references - journal of evidence based medicine and healthcare
advertisement

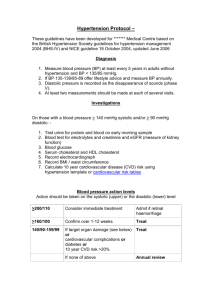
ORIGINAL ARTICLE ANTIHYPERTENSIVE DRUG USE IN DIABETICS: A DRUG UTILIZATION STUDY Limaye R. P1, Ghaisas M. M2, Naik S. A3, Kadam M. S4, Sonavane R. N5 HOW TO CITE THIS ARTICLE: Limaye R. P, Ghaisas M. M, Naik S. A, Kadam M. S, Sonavane R. N. “Antihypertensive Drug use in Diabetics: A Drug Utilization Study”. Journal of Evidence based Medicine and Healthcare; Volume 1, Issue 12, November 24, 2014; Page: 1542-1552. ABSTRACT: INTRODUCTION AND BACKGROUND: Diabetes is a multisystem metabolic disorder complicated by concurrent presence of hypertension. Patients with both disorders have multifold chances of developing complications. Appropriate treatment of hypertension is known to reduce the prevalence of this occurrence. Hence the study was planned to study the antihypertensive drug utilization in diabetics. Such drug utilization studies help in providing evidence for intervention in present therapeutic trends. METHODS: Observational study, carried in consenting patients from Pune and Sangli from September 2013 to January 2014. In a predefined format information regarding use of drugs was recorded. No personally identifiable information was collected. For the purpose of approaching and interviewing the patients, information from tertiary care hospital registers/database was used. Hospitals involved were Bharati Hospital and YCM Hospital. RESULTS: Majority of patients were from age group 61-70 yr. Most prescribed drug was angiotensin II receptor inhibitor, olmesartan (53.33%) in monotherapy and telmisartan in combination with calcium channel blocker viz. amlodipine (60%). Only 6% patients received aspirin while 13% received lipid lowering agents. CONCLUSIONS: Majority of the patients received angiotensin receptor blockers in monotherapy and calcium channel blockers in multidrug therapy. This pattern was not exactly according to the present guidelines but was not irrational. However use of aspirin and lipid lowering agents was very low as compared to expectations and guidelines. KEYWORDS: anti-hypertensive, diabetics, drug utilization. INTRODUCTION: Diabetes is a chronic metabolic disorder which is characterized by high blood sugar level, either because the pancreas does not produce enough insulin, or because cells do not respond to the insulin that is produced. Diabetes and hypertension frequently occur together.1 Hypertension and diabetes are two of the leading risk factors for atherosclerosis and its complications, including heart attacks and strokes1.They share certain physiological traits – that is, the effects caused by each disease tend to make the other disease more likely to occur, some of these effects include: Increased fluid volume –Increased arterial stiffness - Impaired Insulin Handling – Changes in the way the body produces and handles insulin can directly cause increase in blood pressure.1,2,3 Hypertension (defined as a blood pressure ≥140/90 mm Hg) is an extremely common comorbid condition in diabetes, affecting 20–60% of patients with diabetes, depending on obesity, ethnicity, and age.4 In type 2 diabetes, hypertension is often present as part of the metabolic syndrome of insulin resistance also including central obesity and dyslipidemia.4 In type 1 diabetes, hypertension may reflect the onset of diabetic nephropathy. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1542 ORIGINAL ARTICLE Hypertension substantially increases the risk of both macrovascular and microvascular complications, including stroke, coronary artery disease, and peripheral vascular disease, retinopathy, nephropathy, and possibly neuropathy.5,6,7 In recent years, adequate data from well-designed randomized clinical trials have demonstrated the effectiveness of aggressive treatment of hypertension in reducing both types of diabetic complications.4Diabetes increases the risk of coronary events twofold in men and fourfold in women.4 A part of this increase is due to the frequency of associated cardiovascular risk factors such as hypertension, dyslipidemia, and clotting abnormalities.8,9,10 In observational studies people with both diabetes and hypertension have approximately twice the risk of cardiovascular disease as non-diabetic people with hypertension,4 Hypertensive diabetic patients are also at increased risk for diabetes-specific complications including retinopathy and nephropathy. Hence it is essential to monitor the prescribing pattern of antihypertensive drugs in patients suffering from diabetes and hypertension with respect to mono therapy, multi therapy, use of FDC’s etc. to avoid further complications. METHODS: The antihypertensive drug prescribing pattern data was collected, from September 2013 to January 2014, from the patients, whose names were obtained from tertiary care hospitals from Pimpri Chinchwad, Pune, Sangli, (YCM Hospital and Bharati Hospital, respectively), were included in this study according to the inclusion and exclusion criteria. INCLUSION CRITERIA: Patients consenting to participate in the study. Patients having diabetes and hypertension and receiving treatment for it from a physician. EXCLUSION CRITERIA: Patient suffering from any other disease in addition to diabetes and hypertension. STUDY DESIGN: Observational cross sectional. STUDY PERIOD: Five months (No. of patients interviewed were 3475, consent was rejected by 183 patients, excluded patients were 292, included were 3000). STUDY PLACE: Pimpri Chinchwad, Pune & Sangli (Patient interview). SAMPLE DESIGN: Random purposive sampling. The observations were analyzed for descriptive statistics and expressed as %. RESULTS: Age wise distribution of patients Table-1. It was observed that diabetes and hypertension largely occurs in patient of 61-70 years (30.61%). J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1543 ORIGINAL ARTICLE It was observed that angiotensin II receptor blockers (30%) were prescribed mainly by the physician–Table 2. It was observed that combination of (calcium channel blocker + angiotensin II receptor Blocker) 32.25% were mainly prescribed by physician (Table no.3). Fixed Dose Combination use- It was observed that fixed dose combinations of (Calcium channel blockers + angiotensin II receptor blocker) 45.45% were mainly prescribed -(Table 4). It was observed that in only 6% cases aspirin was prescribed. It was observed that in only 13.11% cases lipid lowering drugs were prescribed. DISCUSSION: There are a number of trials demonstrating the superiority of drug therapy versus placebo in reducing outcomes including cardiovascular events and micro vascular complications of retinopathy and progression of nephropathy. These studies used different drug classes, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), diuretics and β-blockers, as the initial step in therapy. All of these agents were superior to placebo; however, it must be noted that many patients required three or more drugs to achieve the specified target levels of blood pressure control. Overall there is strong evidence that pharmacologic therapy of hypertension in patients with diabetes is effective in producing substantial decreases in cardiovascular and micro vascular diseases.1,7,11 The study of patterns of antihypertensive use in patients with diabetes and hypertension was done to evaluate whether they were consistent with evidence-based practice guidelines and to find out what were the prevailing patterns.12,13,14 In monotherapy angiotensin II receptor (AT II) blockers (ARBs) were prescribed maximum. Evidence from several trials and meta-analysis clearly suggested that ACE inhibitors are better than any other class of antihypertensive in protecting against progressive renal damage. According to the analysis in our study in about 18 % cases ACEI’s were prescribed. The rising use of ACE inhibitors may be explained by their substantial benefits in congestive heart failure and diabetes as JNC VI recommends this drug class as the first-line treatment for hypertensive with these conditions. Studies demonstrate the benefits of ACE inhibitors on multiple adverse outcomes in patients with diabetes, including both macrovascular and microvascular complications, in patients with either mild or more severe hypertension and in both type 1 and type 2 diabetes, the established practice of choosing an ACE inhibitor as the firstline agent in most patients with diabetes is reasonable. The use of angiotensin-converting enzyme inhibitors (ACEI) can prevent the progression of renal damage and delay progression to end-stage renal disease in addition to lowering BP. Thus, it has been suggested that all diabetic patients with BP greater than 130/80 mm Hg should begin ACEI treatment unless contraindicated.15,16,17,18,19,20,21 Our study indicated a limited congruency to this principle. In patients with microalbuminuria or clinical nephropathy, both ACE inhibitors and ARBs are considered first-line therapy for the prevention of and progression of nephropathy. However, other strategies including diuretic and β-blocker–based therapy are also supported by evidence.20,22 J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1544 ORIGINAL ARTICLE In our study we cannot conclude whether this principle was followed meticulously or not, as some data regarding nephropathy in many patients was absent or the patient was not evaluated repeatedly. It was also observed that non-selective β blockers were prescribed in some cases (10) in our study. But according to JNC VIII guidelines nonselective β blockers should not be prescribed in diabetic patients as they mask the hypoglycaemic effects in patients.23 Hypertension is a major risk factor for stroke, heart failure, coronary heart disease, and end-stage renal disease. Hypertension is also commonly associated with diabetes and chronic renal failure generally. For management of hypertensive with these comorbidities, both JNC VI and JNC VII guidelines recommend ACE inhibitors as the preferred drug for hypertension in the setting of CKD, diabetes, or congestive heart failure; ACE inhibitors or diuretics for recurrent stroke prevention; and β-blockers for those with prior myocardial infarction. In our study, it is observed that the ACE inhibitors, angiotensin receptor blockers, diuretics along with calcium channel blockers and beta blockers were prescribed but the guideline congruency appeared limited. (We deduce it limited because: only about 40% of patients received the drugs exactly as per guidelines. However in others whether it was prompted by other factors like patient tolerance, adverse effects appearance could not be evaluated due to lack of exact data and history.) Use of multiple drugs in combinations is being increasingly recognized as critical to control hypertension in patients with diabetes. Fixed-dose combination (FDC) therapies offer a means to simplify complex treatment regimens, and have several advantages that help patients reach their glycaemic goals. Recently, several large clinical trials demonstrated that most patients with hypertension can achieve and sustain adequate blood pressure control only with the use of multiple antihypertensive drugs. Initiating drug therapy with a diuretic, either alone or in combination with an agent from another drug class apparently provides the best outcomes for hypertension management as per the JNC VII and JNC VIII guidelines. According to the analysis in our study, combination of calcium channel blockers + AT II blockers was maximum prescribed (as advocated in the JNC VIII guidelines). Also combination of Calcium channel blockers+ diuretics were prescribed (as advocated in the JNC VIII guidelines). As advocated in the guidelines the combination of ACE inhibitors and AT II blockers were not seen to be prescribed. Unacceptable combinations are non-dihydropyridine calcium blockers (such as verapamil or diltiazem) and beta-blockers, dual renin–angiotensin system blockade (e.g. angiotensin converting enzyme inhibitor + angiotensin receptor blocker), renin–angiotensin system blockers and beta-blockers, beta-blockers and centrally acting agents. Combinations of an ACE-inhibitor or angiotensin II–receptor antagonist, a diuretic and an NSAID (including selective COX-2 inhibitors and non-prescribed drugs such as ibuprofen) should be avoided whenever possible due to a high documented risk of acute renal failure. We did find such prescriptions in our study and hence excluded from analysis. Aspirin has been found to be of benefit overall in those at low risk of heart disease as the risk of serious bleeding is equal to the benefit with respect to cardiovascular problems because J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1545 ORIGINAL ARTICLE aspirin has antiplatelet properties. In the present study, it was observed that only in 6% cases aspirin was prescribed. Statins are effective in preventing further cardiovascular disease in people with a history of cardiovascular disease. In the patients without cardiovascular disease but having other risk factors, statins appear to be beneficial with decrease in mortality rate and further heart diseases. Large-scale randomized trials have shown that lipid-lowering with HMG-CoA reductase inhibitors (statins) reduce relative risk for cardiovascular events or death, both in primary and in secondary prevention. The time course over which statins provide prevention against death appears to be long, of the order of one year, which is much longer than the duration of their effect on lipids, a hypothesis put forth by Borghiet.al 2007.24 In the present study only 13.11% cases were prescribed lipid lowering drugs. As per World Health Organization, around 31.7 million individuals in India were affected by diabetes during the year 2000 which may further rise to 79.4 million by the year 2030. Poor management of diabetes and hypertension leads to several complications.25 In developing countries such as India, the focus for long has been on the control of acute and chronic infections and communicable diseases. Mortality data from Global Burden of Diseases Studies has revealed that cardiovascular diseases, especially coronary heart disease are important causes of death. Worldwide, of the 17.5 million deaths from cardiovascular diseases, 20% deaths occurred in high income countries, 8% in upper-middle income countries, 37% in lower-middle income countries and 35% in low income countries including India. In many regions of these countries cardiovascular diseases, especially coronary heart disease, are more prevalent among the illiterate and low socioeconomic subjects. Many of the standard coronary risk factors such as smoking and tobacco use, low physical activity, high dietary fat intake, uncontrolled hypertension, uncontrolled hypercholesterolemia and diabetes are also more.26 In this context, it is important to note the patterns of antihypertensive treatment and follow them for any association with increase in comorbid conditions or mortality if possible. Our study initiates the first part of it and tries to identify areas of concern. If these facts are communicated properly, it may help in bridging the gap between guidelines and actual prescribing. May be appropriate interventions can also be suggested. Exact and meticulous documentation may also be needed to help such studies or such interventions, as we suffered to deduce some inferences because of lack of such information. CONCLUSIONS: In conclusion, findings suggest that angiotensin receptor blockers were prescribed in maximum patients but as per the JNC VIII guidelines the thiazide diuretics should be the first line treatment in hypertension with diabetes. Thus it was observed that the guidelines for treatment were not exactly followed. Anti-hypertensive use in multidrug regimens was generally consistent with JNC VIII guidelines. It was also observed that non-selective β blockers were prescribed in some cases. But according to JNC VIII, non-selective β blockers should not be prescribed in diabetic patients as they mask the hypoglycaemic effects in patients.23 Calcium channel blockers and AT II blockers were the maximum prescribed combinations in FDC as per the guidelines. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1546 ORIGINAL ARTICLE Interpretation of our results must be considered along with recognition of several limitations of the study. First, our study is retrospective and prescribing pattern having a dynamic nature keeps on changing from time to time. Such repeated studies will be needed to comment substantially about trends and its influences. Secondly, for further effectivity, we may require follow up of these patients which are not covered in the study. Third we suffered to deduce inferences on some questions because of lack of appropriate information. REFERENCES: 1. Bernard M.Y., Cheung and Chao Li “Diabetes and Hypertension: Is There a Common Metabolic Pathway?” Published online Jan 27, 2012. 2. Brunton L, Parker K, Blumenthal D, Buxtoraw I, “Therapy of hypertension”. Goodman & Gilman’s Manual of Pharmacology and Therapeutics. 2007, New York: McGraw –Hill pp.544560. 3. Diabetes care “Treatment of diabetes in adults with hypertension “Jan 2002;25(1) supplement 1, d.o.i-10.2337/diacare.25.2007.571, pp 571-573. 4. Diabetes care “Treatment of hypertension in adults with diabetes” American Diabetes association doi-10.2337/diacare 26.2007.580 January 2003 vol 26 no supp 1580-582. 5. Arauz-Pacheco Carlos, Parrott MA, Raskin Philip: “The treatment of hypertension in adult patients with diabetes (Technical Review)”.doi-10.2337/diacare. 25.1.134 Diabetes Care 25: 134–147, 2002. 6. Berlowitz DR, Ash AS, Hickey EC, Glickman M, Friedman R, Kader B “Hypertension management in patients with diabetes: the need for more aggressive therapy”. Diabetes Care. 2003:355–9.J Gen Intern Med. Sep 2005; 20(9): 842–846. doi: 10.1111/j.1525 1497.2005.0170.x PMCID: PMC149021. 7. Sowers JR., Epstein M.“Diabetes Mellitus and Associated Hypertension, Vascular Disease, and Nephropathy: An Update Hypertension. 1995; 26: 869-879 doi: 10.1161/01.HYP.26.6.869. 8. Johnson ML and Singh H. “Patterns of Antihypertensive Therapy Among Patients with Diabetes” Expert Opin Pharmacother. 2007 Oct; 8 (15): 2543-51. 9. McLean DL, Simpson SH, McAlister FA and Tsuyuki RT. “Treatment and blood pressure control in 47,964 people with diabetes and hypertension: A systematic review of observational studies” 2013. 10. Eriksson J, Franssila-Kallunki A, Ekstrand A. “Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus”. N Engl J Med. 1989; 321: 337–343. 11. Monti MC, Lonsdale JT, Montomoli C, Montross R, Schlag E, Greenberg DA "Familial risk factors for microvascular complications and differential male-female risk in a large cohort of American families with type 1 diabetes".(December 2007). J. Clin. Endocrinol. Meta B 92 (12): 4650–5. Doi:10.1210/jc.2007-1185. PMID 17878250. 12. Nilsson PM, Eliasson B and Cederholm J “Hypertension in diabetes: trends in clinical control in repeated large-scale national surveys from Sweden, Journal of Human Hypertension” (2003) doi:10.1038/sj.jhh.1001503 17, 37–44 Current Atherosclerosis Rep Apr 2012; 14 (2): 160–166. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1547 ORIGINAL ARTICLE 13. Qiuping Gu, Ryne Paulose-Ram, Charles Dillon, Vicki Burt, “Antihypertensive Medication Use Among US Adults With Hypertension” Circulation. 2006; 113: 213-221 Published online before print January 3, 2006, doi: 10.1161/ CIRCULATIONAHA.105.542290. 14. W Todd Cade “Diabetes-Related Microvascular and Macrovascular Diseases in the Physical Therapy Setting” Phys Ther. Nov 2008; 88(11): 1322–1335. doi: 10.2522/ptj.20080008 PMCID: PMC2579903 15. Abdi SA, Churi S, and Ravi Kumar Y.S. “Study of drug utilization pattern of antihyperglycemic agents in a South Indian tertiary care teaching hospital” Aug 2006; 22 (10): 855–860. PMCID: PMC2569016 16. Tarikuz Zaman AK, McLean DL, Sobel BE. “The efficacy and tolerability of azilsartan in obese insulin-resistant mice with left ventricular pressure overload.” J Cardiovasc Pharmacol. 2013 Oct; 62 (4): 381-7. doi: 10.1097/FJC.0b013e31829f0c1b. 17. Tarnow L, Groop PH, Hadjadj S, et al "European rational approach for the genetics of diabetic complications—EURAGEDIC: patient populations and strategy". (January 2008) 23 (1): 161–8. Doi: 10.1093/ndt/gfm501. PMID 17704113. 18. Tuomilehto J, Lindstrom J, Eriksson JG “Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance” N Engl J Med. 2001; 344: 1343– 1350. 19. W Todd Cade “Diabetes-Related Microvascular and Macrovascular Diseases in the Physical Therapy Setting” Phys Ther. Nov 2008; 88 (11): 1322–1335. doi: 10.2522/ptj.20080008 PMCID: PMC2579903. 20. Weiss JS, Sumpio BE. "Review of prevalence and outcome of vascular disease in patients with diabetes mellitus". European Journal of Vascular and Endovascular Surgery (February 2006). 31 (2): 143–50. doi:10.1016/j.ejvs.2005.08.015. PMID 16203161. 21. JNC VI https://www.nhlbi.nih.gov/health-pro/guidelines/archive/hypertension-jnc6.htm 22. JNC VII -http://www.nhlbi.nih.gov/files/docs/guidelines/jnc7full.pdf. 23. JNCVIII-http://www.ajmc.com/publications/evidence-based-diabetes. 24. Claudio B, Ada D., Veronesi M, Immordino Y. and Ambrosioni E. “Use of Lipid-Lowering Drugs and Blood Pressure Control in Patients with Arterial Hypertension” Article first published online: 31 MAY 2007 DOI: 10.1111/j.1524-6175.2002.00499.x. 25. Nathan DM, Cleary PA, Backlund JY. "Intensive diabetes treatment and cardiovascular disease in patients with type 1diabetes". The New England Journal of Medicine (December 2005) 353 (25): 2643–53. Doi: 10.1056/NEJMoa052187. PMC 2637991. PMID 16371630. 26. Gupta R, Gupta KD, “Coronary heart disease in low socioeconomic status subjects in India: an evolving epidemic" Indian J Pharmacol. 2012 Mar-Apr; 44 (2): 210–214 doi: 10.4103/ 0253-7613.93850 PMCID: PMC3326914. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1548 ORIGINAL ARTICLE TABLES: It was observed that diabetes and hypertension largely occurs in patient of 61-70 yrs (30.61%) followed by; Age in years < 30 31-40 41-50 51-60 61-70 71-80 81-90 Percentage 2 8.64 17.28 23.45 30.61 14.81 3.70 Table 1: Age wise drug use distribution It was observed that angiotensin II receptor blockers (olmesartan, telmisartan, losartan) (30%) were prescribed mainly by the physician followed by; Category of drug Percentage% Calcium channel blockers Amlodipine 22 ACE Inhibitors 18 (Enalapril, ramipril, lisinopril, levipril) Diuretics 14 (Furesamide, torsemide) β Blockers(Atenolol) 8 + K opener(Nicorandil) 2 Table 2: Category wise drug use distribution It was observed that combination of (calcium channel blocker + angiotensin II receptor [AT II] blocker) 32.25% were mainly prescribed by physician followed by; Category of drug Percentage AT II Blocker +Diuretics 25.80 ACE Inhibitors +Diuretics 9.67 B blocker + Calcium channel blocker 9.67 Calcium channel blocker + ACE Inhibitor 6.45 AT II Blocker +ACE Inhibitors 6.45 Calcium channel blocker+ Diuretics 6.45 B Blocker +AT II Blocker 6.45 Table 3: Combination drug use distribution J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1549 ORIGINAL ARTICLE It was observed that fixed dose combinations of (Calcium channel blockers + angiotensin II receptor blocker) 45.45% were mainly prescribed followed by; Category of drug Percentage (%) β blockers + diuretics 27.27 ACE inhibitors+ diuretics 18.18 AT II blocker + diuretics 9.09 Table 4: FDC drug use distribution Age wise distribution of patients Pattern of drug utilization – mono therapy J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1550 ORIGINAL ARTICLE Pattern of drug utilization – multi therapy Pattern of drug utilization - FDC Use of aspirin It was observed that in only 6% cases aspirin was prescribed. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1551 ORIGINAL ARTICLE Lipid lowering drugs prescribed or not It was observed that in only 13.11% cases lipid lowering drugs were prescribed. AUTHORS: 1. Limaye R. P. 2. Ghaisas M. M. 3. Naik S. A. 4. Kadam M. S. 5. Sonavane R. N. PARTICULARS OF CONTRIBUTORS: 1. Professor, Department of Pharmacology, BVDUMC & H, Sangli. 2. Professor, Department of Pharmacology, SCE’s Indira College of Pharmacy, Pune, Maharashtra, India. 3. Post Graduate Student, Department of Pharmacology, SCE’s Indira College of Pharmacy, Pune, Maharashtra, India. 4. Post Graduate Student, Department of Pharmacology, SCE’s Indira College of Pharmacy, Pune, Maharashtra, India. 5. Post Graduate Student, Department of Pharmacology, SCE’s Indira College of Pharmacy, Pune, Maharashtra, India. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. R. P. Limaye, Department of Pharmacology, Bharati Vidyapeeth DU Medical College & Hospital, Sangli, Maharashtra, India. E-mail: rplimaye@gmail.com Date Date Date Date of of of of Submission: 12/09/2014. Peer Review: 13/09/2014. Acceptance: 07/11/2014. Publishing: 21/11/2014. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/Issue 12/Nov 24, 2014 Page 1552