the gallbladder - Orange Coast College
advertisement

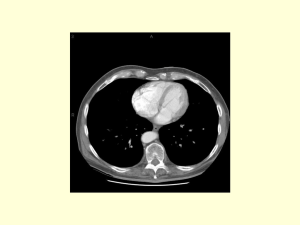
THE GALLBLADDER I. Introduction/General Information A. Location: 1. Epigastric region 2. Right hypochondriac region 3. On inferior surface of liver 4. Between quadrate and right lobes B. Pear-shaped, hollow structure Location of Gallbladder Gallbladder Introduction/General Information, con’t. C. Fundus slants inferiorly, to the right D. Attached to liver by loose (areolar) connective tissue E. Peritoneum covers free surfaces The Gall Bladder and Bile Ducts Fundus Introduction, continued … F. Normal measurements: 7-10 cm long ~ 6 cm diameter 30 – 35 cc volume G. Body and neck directed toward porta hepatis Introduction, continued … H. Neck is continuous with cystic duct I. Cystic duct: 1. joins common hepatic duct 2. superior and posterior to pylorus of stomach The Gallbladder and Biliary System with Pancreas Introduction, continued … J. Common Bile Duct 1. 10-15 cm long 2. Courses through lesser omentum 3. Deep to pyloric sphincter 4. Narrow tube, 1-2 mm diameter 5. Should be no more than 6 mm in diameter CBD, continued … 6. May be 8-10 mm in postcholecystectomy patients 7. Normally has smooth walls 8. Joins with pancreatic duct 9. On L.S., convergence is seen a. anterior to portal vein b. posterior to head of pancreas Introduction, continued … K. Combined duct empties into duodenum @ ampulla of Vater L. Sphincter of Oddi guards duct, regulates bile flow 1. Closed: bile goes into gallbladder 2. Open: bile goes into duodenum Ampulla of Vater with CBD and Pancreatic Duct Ampulla of Vater II. Detailed Anatomy A. Fundus of GB: 1. may be palpated 2. in angle between lateral border of right rectus abdominis and costal margin 3. At level of elbow 4. Most anterior visceral structure Detailed Anatomy, con’t. B. Body of Gallbladder 1. Visceral surface of liver 2. Deep to transverse colon or hepatic flexure of colon 3. Descending portion of duodenum is medial Anatomical Position of the GB IVC Gallbladder Lesser Omentum Common Bile Duct GB in situ, anterior view Detailed anatomy, continued … C. Infections may spread to: 1. duodenum, liver, colon, anterior abdominal wall, peritoneal cavity 2. Direct or via lymphatics 3. Regions on the right half of the abdomen Detailed anatomy, continued … 4. Fistulas may develop: a. abnormal opening between two organs b. with duodenum c. Anastomoses with jejunum Detailed anatomy, continued … E. Neck of gallbladder 1. continuous with cystic duct 2. characterized by a spiral valve (of Heister) 3. makes catheterization difficult GB Anatomy Spiral Valve (of Heister) in Cystic Duct Detailed anatomy, continued … F. Hartmann’s Pouch 1. Infundibulum of gallbladder 2. Lies between body and neck of gallbladder 3. A normal variation 4. May obscure cystic duct 5. If very large, may see cystic duct arising from pouch Hartmann’s Pouch Hartmann’s Pouch of the Gallbladder Cystic Artery Branches Gastroduodenal A. Detailed anatomy, continued … G. Cystic Duct 1. 3-4 cm long 2. Extends from neck of gallbladder to common hepatic duct 3. Joins with common hepatic duct inferior to porta hepatis 4. Spiral valve may extend into neck of gallbladder Cystic Duct Detailed anatomy, continued … H. Epiploic Foramen (of Winslow): 1. an opening deep to lesser omentum 2. leads to lesser peritoneal cavity 3. separates Right portal vein and IVC 4. important clinically Epiploic Foramen Epiploic foramen Lesser peritoneal cavity Midsagittal Section through Abdominopelvic Cavity Detailed anatomy, continued … 5. Surgically, foramen can be used to palpate CBD to check for stones 6. Clinically significant because abscesses may spread via this foramen into lesser peritoneal cavity Detailed anatomy, continued … I. CBD has: 1. hepatic artery on left and portal vein posterior 2. descends in free margin of lesser omentum J. Retroduodenal (2nd) portion of CBD 1. runs parallel to gastroduodenal artery 2. GDA lies to left of CBD Detailed anatomy, continued … K. Last part of CBD 1. passes through pancreas 2. in tube or sulcus closely related to: a. IVC b. Portal Vein c. Gastroduodenal artery Detailed anatomy, continued … 3. On Transverse scans: a. CBD appears as rounded, fluid-filled structure b. anterior and lateral to portal vein Biliary tract, continued … 4. On Longitudinal Scans: 1. the common hepatic duct crosses anterior to right portal vein 2. the CBD courses inferior to head of pancreas Biliary tract, continued … L. Blood supply to gallbladder: 1. Cystic artery a. arises (~ 60% of the time) from right hepatic artery b. passes posterior to hepatic duct, then divides Arterial Supply to the Gallbladder Right hepatic artery Proper hepatic artery Common hepatic artery Cystic artery Blood supply, continued … c. Superficial branch, to peritoneal surface of GB d. Deep branch, to hepatic surface of GB e. May be doubled or tripled Blood supply, continued … Right Hepatic Artery Cystic Artery, Superficial Branch Cystic Artery, Deep Branch Proper Hepatic Artery Common Hepatic Artery Gastroduodenal Artery Blood supply, continued … 2. Small arteries supplying CBD a. arise from cystic artery b. posterior branch of superior pancreaticoduodenal artery 3. May small veins drain directly into the liver Detailed Anatomy, con’t…. M. GB must be distended with bile to be clearly visualized N. Phyrigian Cap 1. Anatomical variation 2. Fund is is folded back on itself 3. not pathological Detailed Anatomy, con’t…. O. Lymphatic drainage of GB 1. Terminate @ celiac nodes 2. Cystic node at neck of GB a. Actually a hepatic node b. Lies at junction of cystic & common hepatic ducts 3. Other lymph vessels also drain into hepatic nodes III. Gallbladder Diseases A. Cholelithiasis & Cholecystitis 1. Cholecystitis = inflammation of GB 2. Cholelithisis = Stone(s) in GB Cholelithiasis GB shows likely sites of stone formation/deposition Gallbladder Diseases, continued … B. Failure to delineate GB 1. Contracted (empty) due to ingestion of food, smoking 2. Secondary to cholecystectomy Gallbladder Diseases, continued … C. Intraluminal defects 1. GB Carcinoma a. US useful in diagnosis b. mass producing thickening and irregularity in wall c. Calculi found frequently Gallbladder Diseases, continued … 2. Polyps of GB a. Intraluminal echogenic projections b. do not change position with patient c. Must be differentiated from septations, mucosal folds 1. septations extend across lumen 2. folds change configuration upon inspiration Gallbladder diseases, continued … 3. Viscid Bile, “sludge” a. Due to intermittent obstruction of CBD or cystic duct b. Seen in patients with bile stasis c. Produces linear, echogenic interface within GB Diseases of the Biliary tract D. Obstructive jaundice: liver patterns a. On T.S., “Parallel channel sign”: 1. presence of two parallel tubular structures near portal vein 2. right portal vein with dilated right hepatic duct anterior Biliary tract, continued … b. On L.S., the “double barrel” or “shotgun” sign is seen 1. not always accurate 2. seeing same vessels as parallel channel sign c. As obstruction progresses, lobulated structures visible