Blood Plasma Composition: Biochemistry Presentation
advertisement

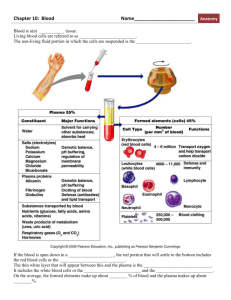
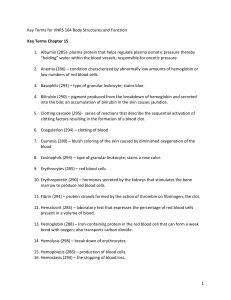
Chemical Composition of Blood Plasma • Terms. Mechanics of investigation. • High- and low- MW compounds of bl.pl. • Interpretation of investigations in clinical practice: – “Basic set” – Disorders of the kidneys and internal environment – Inflammation – Liver disorders Basic terms and mechanics of investigation • Serum = liquid remaining after clotting – usefull for most biochem. tests • Plasma = whole blood - cells – emergency tests – small samples (yield is greater) – clotting tests • The mechanics of investigations – Blood collection: venepuncture Biochemical abnormalities are important markers of disease • Diagnosis = history + examination + biochemical tests + imaging techniques • Treatment: monitoring of the response to therapy in both acute and chronic disorders • Prognosis and secondary prevention • Screening: detecting the non-apparent disease, eg. PKU or hypothyreosis Low-molecular weight compounds of blood plasma • Cations: Na+, K +, Ca + + + • Anions: Cl , HCO3-, HPO42-, HSO4• Metabolites: urea, creatinine, uric acid, bilirubin • Nutrients: glucose, FFA, ketones • Other High MW compounds of blood plasma (= proteins) • According to the function – oncotic pressure – clotting factors and fibrinolytic agents – transport: binding proteins, apoproteins – antibodies and complement: IgG, IgM – buffers – none: enzymes used for diagnostics • Electrophoretic separation: prealbumin, albumin, α-, β-, γ-globulines Internal environment and the blood buffers • Basic life conditions: – isoionia: concentrations of certain ions must be kept in narrow range – isoosmia: osmotic pressure is allways the same in ECS and in cells (in dehydratation osmotic pressure rises) – isohydria: pH = 7.35 - 7.45 • Blood buffers: bicarbonate, hemoglobine, proteins and phosphate Internal environment investigation • Water metabolism: osmolality, Na+ • Acid-base balance disordes: “Astrup“ – taken from arterial blood – pH, pO2, pCO2, HCO3-, BE, BB, AG, lactate • Kidney failure: K+, urea, creatinine, phosphate and sulphate retention • Respiration failure: pO2 decrease with/without pCO2 increase Inflammation • History + examination • Changes in the blood count (eg. leucocytosis) and sedimentation rate • Non-specific inflammatory markers: eg. CRP and fibrinogen • Specific antibodies: IgG or IgM (ELISA) • Antigen assays: eg. HBsAg Assays for liver and billiary tract function and disease • Parenchyme damage: – increase in enyzme activity in plasma: ALT, AST, ALP, GMT • Alteration of liver function: – bilirubin accumulation (jaundice) – alteration of protein synthesis: hypoalbuminaemia, clotting disturbancies „Basic set“ • Taken from most of the patients admitted to hospital • Give to the physician basic overview about patient’s metabolic state and organ functions • Contains: – Na, K, Cl, glycaemia – liver set: ALT, AST, bilirubin, (ALP, GMT) – kidney set: urea, kreatinine – blood count and FW – urine examination + sediment