Lab Abnormalities
advertisement

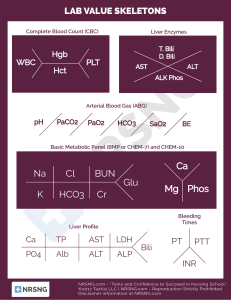
Lab Abnormalities Dan Crouch Kristi Kuhn Kate Lindley Ben Voss Case 1 • You arrive for an afternoon ED shift and send your grateful colleague home. You stop in to evaluate a 24-year-old woman who was signed out to you. She delivered a healthy term infant one month ago. While talking to her, you notice her responses are slow and not very lucid. She complains of vague abdominal pain, nausea, vomiting, and feeling “weak all over”. Vowing revenge on your colleague, who claimed the patient “looked like a million bucks and should never have come in”, you go to a nearby computer and look at her labs. Lab Results – Case 1 11.5 9.3 40 138 106 31 4.0 19 2.4 104 Ca 9.3 PMNs 75% 14.9 1.31 AST 29 ALT 31 38.5 What is most concerning? Discussion – Case 1 DDx Management • TTP (Thrombotic microangiopathy) ▫ Pregnancy/puerperium ▫ Ultra-large von Willebrand factor multimers ▫ ADAMTS13 deficiency (cleaves vWF) due to neutralizing antibodies • DIC ▫ Less likely with normal coags • Peripheral smear • Plasma exchange for TTP • No plts Case 2 • You are seeing a new patient in the Wohl clinic, a quiet 72-year-old African-American male. His son pulls you outside and tells you he thinks his dad is “really depressed”. The patient states that he hasn’t been feeling like himself for the past two months. He feels lethargic, constipated, and has not been eating well. He mentions that he was recently in the ER for back pain and was given some Percocet, which has provided some relief. You are not satisfied with the diagnosis of depression and draw some labs. Lab Results – Case 2 8.1 8.5 350 139 110 45 3.9 28 2.8 92 Ca 10.7 What is most concerning? Protein 8.2 Albumin 2.0 Bili 0.7 AST 15 ALT 11 Alk phos 191 Discussion – Case 2 DDx Management • Malignancy ▫ Multiple Myeloma • Alkylating agents, thalidomide, steroids • Treat hypercalcemia ▫ IVF ▫ Furosemide • SPEP/UPEP, UA • BM Bx • Quantitative Igs • Skeletal survey ▫ Bisphosphnates Case 3 • You are on call for Med 2, and you receive a page from a floor nurse telling you that your next admission, a young lady with an asthma exacerbation, has arrived from the ER and “doesn’t look good”. You put away your chicken fingers and fries and head down the hall to evaluate the patient. Upon entering her room, you notice that she is sitting up on the side of the bed and is audibly wheezing. She tells you in broken sentences that she feels quite short of breath. You place her on supplemental oxygen, call respiratory therapy for a bronchodilator treatment and draw an arterial blood gas. The nurse returns 5 minutes later with the results. Lab Results – Case 3 • • • • • 7.30 / 51 / 190 4 L NC O2 A-a gradient 10 HCO3 20 Anion gap 18 Acid-Base Disorder • Respiratory acidosis • Gap metabolic acidosis (For every pCO2 increase by 10, pH decreases 0.08 and HCO3 increases 1) Discussion – Case 3 Management • BiPAP or intubation. ▫ Pt should be alkalotic. ▫ Acidosis is very ominous, an indication that pt has crossed resp. muscle anaerobic threshold and is generating lactate. • Stay at bedside, watch pt closely. ▫ Earliest sign that BiPAP is working is reduction in RR. ▫ ABG in 30 mins to look for rise in pH, decrease in pCO2. ▫ If not, intubate. Case 4 • You have been slaving away in the ER and are nearing the end of your shift. On the computer tracking system, you see a new patient has just been checked in and is waiting to be seen. She is a 25-year-old female with a complaint of “confusion” per the computer. “How hard can this be?” you say, and head to her room. When you arrive, you see a jaundiced, lethargic woman surrounded by multiple family members. The family states they hadn’t heard from the patient in several days, so they went to her house and found her on the bedroom floor surrounded by empty pill bottles. You start to sweat and order a bundle of labs. The first ones to come back are as follows: Lab Results – Case 4 7.9 13.1 298 141 108 21 4.9 24 1.5 58 Ca 8.9 2.11 41.0 Protein 7.9 Albumin 4.1 Total Bili 6.5 AST 4600 ALT 8450 Alk phos 123 Discussion – Case 4 DDx Management • Ingestion ▫ APAP ▫ Alcohol increases hepatotoxicity of APAP • NG lavage, activated charcoal • Tylenol level check nomogram • Check urine & serum drug screens • NAC (IV given fulminant hepatic failure) • Admit to ICU • Consider liver transplant • Note: dialysis not effective • Pt has many poor prognostic signs (high ALT/AST, high INR, high Bili, renal failure) P4502E-1 half-life prolonged Generates toxic metabolite Case 5 • You are having a quiet day on the rheumatology service, writing your last note on a patient with rheumatoid arthritis who was admitted to the orthopedic service after an injury. “I love the surgery floors,” you say to the surgery chief resident with a smile, “they’re so quiet.” Suddenly, you hear a nurse shouting for help down the hall. You run to her aid and find a little old lady having a generalized tonic-clonic seizure. Her seizure breaks with one dose of Ativan. You quickly review her admission labs. Lab Results – Case 5 9.9 14.6 379 112 82 24 4.3 22 0.9 100 Ca 10.4 UA: specific gravity 1.050 What is most concerning? Protein 7.3 Albumin 3.8 Bili 0.3 AST 24 ALT 13 Alk phos 99 Discussion – Case 5 DDx Management • Hyponatremia ▫ Assess volume status ▫ (Hypovolemic) ▫ Post-operative increase in ADH • IVF: NS until euvolemic • Correct by 0.5 mEq/L/hr • If seizing/symptomatic, correct faster 1-2 mEq/L/hr with hypertonic saline • Na[fluid] – Na[pt]/TBW + 1 ▫ effect of 1 L IVF on Na ▫ TBW = 0.5 x wt (kg) ▫ Then, determine infusion rate needed to correct Na by desired rate. What if pt was in DKA with a glucose of 800? -Corrected Na (1.6 for every 100 over 100) = 123