Muscular System
advertisement

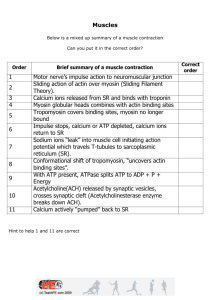
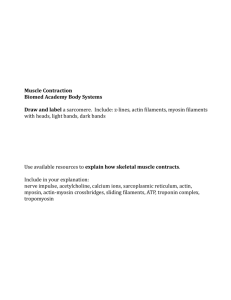
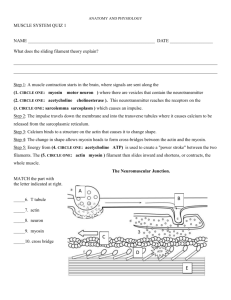
Muscular System Anatomy & Physiology Muscles • From the Latin mus meaning little mouse (Flexing muscles looked like mice scurrying under the skin) • Have ability to transform ATP into mechanical energy • Muscles can only pull, never push, which allows them to exert a force ATP --> ADP + P + Energy ADP + P + Energy ---> ATP Muscle Types Myosin Actin • Skeletal - Slow to Fast twitch • Cardiac - Fast twitch • Smooth - Slow twitch • Twitch = contraction • Skeletal & smooth muscle cells are elongated & called fibers • All have contractile myofilaments actin & myosin Muscle Fxn’s -Produce movement • Skeletal – locomotion & manipulation in response to the environment • Cardiac – moves blood • Smooth – propels (squeezes) stuff through the digestive, urinary, circulatory, and reproductive systems -Maintaining posture -Stabilizing joints -Generating heat (40% of your body heat) Functional Characteristics of Muscle • Excitability (Irritability) – the ability to respond to a stimulus • Contractility – the ability to shorten forcibly when adequately stimulated • Extensibility – the ability to be stretched or extended • Elasticity – the ability of a muscle fiber to recoil & resume its resting length after being stretched Skeletal Muscle • • • • • Striated Multinucleate Voluntary muscles Can generate great power but fatigue quickly Non-rhythmic contraction Gross Anatomy of Skeletal Muscle • Epimysium – outermost layer of dense irregular connective tissue (Surrounds the whole muscle) • Fascicle – bundle of muscle fibers • Perimysium – fibrous C.T. which surrounds the fascicle • Endomysium – each muscle fiber is surrounded by reticular C.T. Sarcoplasmic Reticulum Sarcoplasm = (Cytoplasm with lots of glycogen stored) Sarcolemma (Plasma membrane) Sarcomere Protein Titan Functional unit of muscle Nerve & Blood Supply Each muscle is served by: • 1 nerve • 1 artery • 1 or more veins Skeletal Muscle Attachment Skeletal muscles attach to bones in at least 2 places • When the muscle contracts, the moveable bone (Insertion), moves toward the immovable or less-moveable bone (Origin) • Direct muscle attachment – epimysium fused to periosteum • Indirect muscle attachment – tendon or aponeurosis (flat, sheet-like tendon) Skeletal Muscle Contraction • Sarcomere - contractile unit (z-line to z-line) • Myosin - thick filaments (contain ATPase which is used to split ATP to power muscle contraction) found in the dark Aband. Myosin heads form cross-bridges when attached to actin • Actin - thin filaments found in the light I-band which are anchored to the z-line Sliding Filament Theory • Hugh Huxley 1954 proposed that during contraction actin will slide past myosin which result in overlapping filaments 1. Cross bridge attachment 2. Power stroke (Myosin head pivots pulling actin) 3. Cross bridge detachment (ATP binds to myosin head loosening the bond to actin) 4. “Cocking” the myosin head – ATPase hydrolyzes ATP to ADP & Pi returning the myosin head to it’s cocked position Tropomyosin & Troponin • Tropomyosin – stiffen the actin protein & block myosin binding sites in relaxed muscle fibers, preventing myosin & actin from forming a crossbridge • Troponin – regulates cross-bridge formation. In the presence of Ca2+ troponin moves tropomyosin, thereby exposing the myosin binding sites Z- Line - Defines each end of the sacromere. Thin filaments of adjacent sarcomeres are linked together here. A band - Consists of overlapping thin and thick filaments. I band - Only thin filaments. H zone - Only thick filaments. This also shortens during contraction. Thin Fibers - Each thin filament is made of three different proteins. Actin - Actin filaments are made of subunits called G-actin; these are globular proteins which are linked together to form a filament. Myosin binding site - Each G-actin contains a binding site for myosin head groups (part of the thick filament) Troponin - This protein is associated with actin and it binds calcium. Tropomyosin -The third protein of the group; when the muscle fiber is not contracting, tropomyosin covers the myosin binding site, preventing the myosin head groups from binding to actin. Thick Fibers Consists of a bundle of proteins called myosin Myosin Tails Each tail has two head groups at the same end and each has two binding sites. heads form cross bridges Actin binding site - This binds to the myosin binding site on actin, when it is exposed as tropomyosin moves. ATP-binding site - Binds to ATP; splits the molecule and the released energy is used to drive the movement of the myosin head groups. Power Stroke Calcium • Sarcoplasmic reticulum – regulates intracellular Ca2+ by storing & releasing Ca2+ when a stimulus causes the muscle to contract • T (Transverse) Tubules – extensions of the sarcolemma which allow for rapid impulse transmission through the muscle which ensures a single muscle contraction Step 6. The trans port of calcium ions back into the s arcoplas mic reticulum. Step 5. The hydrolysis of ATP, whichleads to the re-energizing and repos itioning of the cros s bridge. Step 1. The infux of calcium, triggering the exposure of binding sites on actin. Step 2. The bindin g of myos in to actin. Step 4. The binding of ATP to the cros s bridge, which results in the cross bridge dis connecting from actin. Step 3 . The po wer s troke of the cro ss brid ge that causes the s liding o f the thin filaments . Regulation of Contraction • Muscle contraction is stimulated by an action potential from a nerve • The neuromuscular junction (motor end plate) in skeletal muscle is regulated by acetylcholine (ACh) • Ach needs to be broken down as soon as it is used; the enzyme acetlycholinesterase serves this function. 1. ACH released 2. AP propagated along membrane and at Ttubules 3. Ca released from SR voltage gated Ca channel opens 4. Ca binds to Troponin-C conformation changes favor tropomyosin opens actin sites 5. myosin cross-bridges attach-detach from actin...pulls filament toward M-line 6. Ca removed (uptake by SR) 7. tropomyosin blocks actin sites relaxation a. b. c. Generating an Action Potential • Depolarization (Na channels open) • Repolarization (Na channels close K channels open) • Refractory Period (K channels close) • Na/K pump Homeostatic Imbalance • Myasthenia gravis – autoimmune disease where ACh receptors are broken down by ACh antibodies resulting in drooping eyelids and general muscle fatigue • Curare – arrowhead poison used in South America which blocks ACh receptors resulting in respiratory arrest & death • Cobra venom – same as curare • Botulinum toxin prevents ACh release • Black widow spider venom releases all Ach • Nerve gasses inhibit AChase which keeps cleft flooded with ACh ACh destruction • After ACh initiates the action potential the ACh is broken down by acetylcholinesterase • This prevents continued muscle contraction in the absence of additional nerve stimuli Mysostatins control muscle growth Absence of results in enlarged muscle development Energy for muscle contraction ATP is needed for… 1) contraction - Cocking and detachment of the myosin head. 2) calsequestrin - Pumping calcium into the SR of the sarcoplasm. 3) Na+/K+-ATPase - Needed for impulse conduction.. ATP Production • ATP lasts - Only a few seconds during active muscle contraction as ATP stores are used up. • ATP is quickly reconstituted -There are several mechanisms that replenish the ATP stores. • Sources of energy for ATP production 1) phosphocreatine (creatine phosphate, CP) ATP is produced from another high energy molecule called phosphocreatine. • Creatine kinase • Breaks down phosphocreatine, releasing a phosphate and energy. The energy is used to make new ATP. • This store of energy lasts about 8-15 seconds. ATP Production 2) Anaerobic Respiration & Glycolysis Glycogen - A polymer of glucose. For the muscle to recover the lactic acid needs to be removed quickly; a well vascularized muscle serves this purpose. lasts about 2 minutes. Lactic acid/pyruvic acid The product of anaerobic respiration is pyruvate; as no oxygen is available the pyruvate is converted to lactic acid. As lactic acid builds up in the muscles it changes the pH of the tissues in the muscle, which causes a decrease in the efficiency of proteins and enzymes. This leads to soreness and fatigue. ATP Production • Oxidative metabolism a.k.a. Aerobic Respiration - Oxygen used by mitochondria to produce 36 net ATPs (2 from glycolysis and 34 from Krebs and ETC) • Can produce ATP indefinitely as long as you have oxygen and energy stores (fat, proteins or glucose.)