Ventilation for the Surgical Resident
advertisement

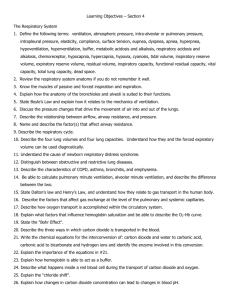
OBJECTIVES Respiratory physiology oxygen delivery abnormalities of gas exchange review of lung volumes chest wall and respiratory mechanics Mechanical Ventilation indications nomenclature ventilation modes: invasive and non-invasive special circumstances: ARDS, refractory hypoxemia and BPF complications: High pressures, VILI, Auto-PEEP, VAP weaning RESPIRATORY PHYSIOLOGY REVIEW OXYGEN DELIVERY oxygen is carried in the blood in two forms: bound to Hb (SpO2) * dissolved in plasma (PaO2) oxygen content (CaO2) is the sum of both: [Hb] x SpO2 x (1.36) + (PaO2) x (0.003) oxygen delivery is a product of both the arterial O2 content and cardiac output harder to unload O2 easier to unload O2 OXYGENATION Hypoxia is a state of tissue oxygen deprivation anaerobic metabolism lactic acidosis can lead to cellular, tissue and organ death Hypoxia can result from: low PaO2 anemia or abnormal Hb low cardiac output states/ impaired perfusion inability to utilize O2 (eg. cyanide) Hypoxemia refers to low PaO2 in the blood ABNORMAL GAS EXCHANGE Efficiency of gas exchange: the a-a gradient P(A-a)O2 = PAO2 – PaO2 PAO2 = [713 x FiO2] – [1.25 x PaCO2] cumbersome, normal values not known for supplemental O2 Often use P/F ratio instead: PaO2/FiO2 normal on FiO2 0.21 is 450-500 range tells us nothing about alveolar ventilation (PCO2) will be dependent on level of PEEP/ CPAP ABNORMAL GAS EXCHANGE Physiologic Mechanism of Hypoxia Description Low PiO2 altitude, disconnection of tubing Hypoventilation displaces O2 from alveolus masked by supplemental O2 V/Q mismatch inappropriately low ventilation for degree of perfusion; usu responds to O2 Shunt alveoli that are perfused are not ventilated with true shunt, minimal effect of O2 healthy alveoli can’t compensate for sick ones Low mv PaO2 low CO or high consumption; can decrease PaO2 in presence of large shunt Diffusion abnormality theoretic abnormality, not clinically relevant INTRAPULMONARY SHUNT VENTILATION Ventilation refers to CO2 clearance Alveolar ventilation air that meets perfused alveoli and participates in gas exchange Dead space ventilation air doesn’t contact perfused alveoli to participate in gas exchange anatomic+ alveolar + equipment “wasted” ventilation Minute Ventilation (MV) RR x VT total gas (L/min) of ventilation normal 6-8 L/min ABNORMAL GAS EXCHANGE HYPERCAPNIA Mechanisms: • rarely causes hypercapnia in absence of other ventilatory defect Increased CO2 production malignant hyperthermia thyroid storm Decreased CO2 clearance low minute ventilation (RR x VT) high dead space ventilation • low respiratory drive • CNS depression • drugs • OHS/ CSA • respiratory mechanical failure • fatigue • neuromuscular disease • chest wall abnormality • underlying lung pathology • COPD • ILD • pulmonary embolism • pulmonary vascular disease LUNG VOLUMES TLC: amount of gas in lungs after maximal inspiration RV: amount of gas in lungs after maximal expiration VC: volume of gas expired going from TLC to RV FRC: volume of gas in lungs at the resting state (endexpiration) TV: amount of gas inhaled in a normal inspiration PULMONARY COMPLIANCE Defined as the ability of the lung to stretch (change in volume) relative to an applied pressure Factors affecting compliance: lung volume (overdistention vs. atelectasis) interstitial pathology (CHF, ILD) alveolar pathology (pneumonia, CHF, blood) pleural pathology (pleural effusion, fibrosis) chest wall mechanics diaphragm mobility chest wall deformities abdominal pressures RESPIRATORY FAILURE RESPIRATORY FAILURE Acute respiratory failure: “any impairment of O2 uptake or CO2 elimination or both that is severe enough to be a threat to life” The signs and symptoms of respiratory failure are nonspecific and often nonrespiratory reflect end-organ dysfunction of neurologic and cardiovascular systems RESPIRATORY FAILURE HYPOXEMIC HYPERCAPNIC Won’t breathe Can’t breathe RESPIRATORY FAILURE Clinical signs and Symptoms hypoxia is relatively easily identified on clinical examination hypercapnia can be more subtle in its presentation may not be in respiratory distress (central failure) General • tachypnea • dyspnea • diaphoresis • central cyanosis (late) Respiratory • wheeze • dyspnea • cough • accessory muscle use •abdominal paradox Cardiovascular • tachycardia • dysrhythmias • hypertension • hypotension Neurologic • restlessness • headache • confusion • delirium • tremor • asterixis • seizures • coma MECHANICAL VENTILATION MV: INDICATIONS Hypoventilation arterial pH more important than absolute pCO2 can result from central or mechanical failure respiratory acidosis with pH <7.25 and pCO2 >50 Hypoxemia hypoxemia refractory to conservative measures pO2 < 60 with FiO2 >60% Respiratory Fatigue excessive work of breathing suggestive of impending respiratory failure Airway Protection MV: INDICATIONS “the patient looked like they need to be placed on a ventilator” most absolute criteria for initiation of mechanical ventilation are arbitrary and reflect a line drawn in the sand fail to account for a spectrum of disease a PaO2 of 61 is acceptable and 59 is not? chronic vs acute derangements fail to account for co-morbid disease management precise control of PaCO2 in a patient with a head injury assisted hyperventilation to compensate for a metabolic acidosis airway maintenance with nasal airway or surgical airway NOMENCLATURE A “mode” is a pattern of breaths delivered by the ventilator pressure support pressure control volume control To understand the differences, must understand the “phases” of ventilation expiratory: passive phase, PEEP applied triggering: change from expiration to inspiration inspiratory: assisted inspiratory flow cycling: end of inspiration and change to expiration PHASES OF VENTILATION A. Triggering: patient triggered (flow, pressure) machine triggered (time) B. Inspiration-assisted INSP time (PCV) volume (VCV) flow (PSV) D. Expiration- passive EXP C. Cycling VOLUME CONTROL (VCV) Set tidal volume, cycles into exhalation when target volume has been reached; airway pressure dependent on lung compliance guarantees a minimum minute ventilation (MV= RR x Vt) useful for patients with a decreased respiratory drive post-operative, head-injured, narcotic overdose Variables: Trigger: patient or machine controlled Inspiratory phase: set inspiratory flow rate Cycling: SET Expiratory phase: set amount of PEEP Alarms: high pressure (default into PCV and cycle), high RR PRESSURE CONTROL (PCV) Inspiratory pressure and inspiratory time are set; tidal volume is dependent on lung compliance allows for control of peak airway pressures (ARDS) a longer inspiratory time can allow for better recruitment and oxygenation Variables: Trigger: patient or machine controlled Inspiratory phase: SET- target pressure, generated quickly and maintained throughout; high initial flow rate Cycling: time Expiratory phase: set amount of PEEP Alarms: high and low tidal volumes, high RR PRESSURE SUPPORT (PSV) Spontaneous mode of ventilation; patient generates each breath and a set amount of pressure is delivered with each breath to ‘support’ the breath comfortable: determine own RR, inspiratory flow and time Vt depends on level of pressure support set, lung compliance and patient effort Variables: Trigger: patient controlled; must initiate breath Inspiratory phase: SET support pressure Cycling: flow cycled (when falls to ~25% of peak) Expiratory phase: set amount of PEEP Alarms: apnea and high RR NOMENCLATURE CMV (Controlled Mechanical Ventilation) minute ventilation entirely determined by set RR and Vt patient efforts do not contribute to minute ventilation AC (Assist/Control) combination of mandatory (set rate) and patient triggered breaths patient triggered breaths deliver same Vt or pressure as mandatory breaths SIMV (Synchronized Intermittent Mandatory Ventilation) combination of mandatory and patient-triggered breaths pure SIMV, patient not assisted on additional breaths can combine SIMV with PSV, so additional breaths are supported NOMENCLATURE Comparison of respiratory pattern using different modes: PEEP Positive End-Expiratory Pressure (PEEP) constant baseline pressure delivered throughout cycle by convention: called CPAP if breathing spontaneously and PEEP if receiving positive pressure ventilation 3-5cm H20 PEEP provided to all intubated patients to overcome the decrease in FRC caused by bypass of glottis Advantages: Improve oxygenation by preventing end-expiratory collapse of alveoli and help recruit new alveoli may prevent barotrauma caused by repetitive opening and closing of alveoli creates hydrostatic forces to fluid from alveoli into interstitium PEEP- COMPLICATIONS Potential complications: may overdistend alveoli: causing barotrauma can worsen oxygenation by increasing dead space decreases venous return (high intrathoracic pressures) decreasing cardiac output increases RV afterload can contribute to RV strain and/or failure associated with severe respiratory failure lung heterogeneous some areas may be getting too much, while others not enough PEEP- CONTRAINDICATIONS Relative contraindications to high PEEP circumstances where risk may outweigh benefit: RELATIVE CONTRAINDIATIONS MECHANISM OF HARM Hypotension Decreased venous return Right Heart Failure High RV afterload worsened RV failure Right to Left Intracardiac Shunts High RV afterload worsened shunt Increased ICP Can increase CVP, decreasing cerebral venous drainage and further increasing ICP Hyperinflation Worsening gas trapping Asymmetric or Focal lung disease High pressure preferrentially directed to normal lung Bronchopleural Fistula Increased air leak prevent healing NON-INVASIVE VENTILATION The delivery of PPV without an ETT avoids complications of intubation, including VAP Two fundamental types: CPAP and bi-level or BiPAP CPAP delivers continuous positive pressure throughout respiratory cycle useful for hypoxemic respiratory failure BiPAP delivers ‘pressure support’ during inspiration (IPAP), coupled with PEEP during expiration (EPAP) useful for hypercapneic or combined respiratory failure NIV: INDICATIONS Has been shown to decrease need for intubation and decrease morbidity & mortality in certain patients: Acute cardiogenic pulmonary edema (ACPE) COPD exacerbation May decrease re-intubation rate after extubation in COPD Fundamental requirements: spontaneously breathing patient who can protect airway potentially reversible condition ability to improve within a few hours cooperative patient no hemodynamic instability, no cardiac ischemia NIV: CONTRAINDICATIONS Hemodynamic instability or shock Decreased LOC and inability to protect airway Inadequate respiratory drive High risk of aspiration (SBO, UGI bleed) Facial trauma or craniofacial abnormality Upper airway obstruction Uncooperative patient Inability to clear secretions or excessive secretions NIV: MONITORING NIV has been successful if the patient’s work of breathing has decreased and blood gas abnormalities are starting to resolve Clinical improvement is usually evident within the 1st hour Biochemical improvement usually evident within 2-4 hours of initiation If ongoing evidence of respiratory failure despite NIV within a few hours of initiation… CONSIDER INTUBATION SPECIAL CIRCUMSTANCES ARDS Definition: bilateral pulmonary infiltrates absence of LA hypertension severe hypoxemia (PaO2/FiO2 ratio <200) Heterogeneous lung involvement dependent: atelectatic, consolidated non-dependent: relatively preserved Concept of the “baby lung” high inflation pressures/ volumes used for hypoxemia can damage normal lung (volutrauma, barotrauma) repetitive opening/closing of marginal areas causes additional trauma (atelectrauma) ARDS: VENTILATION Important to understand principles of ARDS to minimize ventilator-induced lung injury Lung protective ventilation (ARDSnet) compared tidal volume of 12ml/kg (840) and plateau <50 cm H2O vs 6ml/kg (420) and plateau <30 cm H2O stopped early for benefit mortality 31 vs 39% (p=0.007) more vent free days Mild permissive hypercapneia ok May require sedation to maintain REFRACTORY HYPOXIA Some additional modes of ventilation can be tried for hypoxia refractory to conventional ventilation: recruitment maneuvers inverse ratio ventilation (I>E) prone ventilation airway pressure release ventilation (APRV) high frequency oscillation ventilation (HFOV) None to date have shown an increased mortality, but can improve oxygenation APR VENTILATION APRV ventilates by time-cycled switching between two pressure levels (Phigh and Plow) degree of ventilator support is determined by the duration of the two pressure levels and the tidal volume delivered tidal volume determined by Δ P and respiratory compliance permits spontaneous breathing in any phase better ventilation of posterior, dependent lung regions after 24h improves recruitment lower sedation required C/I if deep sedation needed, COPD? HFO VENTILATION HFOV achieves gas transport by rapidly oscillating a small Vt (~anatomic dead space) achieving rapid gas mixing in the lung gas transport occurs along partial-pressure gradients oscillates around a constant high mean airway pressure (mPaw) to maintain alveolar recruitment, avoiding big Δ P risk of barotrauma and hemodynamic compromise limilar to conventional ventilation O2: mPaw and FiO2 CO2: frequency and ΔP BRONCHOPLEURAL FISTULA Presence of a persistent air-leak >24h after insertion of a CT is highly suggestive of a bronchopleural fistula after exclusion of an external leak Weaning from PPV entirely is optimal When not possible, select strategy to minimize minute ventilation and intrathoracic pressure BPF- MANAGEMENT Wean ventilatory support as much as tolerates PSV may be preferable to full ventilation limit mean airway pressure and number of high pressure breaths avoid alkalosis; consider permissive hypercapnia minimize PEEP (intrinsic and extrinsic); treat bronchospasm Limit VT to 6-8 ml/kg Minimize inspiratory time (keep I:E ratio low, use high flows) Use lowest CT suction that maintains lung inflation Explore positional differences that minimize leak BPF- MANAGEMENT Consider specific or unconventional measures for physiologically significant leaks: independent lung ventilation endobronchial approach to sealing leak surgical closure Treat underlying cause of respiratory failure BPF in ARDS Usually a measure of severity of underlying disease will --often doesn’t improve until ARDS improves BPF nearly always improves without specific therapy BPF usually not physiologically significant (<10%), even in presence of hypercapnia Reducing the size of the leak has minimal effect on gas exchange No specific measures have been shown to affect outcome Patients almost never die of BPF… they die with BPF COMPLICATIONS OF VENTILATION HIGH AIRWAY PRESSURES Decreased Compliance pneumothorax mainstem intubation dynamic hyperinflation CHF ARDS consolidation pneumonectomy pleural effusion abdominal distention chest wall deformity Increased Resistance bronchospasm secretions small ETT mucosal edema biting ETT VILI VENTILATOR-INDUCED LUNG INJURY multiple recognized forms: barotrauma: high ventilation pressures result in global or regional overdistention can result in alveolar rupture may be gross (PTX, BPF, subcut emphysema) or microscopic volutrauma/atelectrauma: ventilation at low lung volumes causes repetitive opening and closing of alveoli may lead to shear stress, disruption of surfactant and epithelium biotrauma: mechanical stretch or shear injury lead to inflammatory mediator release and cellular activation VILI Prevention: low VT ventilatory strategies minimize peak and plateau pressures PEEP for recruitment and minimize end-expiratory collapse tolerate mild to moderate permissive hypercapnia to achieve above goals: allowing PCO2 to rise into high 40’s to 50’s to reduce driving and plateau pressures generally considered safe at low levels contraindications: increased ICP, acute or chronic cardiac ischemia, severe PH, RV failure, uncorrected severe metabolic acidosis, TCA overdose, pregnancy AUTO-PEEP aka: intrinsic PEEP or dynamic hyperinflation Seen when a patient has failed to expire full VT and subsequent breaths delivered result in increasing hyperinflation AUTO-PEEP Making the diagnosis: inspection: continuous inward movement of chest until start of next breath auscultation: persistence of breath sounds until start of next ventilator breath failure to return to baseline on waveform before delivery of next breath “Auto-PEEP” “normal” AUTO-PEEP COMPLICATIONS OF AUTO-PEEP Hypotension from increased intrathoracic pressure with decreased venous return Decreased efficiency of diaphragm and force generated May be unable to generate sufficient pressure to trigger breaths Increased work of breathing, and respiratory muscle fatigue Increased agitation, ventilator asynchrony AUTO-PEEP: MANAGEMENT Lengthen time for exhalation slow controlled rate on ventilator lengthen I:E ratio (shorten I time) may require patient sedation if patient-driven Treat bronchospasm bronchodilators corticosteroids if asthma or AECOPD Match intrinsic PEEP to minimize gas trapping by dynamic collapse VAP Nosocomial infection of lung that develops >48h after ETT 9-27% of mechanically ventilated patients 2nd most common nosocomial infection (UTI 1st) Risk of VAP highest early in course, but incidence increases with duration of mechanical ventilation 3%/day (1-5), 2%/day (5-10), 1%/day (>10) overall mortality 27% microbiology: 60% GNB: E coli, P aeruginosa, Klebsiella or Acinetobacter sp. GPC incidence is increasing (esp common in TBI, DM) 20-40% are polymicrobial VAP Mechanism: Aspiration of oropharyngeal pathogens or leakage of secretions around ETT primary routes into LRT Infected biofilm on ETT with embolization during suctioning Risk factors: mechanical ventilation COPD longer duration of MV age >60 ARDS re-intubation male sinusitis supine position trauma aspiration paralytics NG tube low ETT cuff pressure post-surgical patient VAP DIAGNOSIS: suspect if MV >48h -and fever WBC purulent sputum new or progressive infiltrate on CXR increased O2 requirements Problem: • no gold standard • broad DDx • significant overlap with infectious tracheobronchitis • colonization ≠ infection Prevention: VAP bundle: HOB >30°, sedation vacations, DVT prophylaxis, stress ulcer prophylaxis oral decontamination with antiseptic handwashing WEANING WEANING Weaning refers to gradual withdrawal of ventilatory support Most patients (~75%) do not require ‘weaning’ and rather require liberation from mechanical ventilation if no respiratory muscle weakness or abnormal lung mechanics have developed during illness Initial task is to determine if the initial reason for intubation and mechanical ventilation have resolved pneumonia or other pulmonary process treated and improving oxygenation, RR, VT, minute ventilation, RSBI (f/VT) adequate hemodynamically stable level of consciousness improved or airway protection resolved WEANING Next is to determine if the patient can breathe without the ventilator Spontaneous Breathing Trial (SBT) most common method must be HD stable, no cardiac ischemia, oxygenation should be adequate and PaO2/FiO2 ratio >120 at PEEP ~5 sedatives and narcotics should be discontinued in advance 30 m- 2h trial of reduced support: t-piece, PSV (<8/5) on FiO2 0.5 if RR <35, ΔHR <20 bpm, ΔBP <20mmHg, ABG w/o acidosis -and cough PF >60L/min, ETT suction <q2h and cuff leak consider trial of extubation WEANING If fails SBT, attempt to identify contributing treatable factors: hypoxemia- consider diuresis and afterload reduction excessive secretions- treat infections bronchospasm- bronchodilation, steroids hypercapnia- less sedation, treat cause if identified if suspect strength-load imbalance, may need ‘weaning’ Many ‘weaning’ strategies have been tried for patients that fail their 1st SBT: once daily t-piece trial >/≈ PSV > SIMV (most patients ≤ 5d) does not account for patients with respiratory muscle weakness or underlying weaning ‘failure’ QUESTIONS?