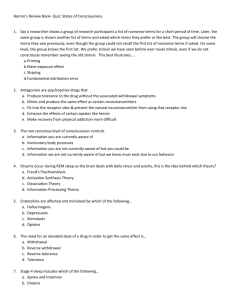
REM Latency (minutes)
advertisement

Understanding the Pathogenesis of Insomnia Dr. Jason Ellis Starting at the end…. Cognitive Behaviour Therapy for Insomnia is: • Longer lasting than pharmacotherapy • More efficacious and is more effective than pharmacotherapy • Cheaper (in the long run) compared to pharmacotherapy • Just as effective with complex cases as with ‘pure’ cases So what’s the problem….? Cognitive Behaviour Therapy for Insomnia is: • Hampered by very few clinicians • Prone to high levels of attrition (50%) and non-adherence • Time and labour intensive for the client Why is Addressing Acute Insomnia Important? • It is the single biggest predictor of chronic insomnia • Acute insomnia is a symptom of many other disorders (e.g. MDD) • 10M prescriptions annually in the UK for sleep medications (£15m) • Persistence of chronic insomnia (mean 2 years) and associated issues • Delivery of preventative intervention would most likely be cheaper than CBT-I • Intervention would most likely be less burdensome on the patient (attrition and non-adherence) How do we Conceptualize Acute Insomnia? Spielman et al (1987) How do we Conceptualize Acute Insomnia? Spielman et al (1987) What is Acute Insomnia? Acute Insomnia Significant Life Event Insomnia Threshold Stress Response Trigger Time Accumulation of Daily Hassles Insomnia Threshold Stress Response Minimum Frequency Duration Time Course 1) Any life event or train of life events which results in a significant reduction in QoL from the individuals Ideal 2) Distress at current situation 3 or more nights per week 3 days -3 months 3 - 14 days Subacute 2 - 4 Weeks Transient 1 - 3 Months Subchronic Chronic Stressor Insomnia Threshold Stress Response Time Qualitative Severity Quantitative Severity Ellis, Gehrman, Espie, Riemann & Perlis (2012) mild / moderate / severe as defined by the patient (+30 Minutes SOL; +30 Minutes WASO) Prevalence of Acute Sleep Disturbance 70.00% 60.00% 50.00% 40.00% USA UK 30.00% N = 2,861 N = 1095 66.85% F Mean Age 32.72 (SD 13.81) 20.00% 10.00% 0.00% Good Sleepers Acute Sleep Disturbance Chronic Sleep Disturbance Unsure USA = 9.47% Acute Sleep Disturbance – Age Category 29-45 UK = 7.85% Acute Sleep Disturbance – Mean Age 31.82 (SD 10.82) Ellis, Perlis et al (under review) Prevalence of Acute Insomnia First-Onset Acute Insomnia 20.00% Episode of Intermittent Acute Insomnia 18.00% First-Onset Acute Sleep Disorders Chronic Insomnia 16.00% Other Chronic Sleep Disorders 14.00% 12.00% 10.00% 8.00% First Onset Acute Insomnia = 2.65% 6.00% Recurrent/ Intermittent Episode = 3.84% 4.00% First Onset Acute Sleep Disorder = 1.37% 2.00% 0.00% First-Onset Acute Insomnia Episode of Intermittent Acute Insomnia First-Onset Acute Sleep Disorders Chronic Insomnia Other Chronic Sleep Disorders Ellis, Perlis et al (under review) Incidence of Acute Insomnia 412 Normal Sleepers from General Population Met all criteria for Acute Insomnia: 1 month assessment (N = 412) – 3.39% - 2.67% First episode (57% F) 3 month assessment (N = 295) – 7.80% - 4.75% First episode (61% F) 75% remission from First-episode cases by 3 months 50% remission from Recurrent cases by 3 months = 33% transition rate from Acute to Chronic Insomnia Ellis, Perlis et al (under review) Question: Are there any differences between normal sleepers and people with acute insomnia in how they sleep? Sample • 54 Participants (36 Females / 18 Males; Mean age 33.6 SD 13.09) • Either no-episode (n = 21 NS) or first-episode insomnia (n = 33 AI) • Acute Insomnia (DSM-V Insomnia Disorder + 3 days – 3 months) • No self-reported chronic illness or psychiatric illness • No gender differences between groups (Chi 2.08, df = 2, p = .35) • No age differences between groups (t(52) = -.3, p = .77) Screening / Measures • 48hour Urinary Melatonin (aMT6s) – circadian abnormalities • Actigraphy (14 days) • Sleep Diaries (14 days) • Polysomnography (2 nights – 1st Night full screen / adaptation night) • Life Events (LES); Stress (PSS); Psychological Adjustment (HADS) Characterising Sleep Continuity in Acute Insomnia Spontaneous Arousals (number per hour of sleep) SL (minutes) Acute Insomnia (n = 33) Normal Sleepers (n = 21) WASO (minutes) SEI (%) 0 20 No significant differences 40 60 80 100 Characterising Sleep Architecture in Acute Insomnia Latency REM Latency N3 Acute Insomnia (n = 33) Normal Sleepers (n = 21) Latency N2 Latency N1 0 20 No significant differences 40 60 80 100 Characterising Sleep Architecture in Acute Insomnia % REM % N3 Acute Insomnia (n = 33) % N2 Normal Sleepers (n = 21) % N1 % WAKE 0 20 40 % N2 (t(52) = 2.22, p<.05) % N3 Significant (t(52) = -2.94, p<.005) 60 Architectural Differences Between Sleeper Groups REM Latency (minutes) 120 * p<.05 * p<.05 100 F(2,51) = 4.75, p<.01 80 60 REM Latency… 40 20 0 Normal Sleeper (n = 21) Acute to Remission (n = 19) Acute to Chronic (n = 14) Architectural Differences Between Sleeper Groups Percentage Slow Wave Sleep 20 * p<.05 18 16 F(2,51) = 5.68, p<.001 14 12 10 Percentage Slow… 8 6 4 2 0 Normal Sleeper (n = 21) Acute to Remission (n = 19) Acute to Chronic (n = 14) Is this a ‘level of stress’ response issue? Life Event Scale Scores Perceived Stress Scale Scores 46 250 * p<.05 * p<.05 45 * p<.05 * p<.05 44 200 43 42 150 41 Perceived Stress Scores Life Events… 40 100 39 38 50 37 36 0 Normal Sleeper (n = 21) Acute to Acute to Remission Chronic (n = 19) (n = 14) Normal Sleeper (n = 21) Acute to Acute to Remission Chronic (n = 19) (n = 14) Is this a ‘sleep propensity’ issue? Is this a ‘sleep propensity’ issue? Time in Bed % Time in Bed (Day) Time in Bed (Diary) Minutes 60 540 530 50 520 40 510 30 % Time in Bed Time in Bed 500 20 490 10 480 0 470 Normal Acute to Sleeper (n = Remission 21) (n = 19) Acute to Chronic (n = 14) Normal Sleeper (n = 21) Acute to Remission (n = 19) Acute to Chronic (n = 14) What is this pattern also seen in? % Slow Wave Sleep REM Latency (minutes) 20 120 * p<.05 * p<.05 * p<.05 18 100 16 14 80 12 10 60 REM… 40 Percentage Slow Wave… 8 6 4 20 2 0 0 Normal Sleeper (n = 21) Acute to Remission (n = 19) Acute to Chronic (n = 14) Normal Sleeper (n = 21) Acute to Acute to Remission Chronic (n (n = 19) = 14) Psychological Adjustment 12 * p<.05 10 * p<.05 8 6 Depression Scores Anxiety Scores 4 2 0 Normal Sleeper (n = 21) Acute to Remission (n = 19) Acute to Chronic (n = 14) New Approaches to Address Attrition in CBT-I? Combining CBT-I with a stimulant Decrease Slow Wave Sleep Combining CBT-I with a hypnotic Question: Are there any relevant daytime factors which relate to this poor psychological adjustment in acute insomnia? Sleep Preoccupation A tendency to be overly preoccupied about sleep during the day, with catastrophic interpretations and counterproductive actions across the 24h cycle. Affective = + worry about short and long-term consequences / anxious at night Behavioural = + drink more coffee / go to bed earlier Cognitive = + concentration difficulties / memory deficiencies Are People With Insomnia Preoccupied with their sleep? 722 participants completed the Sleep Preoccupation Scale • Poor sleeper (“a current sleep disruption which is negatively affecting the quality, quantity, or timing of your sleep and/or having sleep which is unrefreshing, and occurs at least three nights per week”) • Average sleeper (“a current sleep pattern which is sometimes disrupted and/or unrefreshing but occurs less than three nights a week”) • Good sleeper (“a current sleep pattern which is not disrupted in its quality, quantity, and timing, and is refreshing”) Ellis et al (2007) Levels of Daytime Sleep Preoccupation Good Sleepers Preoccupation Average Sleepers Poor Sleepers 0 10 20 30 40 50 60 Aim to examine the relationship between the Sleep Preoccupation Scale (SPS) and sleep parameters over the course of a semi-natural stressor. The sample was four classes of student nurses and midwives from a West London Teaching Hospital. Students filled in the SPS and a sleep diary every day over the course of their two week exam period (one week before, over the two days of exams as well as three days afterward). All scores are averaged across number of nights. Of the initial sample of 103 students, 92 agreed to take part and returned the questionnaires. Mean age 29.4 (SD 8.3) 80 (86.7%) females, 12 (13.3%) males. BASELINE EXAM RECOVERY SPS 40.57 (17.1) 58.67 (21.35) 45.97 (24.98) SEI 71.28 (14.68) 59.39 (18.87) 64.18 (15.64) 0.2 (n.s) -0.4 (p<0.05) 0.18 (n.s) Correlation Coefficient BASELINE EXAM RECOVERY SPS 40.57 (17.1) 58.67 (21.35) 45.97 (24.98) SEI 71.28 (14.68) 59.39 (18.87) 64.18 (15.64) 0.2 (n.s) -0.4 (p<0.05) 0.18 (n.s) Correlation Coefficient Levels of Daytime Sleep Preoccupation Good Sleepers Average Sleepers Preoccupation Poor Sleepers Exam Stress Baseline 0 10 20 30 40 50 60 Conclusions Acute Insomnia is: Highly prevalent (7.9%) Annual incidence (31.2%) Increased Stage 2 Sleep Decreased SWS Increased Daytime Preoccupation The transition to Chronic Insomnia is: and associated with: Highly likely (25-50%) Increased REM Latency Decreased SWS Increased Anxiety and Depression and which looks very similar to: The onset of an Affective Disorder How early is early prevention? 1020 * p<.05 1000 Milliseconds (Standard Error) 980 960 940 Control Group (N = 51) Children of Parents with Insomnia (N = 38) 920 900 880 860 Neutral Words Sleep-Related Words Ellis, Thomson, Gregory & Sterr (2012) University of Surrey University of Everywhere Else in the World Professor Annette Sterr Dr. Michael Perlis (U Penn) Professor Celyne Bastien (U Laval) Dr. Phil Gehrman (U Penn) Professor Dieter Riemann (U Freiberg) University of London Dr. Alice Gregory And the people who fund this work University of Glasgow Professor Colin Espie Dr. Maria Gardani Dr. Amy Thomson jason.ellis@northumbria.ac.uk