Colorado Health Benefits Exchange
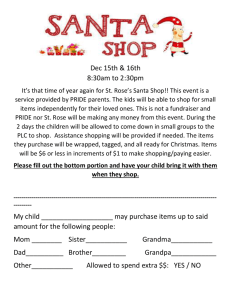
advertisement

IT and Implementation Committee Strategic IT Decisions December 14, 2011 1 • Discussion points from 12/12 Board meeting • “Optimal” Level of “Interoperability” with State Medicaid/CHIP Systems and Business Processes • Storyboard • Areas of Potential Interoperability and Input (IT, Call Center, Plans) • Cost Allocation of Interoperability • Additional Information from RFI process • Path Forward 2 3 • • Input into RFP • Risk management • Ask vendors how they would reduce implementation risk • Ask vendors how they would reduce operational risk (2+ options; pros/cons of each; one biased towards pmpm and one pmpm neutral • How will they align with the COHBE on a sustainable basis • Heavy weighting on call center / customer service experience • Provide COHBE latitude to create partnerships with “best of breed” companies by unbundling (recommend one technology solution for SHOP and individual exchanges) Evaluation Team • • • 6 – 8 members is ideal HCPF will participate Concerns re adequacy of IT resources • Developing options 4 5 CBMS/PEAK & Medicaid/CHIP Eligibility & Enrollment Business Processes Interoperability Between COHBE & State Medicaid/ CHIP Systems and Business Processes COHBE Eligibility & Enrollment Systems and Business Processes Extent of “interoperability” (i.e. amount of overlap) between COHBE system and business processes and CBMS/PEAK and associated State eligibility and enrollment business processes increase s complexity and schedule risk but improves some consumer populations’ experience 6 Moderate Interoperability – MAGI & MMIS Interface COHBE Systems Small Business Owners & Employees Pre-screening SHOP Exchange Account Mgmt & MPI Eligibility Determination Set-up Employee Roster Create Account Eligible for Employer Plan & Amount of Coverage (% and # expected) Individual Households & Small Business Employees Plan Selection & Enrollment Enrollment in Carrier Systems Review Out-ofPocket Costs Select Plan & Enter Enrollment Information Interface Enrollment Information to Carriers’ Systems Individual Exchange Should PreScreening Step be Included? MAGI Create Account (including interfacing w/ federal data hub) Review Subsidy/Outof-Pocket Costs Select Plan & Enter Enrollment Information (% and # expected) Enroll Eligible Household Members into Family Medical Program into MMIS State Systems Household Member(s) Eligible for Other Medical or HS Programs Individual Households (seeking public assistance, i.e. Medical, Food or Cash Assistance) (% and # expected) PEAK CBMS MMIS Interface Enrollment Information to MCO Systems Does CBMS Need Enrollment Data? 7 Approach to Determining Optimal Interoperability Strategy Moderate Interoperability – MAGI & MMIS Interface Pre-screening Small Business Owners & Employees SHOP Exchange Account Mgmt & MPI Eligibility Determination Set-up Employee Roster Create Account Eligible for Employer Plan & Amount of Coverage (% and # expected) Individual Households & Small Business Employees Plan Selection & Enrollment Enrollment in Carrier Systems Review Out-ofPocket Costs Select Plan & Enter Enrollment Information Interface Enrollment Information to Carriers’ Systems Individual Exchange Should PreScreening Step be Included? MAGI Create Account (including interfacing w/ federal data hub) Review Subsidy/Outof-Pocket Costs Select Plan & Enter Enrollment Information (% and # expected) Enroll Eligible Household Members into Family Medical Program Into MMIS Who pays for this interface? Individual Households Gather technical requirements Prioritize all interoperability requirements, i.e. musts, strong wants, nice wants (and who) Define interoperability “musts”” for 2013 including ACA Gather business requirements Prioritization of Requirements Requirements Musts a b c d e f g h i j k l X Strong Wants X X X X X X X X X X Evaluate feasibility of design alternatives Test use cases for impact on consumer considering design principles, guiding principles and best practices (% and # expected) Develop 3 options with increasing levels of interoperability, complexity, risk, costs, etc. PEAK CBMS MMIS Interface Enrollment Information to MCO Systems Does CBMS Need Enrollment Data? Define design alternatives (functions and feature sets for each option) Tiered Sets of Requirements Nice Wants X (seeking public assistance, i.e. Medical, Food or Cash Assistance) Requirements a c j b e g k d f h i l “Musts” Option 1 Option 2 Option 3 X X X X X X X X X X X X X X X X X X X X X X X Strong “Wants” Nice “Wants” Define scope for Exchange System(s) and Services (RFP/RFQQ) Begin Formal Exchange Acquisition Process Compare feasible alternatives against criteria; Draft & Submit IAPD make recommendation Define scope for modifications to PEAK & CBMS Draft/Negotiate Deloitte SOW 8 Interoperability System and Business Process Alternatives • Minimum level of systems interoperability (from design principles, guiding principles and best practices): • • • • • • • • • Moderate level of systems interoperability: • • Single/shared MAGI eligibility process for Private Insurance and Medicaid/CHIP Single sign-on Comprehensive MPI (Exchange and Medicaid/CHIP population) Data only entered once Request only information needed for determining eligibility for healthcare Maximize “no touch” eligibility adjudications Interface from PEAK to MAGI process to support “no wrong door” requirement for medical eligibility Provide links to non-medical eligibility processes and pre-populate with data previously collected during medical eligibility processes Interfaces • TBD Maximum level of systems interoperability: • TBD 9 Tiered Sets of Requirements Interoperability Level Interoperability Feasibility Criterion Impact on Exchange RFP Minimum Moderate Maximum X X X No "wrong door" Shared MPI and Account Management No data entered more than 1x; re-use data Do not ask for data not relevant to medical eligibility X X X X X X X X X X X X Meet all minimum ACA reqs X X X Common "no touch" MAGI eligibility Shared call center Same carriers for some private and public plans Interface PEAK to Exchange for MAGI Eligibility Link and data population Exchange MPI to PEAK Interface Exchange to CBMS for other medical and human services TBD TBD X X X X X X X X X X X 10 Analysis of Alternatives – use cases and preliminary estimate of populations Subsidized Unsubsidized Medicaid EmployeeCombo Private Private CHIP Only SHOP X X X Unemployed uninsured with 382 children plus 1/2 public insured X 7 One fourth of expected small firm 100 participants X One fourth of expected small firm 100 participants X X One fourth of expected small firm 100 participants Currently unemployed w/private 300 insurance plus 1/2 public insured X One fourth of expected small firm 100 participants X 5 6 Preliminary X 3 4 Currently buying private 300 insurance X 1 2 Spouse All-Family TANF Food People SHOP SHOP Stanps 1000s X 11 Use Cases and interoperability considerations System Entry Point COHBE Use Case Construct Individual Household Household Composition Use Cases Eligible for subsidy Population TBD expected to be >200K TBD Not eligible for subsidy SHOP PEAK/CBMS Single person TBD Childless couple TBD Family including TBD children Program Eligibility Family Medical Eligible for Family Medical CHIP Eligible for CHIP Long Term Care Eligible for LTC Disability Eligible for Disability TNAF Eligible for TNAF SNAP TBD expected to be > 300K TBD TBD TBD What is intersecting population? Eligible for SNAP What is intersecting population? Eligible for Subsidized Private Coverage Account PEAK Interface MMIS Interface CB MS Interface Carrier Plans Mgmt/MPI/M (MCOs) AGI Y N/A N/A N/A N/A Y Y N/A N/A N/A N/A Y Y Y Y N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A Y Y Y Y Y Y N Y Y Y Y Y Y Y Y Y Y N N N Y Y Y Y not in COHBE Y not in COHBE Y Y Y Y Y Y Y N N N N/A Y Future Y N N N N/A Y Future What is this population? CHIP Eligible Call Center Eligible for SHOP Coverage What is this population? Rules Engine Other CHIP Eligible 12 • Storyboard shows moderate level option of interoperability COHBE and HCPF End-to-End Solution – Preliminary High Level Business Process and Systems Model Core Exchange Functions Eligibility Initial Screening Business Processes Business Objective for Each Process Determine if individual wants to see if he/she qualifies for financial assistance, i.e. Medicaid/CHIP or subsidized private coverage Collect minimal personal data and make preliminary determine if individual qualifies for financial assistance, i.e. Medicaid/CHIP or subsidized private coverage. No confidential information requested. SHOP employers and brokers must create an account to proceed with SHOP coverage administration and account management. Individual must create account in order to enter personal data which will be stored and verified by interfacing with federal data hub Individual enters required information, creates password, answers challenge questions, etc. COHBE and PEAK Entry Points (Portals) COHBE & State Systems Broker Accesses CHOBE Broker Tools and Authorized SHOP Employer Information Brokers SHOP Employers Brokers and SHOP Employees SHOP Employer Broker or SHOP Employee Small Employers and Employees Manage SHOP Employee Roster and Benefits is accessed only in the COHBE. It is for establishing and administering benefits for SHOP employees. It defines who is eligible for what Metal of coverage. This process is not applicable to SHOP employees, individuals or households. Insurance Exchange Marketplace is a presentation of plans for which the user is eligible. Tools to search, sort and compare plans along a variety of dimensions such as price, deductable, location/ availability of network and out of network providers Eligibility Determination #2 is the determination if and to what extent an individual meets the criteria for a given category or categories of medical coverage. This will be performed by applying business logic to a set of data the required data will be different depending on the type of coverage, it may include but is not limited to: age, smoking, disability status, income, assets [resources], medical expenses, etc.) COHBE Only Plan Selection Plan Selection is the action of selecting a plan in the Marketplace COHBE & State Systems Plan Management Financial Management Tax Credits and Advance Aggregation of Approve and Load QHP Payment of Premiums Premiums Enrollment Enrollment is the assignment of eligible individuals to health care plans that are available to that eligibility category. Plans may be restricted to eligible beneficiaries based on geography, funding stream, or other criteria. (Enrollment generally includes options to choose a plan, but may also have a time-driven default assignment based on a fairly sophisticated algorithm that could include geography and funding streams, but also could include patients previous care providers, an agreement for the exchange to allocate default assignments according to some percentage across plans, or other criteria to be determined, etc.) Aggregate information and transactions Aggregate information and transactions Plan Management is the processes to get State-approved QHP from carrier systems into the Exchange Carrier Operations and Backoffice Functions Approval Guaranteed-issue health insurance coverage – which ensures that individuals are not denied coverage or forced to pay higher premiums because of preexisting conditions or poor health status may, require the gradual elimination of medical underwriting due to the restrictions outlined in the bills on rating practices and the requirement that all individuals have access to coverage regardless of their health conditions. Fulfillment Yes SHOP Employer and/or Broker Administer Benefits and Account SHOP Employer Authorizes Broker to Access Employee Information Carrier Systems SHOP Employee Presented Plans Based on Eligibility and Search Criteria Display Benefit, Out-of-Pocket Cost, etc. Present Medicaid/CHIP plans if available (and provide search capabilities) e.g.: · Location · Network · Costs/Co-pay · Benefits · Specialties · Other CUE3 SHOP Employee completes on-line application to capture any additional required information (pre-populate to max extent possible) SHOP Employee Selects Plan/ Coverage Type Show total cost and cost breakdown and terms and conditions Collect any additional information Obtain user acceptance & e-signature Process financial transaction (if applicable) Enroll Individual/Family Members in Carrier Plans Assign Individual/Family Members to Pools Approve Assignments Send Medical Cards Administer/Pay Claims High-Level Requirements May receive assistance from: · Navigator/Broker/Agent · Case worker · Community-based worker · Volunteer(?) SHOP Employee Creates an Account or Logs In Employees Rules Engine Cascading Eligibility CUE Based on application information business rules make determination re eligibility for Medicaid/CHIP or Other Likely Medical Benefit Account Management Master Data Management Paper Application May be Eligible for Medicaid/SCHIP (Including Expansion) SHOP Individual and Household w/ Income between 133% and 200% PL Federal Data Hub Likely Eligible for Medicaid/SCHIP Show SHOP Employee Eligibility for any Additional Medical Benefits (Public or Private) CHIP Eligible Children? Hotline Calculator Medicaid/CHIP Eligibility Screening Standardized Enrollment CUE5 Does SHOP Employee /Individual Want to Enroll Children in CHIP? Yes CUE6 Enrollment Periods CUE7 Navigators PC2 CUE4 Based on application information business rules make determination re eligibility for Medicaid/CHIP or Other Likely Medical Benefit CUE1 Individuals/ Households SHOP/ Financial Assistance Yes or No Yes User Enters: - Resident of KS - Zip Code - Age - Family or Individual - Income - SHOP ID - Excemptions CUE8 Individual Creates Account In COHBE 350K Call-in Show Individual/Household Eligibility for any Medical Benefits (Public or Private) CUE9 No Individual and Household w/ Income between 133% – 400% PL Rules Engine Cascading Eligibility Consumer Information Inform consumers of plan quality and enrollee satisfaction ratings. Exemptions Have the capability to identify, and inform the U.S. Treasury, about consumers who are exempt from the law’s individual responsibility requirements. Preliminary Eligibility Determination for Subsidized Private Coverage (show estimated and nonverified subsidy amount) Likely Eligible for Subsidized Private Coverage Individual Selects Plan/ Coverage Type Show total benefit package and terms and conditions Collect any additional information Obtain user acceptance & esignature Coverage for a federally determined essential benefits package (as well as any other benefits the state requires) in a plan that has the required out-of-pocket caps; The offering of only specified tiers of coverage: bronze, silver, gold, and platinum. A bronze plan covers 60 percent of medical costs for covered services (excluding premiums) for an average enrollee population; silver covers 70 percent; gold covers 80 percent; and platinum covers 90 percent.2 Any insurer participating in the exchange must offer at least one plan at the silver level and one plan at the gold level. Insurers may also offer “catastrophic” plans for people under 30 and people who are exempt from the individual responsibility requirements (see Section 1302 of the Affordable Care Act). Essential Benefits PC2 Plan Offerings PC3 Number of Network Providers PC4 Marketing Standards Availability of an adequate number of providers in the plan’s network, including providers that serve predominantly low-income, medically underserved individuals (where applicable). Marketing standards. PC5 Quality and Accreditation Specified quality, quality improvement, and accreditation standards. PC6 Transparency Transparency standards, such as disclosure of information on claims denials, plan finances, cost-sharing information, and enrollee rights in plain language. PC7 Preimum Increases Prior justification of any premium increases (which will be made public, and which exchanges are asked to consider when determining whether to allow an insurer to participate). OR Additionally, Exchanes must meet these additonal requirements. OR1 Stakeholder Participation OR2 Transparency Exchanges must publish specified financial information for public inspection and must undergo annual audits by the Secretary of Health and Human Services. Financial Stability Exchange administration must be self-financing by January 1, 2015 (through premiums or other sources). Until 2015, federal grants will be avaialable to help states implement exchanges. Enroll in selected plan Send Subsidy Transactions to US Treasury and Carriers OR3 Consumer and public input: Exchanges must consult with stakeholders, including educated health care consumers, enrollment experts, small business representatives and self-employed individuals, and advocates with experience enrolling hard-to-reach populations. Actual Source Secure Interface from Exchange MAGI Eligibility Process to CBMS CUE Consumer Usability and Enrollment US Treasury Systems/ Subsidy Payments to Carriers and Tax Credits for SHOP Employers Not Eligible for Subsidized Private Coverage Individual and Household w/ Income greater than 400% PL An exchange must be able to certify that plans sold in the exchange meet a number of standards outlined in the Affordable Care Act. PC1 Legend May receive assistance from: · Navigator · County case worker · COHBE customer service · Community-based worker · Volunteer CUE2 Provide for an initial enrollment period as well as annual and special enrollment periods. Establish “navigators”—individuals or entities that help consumers and employers learn about, and enroll in, coverage options. CUE8 1 Implementing Health Insurance Exchanges, A Guide to State Activities and Choices, Familes USA October 2010 Individual completes on-line application May be Eligible for Subsidized Private Healthcare Coverage Private Coverage Individual Presented Private Coverage Eligibility and Search Criteria Display Benefit, Out-of-Pocket Cost, etc. Present Medicaid/CHIP plans if available (and provide search capabilities) based on: · Location · Network · Costs/Co-pay CUE3 · Benefits · Specialties · Other CUE6 PC2 Make an online calculator available so that people can see the actual costs of their coverage after accounting for the premium tax credits they may receive; Be able to screen eligibility for, and enroll people in, Medicaid, the Children’s Health Insurance Program (CHIP), and other public programs. Use a standardized enrollment form for coverage. CUE9 Yes Interface to HHS Data Hub SSA, IRS, HHS, DHS Requirement Description Implement a web portal where consumers and businesses can view coverage options, with benefits and costs presented in a standardized format. Operate a toll-free hotline for consumer assistance. Web Portal CUE2 CUE3 CUE4 CUE4 Requirement Exchanges must be able to enroll individuals and small businesses (with up to 100 workers) into coverage in a user-friendly way. CUE1 PC Preliminary Eligibility Determination for Medicaid/SCHIP (show potentially eligible programs) Renewal Plan Management Does Employee Want to Check Eligibility for CHIP or Subsidized Private Coverage? Yes SHOP Employee Eligible (Defined Contribution) for Employee Only or Employee Household SHOP Employer Creates an Account or Logs In Employers Does Employee have Household Family Members Who are Not Covered? Broker Accesses CHOBE Broker Tools and Authorized SHOP Employer Information Individual CUE7 Premium Collection/ Aggregation Approve and process allowable claims on behalf of enrollee Exchange Only COHBE or State MMIS Operations Provide medical card/proof of insurance when needed Rqmt # Individual Individual and Household w/ Income Less than 133% PL Insurance Exchange Marketplace Eligibility Determination No Broker Creates an Account or Logs In SHOP Enrollment Manage SHOP Employee Roster & Benefits and Admin Tools Account Management Rules Engine Cascading Eligibility Eligible for SHOP CUE2 Effective as of 2014 Call Center and Customer Assistance Main article: Patient Protection and Affordable Care Act#Effective by January 1, 2014 · State health insurance exchanges for small businesses and individuals open. · Individuals with income up to 133% of the federal poverty level qualify for Medicaid coverage. · Healthcare tax credits become available to help people with incomes up to 400 percent of poverty purchase coverage on the exchange. · Premium cap for maximum "out-of-pocket" pay will be established for people with incomes up to 400 percent of FPL.[10][62] Section 1401 of PPACA explains that the subsidy will be provided as an advancable, refundable tax credit[63] and gives a formula for its calculation.[64] Refundable tax credit is a way to provide government benefit to people even with no tax liability[65] (example: Child Tax Credit). According to White House and Congressional Budget Office figures, the maximum share of income that enrollees would have to pay for the "silver" healthcare plan would vary depending on their income relative to the federal poverty level, as follows:[11][66] for families with income 133–150% of FPL will be 4-4.7% of income, for families with income of 150–200% of FPL will be 4.7-6.5% of income, for families with income 200–250% of FPL will be 6.5-8.4% of income, for families with income 250-300% of FPL will be 8.4-10.2% of income, for families with income from 300 to 400% of FPL will be 10.2% of income. In 2016,the federal poverty level is projected to equal about $11,800 for a single person and about $24,000 for family of four.[66] See Subsidy Calculator for specific dollar amount.[67] · Most people required to obtain health insurance coverage or pay a tax if they don't. · Health plans no longer can exclude people from coverage due to pre-existing conditions. · Employers with 50 or more workers who do not offer coverage face a fine of $2,000 for each employee if any worker receives subsidized insurance on the exchange. The first 30 employees aren't counted for the fine. · Health insurance companies begin paying a fee based on their market share. Track Enrollment and Changes to Enrollment Boundary between COHBE and PEAK/CBMS Boundary between COHBE and PEAK/CBMS Boundary between COHBE and PEAK/CBMS Secure Interface to Exchange/ MAGI Eligibility Process from PEAK Visit County Office PEAK CBMS MMIS County case worker enters application and interviews client CBMS determine eligibility for non-MAGI population and other human services programs Individual and Household seeking public assistance for Medical and/orMail SNAP Application HCPF and/or TNAF and/orInto other Center Federal and StateProcessing programs Enroll Individual/Family Members in MMIS Send Medical Cards MAXIMUS employee enters application and notifies client Call Center and Customer Assistance Track Enrollment and Changes to Enrollment KEES Integration with Federal Exchange Version 2.0 September 25, 2011 Gary Schneider 13 Interoperability System and Business Process Alternatives • Shared call center with HCPF • Four types of calls anticipated: 1. 2. 3. 4. • • Exchange call center – eligibility, site, information, assistance, billing, etc. State Medicaid call center (MAXIMUS) – eligibility, claims, etc. Carrier call center – policy questions, claims, etc. Division of Insurance – complaints Should #1 and #2 be combined? (shared /consistent support processes, infrastructure, capacity management flexibility, consumer experience, need for specialization or separation) Carriers offering plans that bridge private and public healthcare coverage to enable household to be covered by one carrier/similar provider network, etc. • Prevalence of “mixed” household populations being researched, e.g. 1. 2. Single parent eligible for subsidized private coverage and children eligible for CHIP. One parent receives subsidized coverage from SHOP employer, spouse eligible for subsidized private coverage and children eligible for CHIP 14 Analysis of Interoperability Alternatives – feasibility of alternatives versus critierai Alternative Cost Description/ Implementatio 5-Year Approach n Costs Operational (federal & Costs (federal SGF) & SGF) Consumer Experience Impact of Change on Workforce Reliability/ Maintainability/ Scalability State of System after Investment (MITA/Tech Arch/Platform) Impact on COHBE Operations and Systems State’s Strategic Direction and Latitude Stakeholder Acceptance Minimum 2013 Interoperability Moderate 2013 Interoperability Maximum 2013 Interoperability 2015 Interoperability 15 Consumer Experience - Make enrolling in coverage for the individual/household as fast and as simple as possible - Balance administrative simplicity, efficiency and effectiveness - Enable continuity of care - Provide user-friendly access to all eligible CO citizens and small CO businesses that desire access - Leverage and integrate with State systems and business processes as appropriate Reliability/Simplicity in Getting Consumer Enrolled - Make enrolling in coverage for the individual/household as fast and as simple as possible - Leverage and integrate with the State system(s) and business processes Reliability/Backend Complexity of Having All Solution Components Fully Functioning - Leverage and integrate with the other systems w/o reducing reliability Privacy and Security - Leverage and integrate security, i.e. account management and MPI - Minimize proliferation and transmission of PII Cost - Minimize costs to the COHBE, consumers, employers and carriers Risk to COHBE Project Deadlines - Minimize Risks of: 1) not meeting federal milestones, 2) delivering baseline scope and 3) completing the project within the baseline budget Strategic Direction and Latitude - Maximize flexibility to change its direction; enable the state to go in a different direction in the future without COHBE or State incurring a large potential cost impact or disruption to end users; this could include a different Exchange solution provider (recompete) or a different Exchange solution direction such as building or buying the HIX software and integrating with State system in future Stakeholder Acceptability - Recognize limitations of interoperability given political realities, funding constraints, etc. 16 17 All state-run procurements. • Maryland – stringent to the point of limiting vendor creativity; all risks put on vendor • Minnesota – structured to get the best functional modules; presents significant integration challenges; Phase 1 complete vendors to built exchange prototypes; available to other states • Washington – design, develop, implement (DDI) model; ignores significant investment in exchanges currently on market; SaaS only solutions excluded • Mississippi – phased approach (e.g. web portal/shop & compare, unsubsidized exchange, subsidized exchange eligibility determination); open to multiple vendors across phases; risky with lots of unknowns (federal guidelines, etc) • Regular conference call with CCIIO indicates that the following states have or will have issued RFPs by the time COHBE RFP is issued (MA, MD, MS, WA, NY, OR, MN) 18 Company Respondents End-toEnd Solution Exchanges Operating Model Benefitfocus Yes Individual & SHOP SaaS only Connecture/ MAXIMUS Yes Individual & SHOP license & SaaS CA, TX, CO, IA, NY Getinsured.com Yes Individual & SHOP license & SaaS MS CGI Yes Individual & SHOP Individual & SHOP license & Saas ACS/Choice/ Current Clients Partners MAGI Rules engine Implements with an independent rules engine custom – proprietary MAXIMUS (prime) designing for MN prototype open source Accenture No Drools Flow (jBPM5) FL, NJ, CT, VA Insurance companies, employers, education systems COTS – HIE360 Federal Exchange, New England states, UT, CMS, CCIIO; hCentive, Exeter, Policy Studies (PSI) Yes SaaS pmpm CO – Anthem BCBS MD – CareFirst BCBS CO broker – Jim Sugden MD – Dell, Oracle, Cognascante No No SaaS only(?) 130,000+ using payroll & benefit mgmt services Solution works with a number of structures No custom Mass HealthConnector Florida w/Ceridian Deloitte (MN & WA) Support – Ceridian No No Vendors w/ partial solution BenefitMall No SHOP Ceridian No Individual eHealth No Individual SaaS only 19 • Information on costs will require additional analysis and follow-up with vendors • Preliminary estimates for Exchange technology and services range from $30 million to $60 million per year w/ implementation costs amortized over 4 years 20 21 COHBE RFP Gamplan RFP Section 1. Purpose of RFP, Vision, Concept of Operations 2. COHBE Background 3. General and Administrative Procurement Information and Timeline 4. Scope of Implementation and On-going Services 5. Proposal Response – System, Implementation Services, On-going Operations and Administrative Services: 5.1 Solution Proposal (business, technical) 5.2 Cost Proposal Key Points/Direction Assist Other Reviewers Materials What/Why/How from 30K ft Benefits and what we're trying to accomplish Need to contain costs for sustainability Information on entity and mission Gary Lead Chuck, Larry Myong, Shawn, Patty Business Concept SB 200 Gary Shawn Myong, Shawn Structured defined procurement process Timeline set for procurement Show timeline for project (SHOP and Individual) Gary Chuck, Larry HCPF Procurement Officer Business Concept SB 200 Briefings Define scope for core areas Define populations System implementation System support and maintainance System hosting and operations Optional application licensing Very prescriptive Response format to be structured and consistent Gary Chuck, Larry Shawn, Patty KS RFP/BAFO Population estimates from CHI, Gruber, etc. Gary Chuck, Larry HCPF Procurement Officer KS RFP/BAFO Vendor description of how solution will function from business and technical perspective Gary Chuck, Larry Shawn KS RFP/BAFO Cost templates will be provided ; line items broken down between implementation and on-going costs to insure ability to accurately compare costs Operations for 1,3,5 years Attempt to segment between technology and labor (services) For pmpm cost risk use ranges on bid schedule Population metrics and pmpm ranges Chuck Larry, Gary Shawn, Patty Gary to provide starting pt See KS and MD cost schedules MD's approach to addressing uncertainty in ACA final rules Gary Chuck, Larry HCPF Procurement Officer HCPF Ts&Cs Larry Chuck, Gary Chuck - Exchange Larry - Medicaid Gary Draft Complete 15-Dec 15-Dec 16-Dec 16-Dec 16-Dec 19-Dec 16-Dec 6. Proposed Contract Terms and Conditions 7. Appendices: Appendix A – Business Process Models 15-Dec Gary has templates 16-Dec Appendix B – Requirements (functional, technical) Functional Gary Technical Appendix C – Interoperability with State Medicaid Systems and Business Processes Appendix F – Reporting and Business Intelligence Gary has starting set Sherri Gary has starting set Chris/Antoinette/ Jenny/Deloitte HCPF work HCPF work Gary will provide format HCPF work Gary will provide format May need help from Jeff Mitchell Look in CALT 16-Dec 16-Dec 16-Dec Build small table Larry Gary Chris/Antoinette/ Jenny/Deloitte PEAK and CBMS into single account management for single sign-on What State systems involved? Need to make sure this is possible Larry Gary Chris/Antoinette/ Jenny/Deloitte Need to get starting set of Exchange metrics ASAP Reach out to MA and UT, Brokers, Carriers, Providers, Health Foundations Chuck Larry,Gary Shawn, Patty Standards Gary Jeff Mitchell Eric/Nathan/Sherri Consider graded cost approach Gary Chuck Eric/Nathan/Sherri COHBE RFI MD RFP KS RFP KS EI grant app KS RFP/BAFO Balance granularity w/ control Ensure data turnover as per Sherri Gary Gary Chuck, Larry Jeff Mitchell Shawn, Patty Shawn, Patty KS RFP/BAFO KS RFP/BAFO Appendix D – Interfaces Appendix E – Conversions Shawn Jim Reiseburg Chris/Antoinette 16-Dec 16-Dec 16-Dec Appendix G – Technical Architecture Appendix H – Operations, SLAs, and Continuity of Operations Appendix I – Deliverables Appendix J – Turnover 18-Dec 19-Dec 13-Dec 13-Dec 22 High-Level Timeline – COHBE Policy & Business Decisions and IT 2011 11/11 2012 01/12 03/12 Policy & Business Decisions and Activities Policy & Business Decisions Impacting IT 05/12 07/12 2013 09/12 11/12 01/13 Supreme Court Ruling on Mandate 03/13 05/13 07/13 COHBE Certification by HHS Evolving Policy and Business Decisions based on CCIIO/CMS/Board/Executive Director/Legislative Oversight/etc. Operational Activities Start-up and Operational Decisions Start-up Activities IT/Systems Pilot Phase 04/13 – 10/13 HIX - SHOP Analysis/Confirmation of Current Approach & Prel RFP Procure IT Systems & Services for HIX Design/Build/Test HIX Systems for SHOP HIX SHOP Integration Testing HIX Deployment Establish PMO Pilot Phase 06/13 – 10/13 HIX - Individual Analysis/Confirmation of Current Approach & Prel RFP Procure IT Systems & Services for HIX Design/Build/Test HIX Systems (Eligibility/Enrollment/Plan Mgmt and Associated Services Interface w/ Federal Data Hub, Other Data Sources, MMIS, PEAK/CBMS) HIX Integration Testing HIX Deployment Note: Accompanying timeline for required enhancements to PEAK 23 & CBMS not shown Category Exchange Functions, Features and Business Processes Guiding Principle Meet the minimal requirements of federal regulations; enhanced functions, features and integration will be considered in the future. New business processes to execute Exchange business processes shall minimize the impact to other State agencies’ business processes or systems. Exchange Customers Customers of the Exchange are individuals and small business owners and their employees. There will be a single Exchange. The Exchange will have two business lines: 1) the SHOP Exchange and 2) and Business Lines the Individual Exchange Market Competition Encourage competition in the market whether it is inside or outside the Exchange. Continuity of Care Ensuring continuity of care is a personal responsibility; the Exchange will not pro-actively enroll or change enrollments of consumers (i.e. individuals and small employers and their employees). Integration with Medicaid Minimize integration with Medicaid eligibility in the near-term; consider tight integration (and possible upgrade of State’s eligibility system) in long-term (i.e. 3-5 years); make investments based on this strategy. Send consumers to the “right” door first but enable cross (MAGI) eligibility determination. Federal Deadlines Work with State Medicaid agency but do not jeopardize meeting federal and state deadlines. Solution Acquisition Leverage existing solutions and solution components from other states and federal partners to the maximum extent possible. Inter-agency Partnerships Work in concert with all State agencies, e.g. HCPF, DHS, OIT and Insurance Department. Regulatory Authority Maintain the Colorado Insurance Department as the single regulator. 24 Exchange Capability and/or Service Category Exchange Capability and/or Service Strawman Priority for 2013 (depends on “who” is asked) High Eligibility, Plan Shopping and Enrollment (System) MAGI eligibility for individuals and households (subsidized coverage and State Medicaid and CHIP) and enrollment SHOP employee eligibility and enrollment Eligibility and enrollment of SHOP employees and their household members in private coverage or State Medicaid and CHIP Multi-dimensional search criteria (network, provider, disease specialty, deductable, co-pay, etc.) Multi-lingual on-line system Directory of available brokers and qualifications Broker-Related Ability for broker to access SHOP employer data Features & Tools Ability to develop comparative quotes and to sort information to (System) support recommendations and decision making Ability for broker to work remotely and one-on-one with employer through the system Plan Management Interfaces/admin tools and associated services for carriers to load plans into COHBE Admin tools and associated services for regulators to approve plans in COHBE Moderate Low Impact on Implementation and Operational Costs Impact on Impact on Implementati Operation on Cost al Costs X High High Moderate Moderate High Moderate Moderate High Moderate Moderate Moderate Low Low Low Moderate Moderate Low Low X Moderate Low X Moderate Moderate X X X X X X X 25 Exchange Capability and/or Service Category Customer Service Financial Management Exchange Capability and/or Service Strawman Priority for 2013 (depends on “who” is asked) Impact on Implementation and Operational Costs Call center support for on-line eligibility and enrollment (individual households, SHOP employees) X Impact on Implementation Cost Moderate Call center support for SHOP employers and brokers X Moderate High Support for carriers Support for regulators Call center for Navigators Print/mail for notices Multi-lingual call center support Customer support for mail-in applications Customer support for walk-in applications X X X X X X X Low Low Moderate Moderate Moderate Moderate Moderate Moderate Low High High High High High X High High X High Moderate X High High Moderate High Moderate High High A/R management (including billings) for premiums from SHOP employers and consumers; A/P management for payment to carriers (system and support) including electronic and paper notifications, invoices and receipts (systems and services) Aggregated premium billing for SHOP employers On-line payment service for individuals and SHOP employers & employees (ACH, credit card) Flexible spending accounts, health reimbursement accounts, health savings accounts (system and support) Managing commissions/ payments to brokers and Navigators (system and services) Moderate X X Low Impact on Operational Costs High 26 Exchange Capability and/or Service Category Exchange Capability and/or Service Strawman Priority for 2013 (depends on “who” is asked) High Other Exchange Features Data repository of all plan/carrier ratings, transactions, enrollments, disenrollments, trend reporting, performance indicators/metrics to support COHBE improvements and to provide useful information to navigators, agents, brokers, carriers, regulators, consumers Moderate Low Impact on Implementation and Operational Costs Impact on Impact on Implementat Operation ion Cost al Costs X High High X Moderate Low X Moderate Low X Low Low Track all consumers/enrollees into and out of plans Individual homepage and account management (system and services) Wellness program functionality (system and services) On-line advertising capabilities (system and services) Outreach Services Electronic content management to store and access electronic documents (notices, receipts, invoices, forms, etc.) X High Moderate Promotion of COHBE to public, Navigators, brokers, etc. X Moderate Moderate Low Low Promotion of wellness programs, enrollment, monitoring, etc. X Web and classroom training for brokers, navigators, Counties X Moderate Moderate Content/resources for consumers, agents, brokers, providers, carriers X Moderate Moderate 27 • Role is to provide guidance to COHBE executive leadership and early input into major strategic decisions such as IT investments, acquisition of services and Acquisition strategy • These initial acquisition decision(s) will likely be in the order of tens of millions of dollars over the first 3 – 5 years • Acquisitions will be structured to be competitive, fair and transparent • Due to the political sensitivities and visibility surrounding the COHBE, it is important that there be no real or apparent conflicts of interest in Acquisitions activities and operational decisions • Meet weekly leading up to the start of the formal acquisition process 28