Pulmonary Considerations in Neurological Care Patients
advertisement

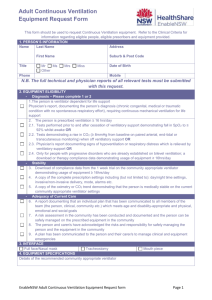
Pulmonary Physiology, Oxygen Delivery, and Mechanical Ventilation James Barnett, RN, MSN Clinical Educator – Neuroscience PCC Vanderbilt University Medical Center May 2007 Physiology Review Pulmonary Perfusion Recruitment—this mechanism decreases pulmonary vascular resistance (PVR) to accommodate increased blood flow Capillary dilation—this mechanism directly increases capillary size via stimulation of the autonomic nervous system Lung Compliance Compliance A term used to describe resistance in relation to elasticity Low Compliance Lungs become stiffer and less elastic Stiff lungs (ARDS, pulmonary edema, fibrosis, pneumonia, atelectasis High Compliance More easily distended Physiology of Gas Exchange (Respiration) Respiration: The interchange of gases between an organism and the environment in which it lives 3 Step Process 1. Ventilation 2. Diffusion 3. Transport Physiology Review Ventilation …movement of air between the body and the environment…and distribution of air within the tracheobronchial tree to the alveoli effected by: respiratory pressures, surface tension (surfactant), and lung compliance Physiology Review Alveolar Diffusion …gas exchange across the alveolar-capillary membrane from the air sac (higher concentration) into the pulmonary blood supply (lower concentration) …CO2 is 20 times more diffusable than O2 across the alveolar-capillary membrane …effected by five variables Physiology Review Five variables determine alveolar diffusion 1. Surface Area 2. Membrane Thickness 3. Amount of Hemoglobin 4. Partial Pressures 5. Diffusion Coefficients Pathologic Alterations V/Q Mismatching Normal pulmonary function V=Q Physiologic shunting V<Q Atelectasis or pneumonia Remember: V = Ventilation and Q = Perfusion Pathologic Alterations V/Q Mismatching Alveolar dead space V>Q Pulmonary emboli Silent units No V nor Q ARDS secondary to Pulmonary Embolus Total Lung Ventilation The Sum of: Deadspace ventilation Deadspace Ventilation + Alveolar Ventilation Volume of inspired air that does not participate in gas exchange (upper airways, trachea, ET tubing) Total Lung Ventilation Alveolar Ventilation That portion of total ventilation that takes part in gas exchange Best indicator is PaCO2 Normal – adequate alveolar ventilation High – alveolar ventilation is low and hypoventilation is present Low – alveolar ventilation is high and hyperventilation is present Description of Ventilatory Failure Clinical state produced when PaCO2 rises quickly enough to produce an immediate, lifethreatening situation PaCO2 > 50 mmHg Signs and Symptoms of Acute Hypoxia Tachycardia Tachypnea Dyspnea Euphoria Stupor Tremors Hyperreactive reflexes Anxiety Arrhythmias Decreased PaO2 HTN Impaired judgment Blurred Vision Coma/Death Clinical Conditions With Increased Risk of Hypoxia Myocardial infarction Acute pulmonary disorders Sepsis Drug overdose Liver failure Head trauma CHF Hypovolemic shock Blunt chest trauma Acute neuromuscular disease Acute abdomen (splinting) Acute pancreatitis Spinal cord injury Indications for Oxygen Therapy Tachypnea Cyanosis Restlessness Disorientation Cardiac arrhythmias Slow bounding pulse Tachycardia Hypertension Dyspnea Coma Labored breathing (use of accessory muscles, nasal flaring) Lethargy Tremors/seizure activity Methods of Oxygen Delivery Most common methods of oxygen delivery include Nasal Cannula Venturi Mask 100% Non-Rebreather Mask Mechanical Ventilation Oxygen Delivery Methods Nasal Cannula Comfortable, convenient, mouth breathing will not effect % of O2 delivered Liters/min = % 2 l/m = 24-28% 3 l/m = 28-30% 4 l/m = 32-36% 5 l/m = 36-40% 6 l/m = 40-44% Cannot administer > 6 liters/minute (44%) Nursing Care Clean equipment daily Evaluate for pressure sores over ears and cheeks Lubricate prongs before inserting into nares Liter flow > 6 L/min will not increase FiO2 Oxygen Delivery Methods Venturi Masks FiO2 Delivery (55688) Blue 24% Yellow 28% White 31% Green 35% Pink 40% Nursing Care Concerns Tight seal is a must Interferes with eating/drinking Condensation collection Monitor ABG’s Check for leaks in system Do NOT operate at <5 L/min (will not flush out accumulated CO2) Clean equipment several times daily Oxygen Delivery Methods 100% Non-Rebreather Delivery percentages 6 l/min = 55 – 60 % 8 l/min = 60 – 80 % 10 l/min = 80 – 90 % >12 l/min = 90 + % Concern Nursing Care Benefit: Has a one way expiratory valve that prevents rebreathing expired gases May lead to O2 toxicity Monitor ABG’s Check for leaks See Venturi mask care Oxygen Delivery Methods Mechanical Ventilation Allows administration of 100% oxygen Controls breathing pattern for patients who are unable to maintain adequate ventilation Is a temporary support that “buys time” for correcting the primary pathologic process Indications for Mechanical Ventilation Mechanical Failure Ventilatory Failure Oxygenation Failure General Anesthesia Post-Cardiac Arrest Mechanical Ventilation Two categories of ventilators Negative pressure ventilators Iron lung Cuirass ventilator Positive pressure ventilators Two categories Volume-cycled (volumepreset) Pressure-cycled (pressurepreset) Iron Lung Positive Pressure Ventilators Volume-cycled terminate inspiration after delivering a preset volume of gas delivered regardless of required pressure to do so volume remains the same unless high peak pressures reached Pressure-cycled terminate inspiration when a preset pressure is reached varying degrees of resistance will interfere with gas flow best used with drug overdose patients not good for postoperative or severe respiratory infections Modes of Ventilation Volume preset modes Volume variable modes Control mode ventilation (CMV) Assist - Control mode ventilation (A/C) Intermittent mandatory ventilation (IMV/SIMV) Pressure support ventilation (PSV) Pressure controlled ventilation (PCV) Pressure regulated volume control ventilation (PRVC) Positive Airway Pressure Positive End Expiratory Pressure (PEEP) Continuous positive airway pressure (CPAP) Controlled Mandatory Ventilation Allows total control of the patient’s rate and tidal volume Used for patient’s needing short term ventilation When no inspiratory effort is desired Multiply injured patients without spontaneous ventilatory effort Neurologic injury Drug overdose Assist – Control Ventilation Allows patient to “initiate” inspiration and control “frequency” Patient initiated breaths are delivered at preset tidal volumes Can allow an inappropriately high minute ventilation and increase work of breathing Mechanical Ventilation IMV Patient receives a baseline minute volume Breathes spontaneously at a fast or slow rate Variable tidal volume Mechanical Ventilation SIMV Provides the additional advantage that the IMV mandatory breaths are triggered when the ventilator senses inspiratory effort by the patient Generally well tolerated Diminished risk of barotrauma (less stacking) Mechanical Ventilation SIMV Key Advantages of IMV/SIMV Patient’s respiratory efforts are utilized Weaning begins at the outset of ventilation Mean intrathoracic pressure is decreased Increased venous return Increased cardiac filling IMV versus ACV In patients who are breathing rapidly during ACV and have evidence of over-ventilation (respiratory alkalosis) or hyperinflation (autoPEEP), a switch to IMV should prove beneficial In patients with evidence of respiratory muscle weakness or with a history of LV dysfunction, ACV should be favored over IMV Mechanical Ventilation Pressure Support Ventilation (PSV) Descriptions For patients with spontaneous breathing pattern Ventilator does not deliver a set volume, rather a preset positive pressure Pt determines own inspiratory flow rate and time, and respiratory rate Indications Long-term mechanical ventilation Often used with SIMV to reduce work of breathing Useful method for weaning Mechanical Ventilation Pressure Support Ventilation (PSV) Advantages Reduces work of breathing while maintaining muscle tone Pt determines timing and rate Disadvantages Dangerous if pt’s respiratory rate slows or stops Can be used with PEEP or CPAP but increases the risk of barotrauma or decreased cardiac output Mechanical Ventilation Pressure Controlled Ventilation (PCV) Pressure cycled breathing that is completely controlled by the ventilator, with no participation by the patient The inspiratory flow rate decreases exponentially during lung inflation reducing peak airway pressures and improving gas exchange Disadvantage: inflation volumes vary based on mechanical properties of the lungs Mechanical Ventilation PEEP Description Maintains a preset positive airway pressure at the end of expiration Increases PaO2 so that FiO2 can be decreased Increases DO2 (amt of delivered O2 to tissue) Maximizes pulmonary compliance Minimized pulmonary shunting Indications PaO2 < 60 on FiO2 > 60% by recruiting dysfunctional alveoli Increases intrapulmonary pressure after cardiac surgery to decrease intrathoracic bleeding (research does not support this idea) Mechanical Ventilation PEEP Advantages Improves PaO2 and SaO2 while allowing FiO2 to be decreased Decreases the work of breathing Keeps airways from closing at end expiration (esp. in pts with surfactant deficiency) Disadvantages Increased functional residual capacity (increases risk for barotrauma) Can cause increased dead space and increased ICP In pts with increased ICP, must assure CO2 elimination Contraindicated: hypovolemia, drug induced low cardiac output, unilateral lung disease, COPD Mechanical Ventilation CPAP Description Constant positive pressure is applied throughout the respiratory cycle to keep alveoli open Indications To wean without having to remove the ventilator and having to connect to additional equipment Mechanical Ventilation CPAP Advantages Takes advantage of the ventilator alarm systems providing psychological security of the ventilator being there Disadvantages Patient may sense resistance as he breathes through the ventilator tubing Nursing Care of the Ventilator Record and document the following settings per unit standards Rate (mech and spont) FiO2 Tidal volume (mech & spont) PS/PEEP/CPAP Peak pressure (PIP) SpO2 NEVER use the top of the ventilator as a desk NEVER sit liquids on or near the ventilator NEVER make changes to ventilator settings Refer to RT, MD, NP, or Charge Nurse as needed Care of the Ventilator Patient Observe and document Airway type, size, and position Character of insertion site Date airway inserted Pulmonary assessment Inspection Palpation Percussion Auscultation Provide oral care prn Reapply ETT tape q24h and prn Provide trach care and replace inner cannula q12h and prn Monitor for complications Suction as needed Wean and extubate Mechanical Ventilation Complications Respiratory arrest from disconnection Respiratory infection (VAP) Acid-base imbalances Oxygen toxicity Pneumothorax GI bleeding Barotrauma Decreased cardiac output Troubleshooting Ventilator Alarms High Pressure Alarm – something is blocking airflow (kinked tubing, secretions) Low Pressure Alarm – not enough pressure (tubing disconnected) High Minute Volume Alarm – minute volume is the respiratory rate times the tidal volume – anything that increases RR or Vt will increase Minute volume Low Minute Volume Alarm FiO2 Alarm – usually due to leaving FiO2 at 100% after hyper-oxygenation before suction technique Hazards of Oxygen Therapy Oxygen induced hypoventilation with the following risk criteria: Pts baseline PaCO2 > 50 mmHg Baseline O2 saturation < 90% With supplemental O2, PaO2 doesn’t exceed 60 mmHg Absorption atelectasis with the following risk criteria: FiO2 > 50% Decreasing alveolar volumes Airway obstruction Signs of Oxygen Toxicity Substernal pain Cough Dyspnea Anxiety Paresthesia Fatigue Pulmonary infiltrates Decreased PaO2 Decreased compliance Pulmonary edema Atelectasis Decreased vital capacity Increased shunting (V/Q mismatching) Potentiators of Oxygen Toxicity CO2 inhalation or retention Adrenocortical hormones Epinephrine Thyroid hormones Insulin Amphetamines Norepinephrine Vitamin D deficiency Inhibitors of Oxygen Toxicity Intermittent O2 therapy Acclimation to hypoxia Vitamin E Adrenergic blockers Hypothermia Ganglionic blockers Hypothyroidism Anesthesia Ventilator Weaning Vital Capacity at least 10 – 15 ml/kg Tidal Volume > 5 ml/kg Resting minute volume > 10 L per minute ABG’s adequate on < 40% FiO2 Stable vital signs Intact airway protective reflexes (strong cough) Absence of dyspnea, neuromuscular fatigue, pain, diaphoresis, restlessness, use of accessory muscles Extubation Procedure Explain procedure to patient RT must be at bedside Wash your hands and don PPE Suction airway and oropharynx for pooled secretions (prevents aspiration of secretions atop balloon) Place a towel on patient’s chest Assure new oxygen setup is ready to use Deflate cuff and remove tube instructing patient to cough as tube is removed Apply supplemental oxygen Monitor pt for distress (stridor, coughing, anxiety) Finished You have completed this in-service Please complete the post test, titled: Pulmonary physiology, O2 delivery, and Mechanical Ventilation At the following website