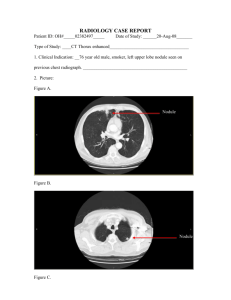
Lung Nodules
advertisement

Lung Nodules Frans Naudé Definition of Pulmonary nodule • Rounded opacity , moderately well defined • < 3cm in diameter Web p 97 General Approach to lung nodules Position • Is it a lung nodule? – Skin tags, nipple shadows, bone lesions • Distribution in the lung Number of Nodules ( SPN, Multiple) Compare with previous radiographs Interpreting CXR p102 Web p185 P84, Computed Tomography of the Lung, Verschakelen Lung nodules: Imaging Modalities • CXR • CT ( HRES) • PET/CT : F18-FDG Description of pulmonary nodule • Pattern of distribution (Relationship to fissures, pleura, secondary lobules) • Edge characteristics (sharp, poorly circumscribed, ground glass) • Morphology ( branching/ tree in bud) • Size: – Pulmonary nodule <3cm – Small nodule < 1cm Web p97 High resolution CT of the lung Large nodules 1-3cm (Easily seen on CXR) HRES CT Anatomy of pulmonary lobule Secondary pulmonary lobule (1) interlobular septa (2) centrilobular region (3) lobular lung parenchyma Blue = Pulmonary veins Green = lymphatic's Yellow= bronchiolar branches Red = Arteries White = Connective tissue Computed Tomography of the lung p9 Secondary pulmonary lobule Prof Naidich HRES CT • Interstitial nodules vs Air space nodules WEB-Algorithmic approach to nodules Interstitial Air space Well defined Ill defined Soft tissue attenuation Homogenous soft tissue Obscure edges of vessels they touch Hazy and less dense than adjacent vessels Peripheral in Pulm. Lobule Central P120 High resolution CT lung ,Web - approach CT of the lung , p74 CT of the lung , p72 HRES CT High resolution CT lung ,Web – Algorithm 4 Airspace nodules • = centrilobular distribution • = no pleural/septal nodules • Ground-glass opacification/ less dense than adjacent blood vessels Centrilobular nodules : Tree in Bud Tree – in - Bud • PT with TB • Indicative of endobronchial spread P83, Computed Tomography of the Lung,Verschakelen Infective bronchiolitis Tree in Bud appearance Bronchial wall thickening Computed Tomography of the Lung,Verschakelen HRES CT Tree in bud absent High resolution CT lung ,Web - approach Centrilobular: Tree in bud absent Poorly defined hazy ground glass nodules • Respiratory bronchiolitis • Langercell histiocytosis • Lymphocytic interstitial pneumonitis Interstitial nodules • = pleural/ septal predominance HRES CT Perilymphatic High resolution CT lung ,Web - approach Perilymphatic disease • Clustered nodules • Adjacent to fissures and pleural surfaces and along central vascular structures • DDX: Sarcoid, silicosis, CWP. • Rare: Amyloid ,LIP • Sarcoidosis P83, Computed Tomography of the Lung,Verschakelen Silicosis Web p305 Web p 306 Coal workers pneumoconiosis Web p 306 Diffuse pattern more in favour of CWP or silicosis than sarcoidosis HRES CT Random High resolution CT lung ,Web - approach Random nodules • Sharply define,+- feeding vessel DDX 1. Metastases: lung, breast, kidney, colon, melanoma, thyroid , pancreas 2. Infection: Milliary TB, septic emboli, fungal infection 3. Vasculitis 4. Langercell histiocytosis Metastases • Random • Basilar predominance P82, Computed Tomography of the Lung,Verschakelen CT of the lung, p 75 Perilymphatic vs. centrilobular Sarcoidosis - Fissural and subpleural nodules TB Centrilobular changes : nodules, tree-inbud, branching lines (A) Perilymphatic nodules. Nodules are immediately in contact with interlobular septa and the visceral pleura (B) Centrilobular nodules. Nodules are positioned 5 - 10 mm from costal and visceral pleural surfaces and interlobular septa. High resolution CT lung ,Web - approach References • • • • High resolution CT of the lung, Web, Naidich CT of the lung, Verschakelen, De Wever Prof Naidich RSSA lecture High-Resolution CT of the Lung: Patterns of Disease and Differential Diagnoses, Radiol Clin N Am 43 (2005) 513 – 542 • Imaging of Interstitial Lung Disease, Radiol Clin N Am 43 (2005) 589 – 599 SPN Def: focal area of increased round /oval density in the lung parenchyma measuring less than 3cm, Cause : infection, malignancy , inflammation, vascular, congenital Risk : 30-40% malignant Radiographics 2000:20: 43 Approach to SPN • Morphology: • - Size ( smaller more likely benign) • - margins and contours Margins Risk for malignancy Smooth 21% Lobulated ( uneven growth 75% Irregular ,spiculated, distortion of blood vessels Very high risk Internal characteristics • Homogeneous attenuation (55% benign, 20%malignant) • Pseudocavitation and air bronchograms: lymphoma or bronchioalveolar cancer • Benign cavitation : smooth ,thin walls (<4mm) • Malignant cavitation: thick irregular walls( >16mm) • Intranodular fat = hamartoma • Benign calcification : – post infection: central, diffuse solid, laminated , – hamartoma : popcorn like • Malignant calcification: diffuse,amorphous,punctate • Metastatic osteosarcoma: high attenuation nodule • 25-39% malignant nodules classified as benign on radiological morphology assessment • growth rate assessment: doubling rate ( increase in diameter of >26%) for malignant nodules between 30-400 days • Clinical data: age, risk factors, previous malignancy Distribution of lung nodules • Cancer – basal predominance • Breast CA, Colon, Renal often metastasize to lung Interpreting CXR p100 Size of lung nodules • Mayo clinic CT screening trial • ( in patients with no history of cancer) • • • • • <3mm = less than 0,2% malignant <5mm = fewer than 1% malignant 4-7mm = 0,9% malignant 8-20mm = 18% malignant >20mm = 50% malignant Radiology Nov 2005 p 397 Follow-up National Lung Screening Trial • nodules smaller than 4mm • return for screening after 12 months, without interval scans or other work-up Radiology Nov 2005 p 397 Radiology Nov 2005 p 398