principles vs. detailed medical knowledge Teach at breaks / between patients Review cases at end of day, take home points, reading • Non-teaching time for student WHEN BEHIND • • • • • • • • Ask learner to chart /read / look up question Set strict time limits for slower trainees Go and rescue student Have student shadow you for a few cases Have the trainee work with your staff Choose simpler patients if appropriate Save it for later – write it down, and discuss after clinic Just stop teaching, and have student take a break ATTITUDE IS EVERYTHING • • • • Role Model Positive Attitude Professionalism Work-Life Balance SUMMARY • • • • • • • Welcome and orient the student Prepare your patients Prepare your staff and colleagues Adjust your schedule Maintain flow, and find time to teach Have a positive attitude Use the Checklist for help STUDENT INTEGRATION CHECKLIST WELCOME AND ORIENTATION: PREPARE PATIENTS: Orientation Checklist Contact student prior to start date – email/phone What should student bring? – stethoscope, tools, dress code, ID badge Plan student’s schedule, dates in office Get student’s contact information, give your info Any special needs? Meet and Greet 15-30 min before first clinic starts Complete Student Information Form Review student’s experiences, rotations, career goals, interests, hobbies Review course objectives Review preceptor expectations Student objectives – expectations, specific learning needs, goals Review evaluation criteria Review office policies, procedures Office Walk-Through Orient to office space, exam rooms, supplies, patient flow, bathroom, place for student’s stuff, desk space Introductions – staff, MDs, Allied Health Care Orient to charts – paper/EMR (?login and password) Record keeping - Soap notes, format Orient to requisitions, diagnostic imaging, labs How to track student results, follow-up on tests? Mailbox? Exam room set-up 1 or 2+ rooms? Where will the student stand in rooms? Extra chair? Video camera for taping student interviews Access to Information: Internet, library, guidelines, handouts Avoid Surprises! Signs – front desk, exam rooms Reception to advise patients when booking Reception to ask patients when arriving Nurse to ask patients when going into exam rooms Physician to ask patients before seeing them Students to ask patients as they enter room Patients can refuse – have a backup plan Negotiate with patients – observe only, see student first, see with preceptor, see on own PREPARE STAFF: Tell your staff ahead of time! Educate staff about student and teaching Describe benefits of having student Describe how the student will be involved – observer, seeing from your list, or own list Any need to change booking methods? Give student’s schedule to staff Give student’s contact information to staff Get feedback from staff on how to integrate trainees – they know your schedule best! Get feedback from staff on trainee for evaluations Tell other MDs about students and teaching Ask other MDs or Allied health care team if student can see interesting cases, procedures, spend time with them Staff attitudes toward teaching are critical STUDENT INTEGRATION CHECKLIST SCHEDULING: • etting Organized G Extra 15-30 min/half-day … 3 exam rooms ideal (2 for you, 1 for student) Students take longer (20-30 min/patient) Medical Students: 1-2 per hour Residents: 2-5 per hour Type of Schedule? Separate student schedule or work from yours? Leave empty space in schedule or book full? Review schedule with your staff ahead of time See examples of booking Selecting Patients Review your schedule with student before start of clinic Preceptor selects cases for students - avoid certain patients Student selects cases - based on needs, objectives Seeing Patients Student shadows preceptor (often at beginning) Student sees patients independently Focus or prime student - take history, limited exam, task Student sees patient with preceptor – have student perform a skill while you watch (BP, take history), be a fly on the wall Set time limits, review tasks, plan when/how to review case You see 1 or 2 patients, while student sees 1, then review things to consider • Other Book specific types of patients for student day Pull learner in for interesting cases Continuity of care - get student to see patients in follow-up, rebook with student How will the student follow-up on cases, results? (ie. add student’s name to lab requisition, put results aside, mailbox, EMR) Consider other office activities – spend time with Office Manager, Reception, Nursing, Dietitian, etc Teach them basics of billing, diagnostic codes FHG, FHO, FIT, etc. Scheduling and work-life balance ENSURE PATIENT FLOW: • Trainee doesn’t have to see every patient Student sees case, then break to read around it Avoid difficult or problem patients Focus / limit your teaching (One Minute Preceptor) Basic principles vs. detailed medical knowledge Teach at breaks / between patients Review cases at end of day, take home points, reading Non-teaching time for student WHEN BEHIND: Ask learner to chart /read / look up question Set strict time limits for slower trainees Go and rescue student Have student shadow you for a few cases Have the trainee work with your staff Choose simpler patients if appropriate Save it for later – write it down, and discuss after clinic Just stop teaching, and have student take a break STUDENT INTEGRATION CHECKLIST Sample Schedule: No change, Student shadowing Sample Schedule: Leave empty space 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am 10:10 am 10:20 am HTN DM Cholesterol Well Baby Sprain Flu Depression (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) (Student + Preceptor) HTN (Student) DM (Preceptor) Cholesterol (Preceptor) Well Baby Sprain Flu (Student) (Preceptor) (Preceptor) Depression (Student) Sample Schedule: No change, but select pts for student Sample Schedule: Separate rooms (“Double Book, Book, Review”) 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am 9:00 am 9:10 am 9:20 am 9:30 am 9:40 am 9:50 am 10:00 am HTN DM Cholesterol Well Baby Sprain Flu Depression (Student + Preceptor) (Student) (Preceptor) (Student + Preceptor) (Student + Preceptor) (Student) (Preceptor) Room 1(Student) URI Room 2 (Preceptor) HTN DM Review Cholesterol Sprain Flu Review Well Baby Depression Dr. David Palmer - Integrating Medical Students into the Office Setting REFERENCES • Brown, Merilee and Kahane, Steve. Original Presentation from The Basics Program, Integration of Students into the Office Setting, 2006. • Palmer, David. Integrating Medical Students into the Office Setting. Presentation for Orientation of New Faculty, Family Medicine Longitudinal Experience, 2011. • Rubenstein, W. & Talbot, Y. Medical Teaching in Ambulatory Care, Second Edition . Springer (2003) • Mountain Area Health Education Center (MAHEC) Department of Continuing Medication Education: Integrating the Learner into the Busy Practice. (http://www.mahec.net/pdp/eLearning_Tools.asp) • Sheet, KJ, Harris DL. Questions asked by family physicians who want to serve as preceptors. J. Fam Pract 1996;42:503-11. • Langlois JP. Support of Community Preceptors: what do they need? Fam Med 1995; 27(10)641-5. • Freeman, Risa. Teaching 101. Power Point Presentation. Updated 2005