These Power Point slides are for the use of all GRACE investigators

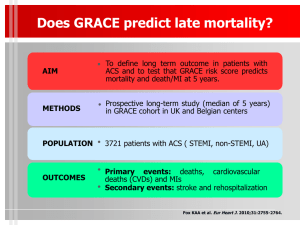
Global Registry of Acute
Coronary Events
Assessing Today’s Practice Patterns to
Enhance Tomorrow’s Care
Supported by an unrestricted educational grant from sanofi-aventis to the Center for Outcomes Research
University of Massachusetts Medical School
What is GRACE?
Global Registry of Acute Coronary Events
Largest multinational registry covering the full spectrum of ACS
Generalizable patient inclusion criteria
In-hospital and 6-month follow-up
Representative of the catchment population:
(clusters of hospitals)
Full spectrum of hospitals and facilities
Training, audit and quality control
International Scientific
Advisory Committee
International Advisory Committee
‘ Americas’ clusters
Chair: JM Gore
8 advisors
40 subsite cardiologists
‘European’ clusters
Chair: KAA Fox
8 advisors
40 subsite cardiologists
Scientific Advisory Committee
Co-Chairs Keith AA Fox, UK
Joel M Gore, USA
Publications
Co-Chairs
Kim A Eagle, USA
Ph Gabriel Steg, France
Study Co-ordination Fred Anderson, University of Massachusetts
Argentina
Enrique Gurfinkel
Australia/New Zealand
David Brieger
Belgium
Frans J Van de Werf
Brazil
Álvaro Avezum
Canada
Shaun Goodman
Germany
Dietrich C Gulba
Italy
Giancarlo Agnelli
France
Gilles Montalescot
Ph Gabriel Steg
Poland
Andrzej Budaj
Spain
José López-Sendón
United Kingdom
Keith AA Fox
Marcus Flather
United States
Frederick A Anderson
Kim A Eagle
Robert J Goldberg
Joel M Gore
Christopher B Granger
Brian M Kennelly
Objectives of GRACE
Identify opportunities to improve the quality of care for patients with ACS
Describe diagnostic & treatment strategies,
& hospital & post-discharge outcomes
Develop hypotheses for future clinical research
Disseminate findings to a wider audience
Core GRACE Study Design
~100 hospitals in 13 countries
– Europe, North & South America, Australia,
New Zealand
Population-based clusters with community hospitals and referral centres
First 10-20 consecutive cases per centre/month: qualifying symptoms PLUS evidence of CAD
Random audit of all centres: 3 year cycle
1
6
Cluster Strategy for Study
Sites: Population-Based Design
2
3
18 advisory committee members
~ 100 hospitals
~ 10,000 ACS patients/year
4
5
Multinational Site Network
Argentina 6 sites
Australia 6 sites
Belgium 6 sites
Brazil 7 sites
Canada
France
5 sites
7 sites
Germany
Italy
5 sites
5 sites
New Zealand 2 sites
Poland 6 sites
Spain
UK
USA
3 sites
5 sites
18 sites
81 Active Core Study Sites:
16 Clusters in 13 Countries
Q3-2006
Status of 16 Core Clusters
60,723 cases enrolled
85% six-month follow-up
The “Big Picture”
Core GRACE & GRACE 2
GRACE Core
60,723 patients
81 hospitals
13 countries
GRACE Core
Substudy 1
Substudy 2
Substudy 3
GRACE 2
24,513 patients
153 hospitals
23 countries
234 Core GRACE & GRACE 2
Study Sites in 29 Countries*
*29 countries = 17 GRACE 2 + 6 core GRACE + 6 both
Q3-2006
Status: September 30, 2006
81 Core & 153 Expanded Sites
29 countries
234 hospitals
85,236 cases
Internet Website www.outcomes.org/grace
Hospital Characteristics
Q4-2001 vs. Current Quarter
Number of Hospitals
Coronary care unit
Emergency department
Cardiac catheterization laboratory
Open heart surgery
Hospital beds (mean)
Coronary care unit beds (mean)
ACS admissions (mean, per year)
Q4-2001 Q3-2006
109 81
94% 99%
86% 91%
65% 74%
43% 51%
416 555
10 11
487 640
Q3-2006
60,723 Cases Enrolled as of September 30, 2006
70000
Initial CRF 6-Month Follow-up
60000
55454
57406 58866
60723
50000 46945
43117
45106 46521
48045
40000
38444
35301
30000
28699 27618
20000
10000
0
19453
13245
2411
233
11543
6689
20303
1999 2000 2001 2002 2003 2004 2005 Q1-06 Q2-06 Q3-06
Quarter-Year
Q3-2006
Classification of Cases
40%
30%
34%
Q3-2006
20%
10%
0%
STEMI
29%
UA
30%
7%
NSTEMI Other
Hospital Discharge Status
Death
Home
Transfer *
Other
STEMI NSTEMI UA
8% 4% 3%
77%
9%
6%
78%
11%
6%
87%
9%
2%
* Transfer to another acute care hospital.
Q3-2006
Admission versus Final
Diagnosis
UA
N=4999
(44%)
*Missing diagnosis in 236 patients
MI
N=4100
(36%)
‘Rule-out’ MI
N=957
(9%)
Unspecified chest pain
N=745
(7%)
Other cardiac
N=381
(3%)
Non-cardiac
N=125
(1%)
STEMI
N=3419
(30%)
Non-STEMI
N=2893
(25%)
Unstable angina
N=4397
(38%)
Other cardiac
N=508
(4%)
Non-cardiac
N=326
(3%)
Admission diagnoses versus final diagnoses (derived from discharge diagnosis, electrocardiographic changes and cardiac enzymes) in 11,543 patients with acute coronary syndromes. Figures expressed as percentage of total ACS.
Fox KAA et al.Eur Heart J 2002;23:1177-89.
Baseline Characteristics
STEMI NSTEMI UA
(n = 13,862) (11,316) (12,509)
Median age (years)
Male (%)
65
70
Prior history (%)
• Angina
• Myocardial infarction
• PCI/CABG
• Smoking
• Diabetes mellitus
• Hypertension
• Hyperlipidemia
43
20
8/5
62
21
52
38
Participant in clin trial (%) 117
68
66
56
32
15/14
57
28
62
47
7
66
64
78
41
25/19
55
26
66
54
Hospital Treatment According to Admission Diagnosis
MI UA ? MI Chest pain n 16,304 15,266 3,474 3,266
% %
ACE inhibitors
Aspirin
-blockers
Ca 2+ blockers
Gp IIb/IIIa: no PCI
69
94
83
15
5
Gp IIb/IIIa with PCI 26 11
LMWH 52 64
UFH
Thrombolytic agents
59
35
43
2
56
92
81
34
4
%
56
92
81
30
7
15
40
51
3
%
55
92
79
29
7
18
40
51
3
Diagnostic Procedures
100%
80%
60%
40%
20%
0%
78%
69%
58%
LVEF
STEMI NSTEMI UA
73%
60%
47%
18% 17%
25%
Echo Stress test
Hospital Cardiac Interventions
According to Final Diagnosis
Intervention STEMI NSTEMI UA n 13,862 11,316 12,509
Cardiac catheterization
PCI
%
62
45
%
57
31
%
49
23
CABG 4 7 6
Treatments at Discharge
STEMI NSTEMI UA n 13,862 11,316 12,509
ACE inhibitors
Aspirin
-blockers
Ca 2+ blockers
%
67
92
78
10
%
56
89
76
20
%
52
88
72
31
Statins
Warfarin
63
8
59
7
57
7
10
5
0
20
15
8
5
3
Hospital Outcome by
Final Diagnosis
STEMI (13,862)
NSTEMI (11,316)
UA (12,509)
4
3
2
Death Major Bleed
1.3
0.9
0.5
Stroke
12
8
4
0
Hospital Outcomes
10.7
<0.0001
Elderly patients (>=75)
Younger patients (65-<75)
5.6
5.6
<0.0001
4.0
Death Major bleed
Lankes W et al.Eur Heart J 2002;23(Abstr Suppl):502.
What proportion of eligible patients receive reperfusion therapy?
Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the
Global Registry of Acute Coronary Events
(GRACE)
Kim A. Eagle, Shaun G. Goodman, Álvaro Avezum,
Andrzej Budaj, Cynthia M. Sullivan, José López-Sendón, for the GRACE Investigators
Lancet 2002;359:373-77
Missed Opportunities for
Reperfusion
ST ↑ or LBBB, <12 hrs from onset, no contraindications n
ANC (%) US (%) AB (%)
269 327
EUR (%)
339 739
PCI alone 1.1
Lytic alone 66.9
Both 2.2
Neither 29.7
17.7
30.6
18.7
33.0
13.9
53.1
5.0
28.0
16.2
49.4
4.9
29.5
AB, Argentina/Brazil; ANC, Australia/New Zealand/Canada; EUR, Europe; US, United States
Eagle KA et al. Lancet 2002;359:373-7.
Independent Predictors of
No Reperfusion
Variable OR (95% CI)
Prior CABG
History of diabetes
2.28
(1.35 - 3.87)
1.46
(1.11 -1.94)
History of congestive heart failure 2.92
(1.84 - 4.67)
Presentation without chest pain 2.23
(2.13 - 4.89)
*Age
75 years 2.37
(1.82 - 3.08)
*As compared to the <55 years age group
Eagle KA et al. Lancet 2002;359:373-7.
100
80
20
0
60
40
80
20
Geographical Variation:
Admission to Hospitals with/without Access to Cath Lab
78
Cath lab No cath lab
22
61
39
USA Europe ANC
ANC, Australia/New Zealand/Canada; AB, Argentina/Brazil
82
AB
18
Global patterns of use of antithrombotic and antiplatelet therapies in patients with acute coronary syndromes: Insights from the Global
Registry of Acute Coronary Events (GRACE)
Andrzej Budaj, David Brieger, Ph Gabriel Steg, Shaun G. Goodman,
Omar H. Dabbous, Keith A. A. Fox, Álvaro Avezum, Christopher P.
Cannon, Tomasz Mazurek, Marcus D. Flather, and
Frans Van De Werf, for the GRACE Investigators
Am Heart J 2003;146:999-1006.
100
80
Geographic Practice Variation
92 92 91
95
United States
Australia/New Zealand/Canada
Europe
Argentina/Brazil
58
65
60
40
20
37
17
30
24
33
8
15
9
13
39
0
PCI GP IIb/IIIa LMWH ASA
Budaj A et al. Am Heart J 2003;146:999-1006.
Antithrombotic Rx Used
LMWH + llb/IIIa
2%
UFH + llb/IIIa
4%
None
18%
UFH
30%
LMWH
46%
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
9
6
3
0
Incidence of Major Bleeding
UFH
LMWH
UFH + IIb/IIIa
LMWH + IIb/IIIa
3.9
2.4
8.3
2.9
Major bleed
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
UFH
LMWH
UFH +
IIb/IIIa
Multivariate Adjusted Odds of
Major Hemorrhage
Major hem
3.9%
OR=0.55
P<0.001
2.4%
OR=2.26
8.3%
LMWH +
IIb/IIIa
2.9%
0 0.5
1 2 3
Lower Higher
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
Safety Events
3
2
1
0
UFH
LMWH
UFH + IIb/IIIa
LMWH + IIb/IIIa
2.9
1.5
1.2
0.7
0.7
0.6
0.6
0.1
0
0.3
0
ICH
0
Stroke
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
15
10
5
Major Cardiac Events
UFH
LMWH
UFH + IIb/IIIa
LMWH + IIb/IIIa
6.3
6.6
11.3
9.9
5
2.9
2.9
4.4
10.6
13.8
12.4
5
0
Death MI Death/MI
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE)
M. Moscucci, K.A.A. Fox, Christopher P. Cannon, W. Klein,
José López-Sendón, G. Montalescot, K. White, R.J. Goldberg, for the GRACE Investigators
European Heart Journal 2003;24:1815-1823
4
3
2
1
0
6
5
Overall
NSTEMI
3.9
Incidence of Major Bleeding
UA
STEMI 4.7
4.8
2.3
Major Bleed
Moscucci M et al.Eur Heart J 2003;24:1815-23.
Predictors of Major Bleed
Variables
Age (per 10 year
↑)
Female gender
History of renal insufficiency
History of bleeding
Killip Class IV
MAP (per 20 mmHg
↓)
IV Inotropics
Overall UA STEMI x x x x x x x x x x x x x x x
Other vasodilators x x
Thrombolytics
Diuretics
Unfractionated heparin
IIb/IIIa receptor blockers
PA catheters x x x x x x x x x x x
PCI x x x
Thrombolytics and IIb/IIIa inhib x x
Moscucci M et al.Eur Heart J 2003;24:1815-23.
NSTEMI x x x x x x x x x x x
In-Hospital Mortality Rates
50
40
30
20
10
0
** P <0.001
No Major Bleed
Major Bleed
**
18.6
**
16.1
**
**
22.8
15.3
5.1
5.3
7.0
3.0
Overall Unstable Angina NSTEMI
Moscucci M et al.Eur Heart J 2003;24:1815-23.
STEMI
Outcome of “Low-risk”
Patients with ACS
Presentation with UA in the absence of dynamic
ECG changes, no troponin elevation, no arrhythmia nor hypotension
Abnormal ECG in 38%,
27% stress test, 37% echo, 52% angio
6 month outcome:
– 23% readmission
– 12% revascularized
– 3% deaths
“Low-risk” is not no risk
Devlin et al.Eur Heart J 2001;22(Abstr Suppl):525.
Evidence Based Medicine
Total Population = 9,980
Therapy
ST
MI Non- ST
MI UA % of pts who are
(n=2,501) (n=2,504) (n=3,631) eligible
ASA
B blocker
ACE-I
Reperfusion
GP IIb/IIIa/LMWH
X
X
X
X
X
X
X
X
X X
Granger CB et al. J Am Coll Cardiol 2001;37(2 Suppl A):503A.
60%
40%
20%
GRACE: Use of EBM in
“Eligible” Patients
100% 93%
89%
80%
81%
71%
64%
57%
In-hosp
Discharge
70%
14%
PTCA
58%
14%
IIb/IIIa
56% lytics
48%
LMWH
0%
ASA B-blocker ACE-I Reperf LMWH/IIb/IIIa n=5,373 n=4,480 n=3,254 n=1,963 n=4112
Granger CB et al. J Am Coll Cardiol 2001;37(2 Suppl A):503A.
Management of acute coronary syndromes. variations in practice and outcome: Findings from the Global Registry of Acute Coronary
Events (GRACE)
K.A.A. Fox, S.G. Goodman, W. Klein, D. Brieger, P.G. Steg,
O. Dabbous and Á. Avezum for the GRACE Investigators
Eur Heart J 2002;23:1177-1189
100
80
Geographic Practice Variation:
Discharge Medication
47
United States
Australia/New Zealand/Canada
Europe
Argentina/Brazil
49
54 53 53
57
50
94 93 94 93
60
40
26
20
0
ACE
** P <0.01
AT/AC, antithrombin or anticoagulant
Statin AT/AC
Fox KAA et al. Eur Heart J 2002;23:1177-89
.
Increase in Diagnosis of MI
Utilizing Troponin
30
25
20
15
10
26
15 n=3420 of 8213 with CK, CK-MB
& troponin measurements
9
5
0
Troponin + in addition to CK ULN
Troponin + in addition to CK 2 x ULN
Troponin + in addition to CK-MB ULN
Goodman SG et al. J Am Coll Cardiol 2001;37(2 Suppl A):358A
.
8
6
4
2
In-Hospital Mortality
OR & 95% CI n=900
3
*
(1.6 - 5.7) n=124
2.1
(0.6 - 7.4) n=1111
5.8
*
(3.3 - 10.1)
0
*p<0.05
Troponin– Troponin +
CK > 2 x ULN
Troponin–
CK > 2 x ULN
Troponin +
Goodman SG et al. J Am Coll Cardiol 2001;37(2 Suppl A):358A
.
Impact of Aspirin on Presentation and
Hospital Outcomes in Patients with Acute
Coronary Syndromes (The Global Registry of Acute Coronary Events [GRACE])
Frederick A. Spencer, Jose J. Santopinto, Joel M. Gore, Robert J.
Goldberg, Keith A.A. Fox, Mauro Moscucci, Kami White, and
Enrique P. Gurfinkel
Am J Cardiol 2002;90:1056-1061
40
20
0
100
80
60
Impact of Prior ASA on ACS:
GRACE
77.8
74.5
70.3
69.5
Australia/New Zealand/Canada
Europe
South America
USA
18.1
18.5
18.3
25.4
Hx of CAD (n=4974) No Hx of CAD (n=6414)
Prior long-ASA use according to geographic region and history
80
60
40
20
0
15
26
Type of ACS and Hospital
Mortality in Patients with History of CAD Stratified By Prior ASA
Prior ASA No prior ASA
58
28 29
45
Impact of prior ASA on:
– STEMI 0.52
(0.44,0.61)*
– Death 0.69
(0.5,0.95)**
3
7
STEMI NSTEMI UA Death
*Controlled for age, sex, medical hx, prior therapies, in hospital therapies
**Controlled for above plus MI type
60
40
20
25
51
Type of ACS and Hospital Mortality in Patients without History of CAD
Stratified By Prior ASA
Prior ASA
31
27
No prior ASA
44
23
Impact of prior
ASA on:
– STEMI 0.35
(0.30,0.40)*
– Death 0.77
(0.55,1.07)**
5
6
0
STEMI NSTEMI UA Death
*Controlled for age, sex, medical hx, prior therapies, in hospital therapies
** Controlled for above plus MI type
Association of Statin Therapy with Outcomes of Acute Coronary Syndromes: The GRACE
Study
Frederick A. Spencer, Jeanna Allegrone, Robert J. Goldberg, Joel M.
Gore, Keith A.A. Fox, Christopher B. Granger, Rajendra H. Mehta and
David Brieger for the GRACE Investigators*
Ann Intern Med 2004;140:857-866
Prior and Early Utilization of Statins in Patients with ACS: GRACE
18000
16000
14000
12000
10000
8000
6000
4000
2000
0
Hospital Statins No Hospital Statins
N/N
N/Y
N/Y
Y/Y
Prior Statins No Prior Statins
Ann. Intern Med. 2004;140:856-866.
Final Diagnosis of ACS Patients
According to Previous Treatment with Statins
St elevation MI* non-ST elevation MI Unstable angina
100
80
60
40
20
0
Previous Statin Use No Previous Statin Use
*Multivariate analysis: Prior statin users less likely to present with STEMI -OR 0.79 (0.71,0.88)
Ann. Intern Med. 2004;140:856-866.
Outcome
Death
Hospital Outcomes of ACS
Patients Stratified by Statin Use
Prior statins
Only
Prior & Hospital
Statin
Hospital Statins
Only
1.39
(0.91,2.14) 0.20
(0.16,0.25) 0.38
(0.30,0.48)
Recurrent MI
Stroke
0.69
1.08
(0.43,1.11)
(0.43,2.73)
0.90
0.68
(0.75,1.07)
(0.42, 1.12)
1.22
(1.08,1.37)
0.80
(0.57, 1.14)
Composite 1.02
(0.74,1.41) 0.66
(0.56,0.77)
*Compared to patients never receiving statins
Ann. Intern Med. 2004;140:856-866.
0.87
(0.78,0.97)
Comparison of Outcomes of Patients With
Acute Coronary Syndromes With and Without
Atrial Fibrillation
Rajendra H. Mehta, Omar H. Dabbous, Christopher B. Granger,
Polina Kuznetsova, Eva M. Kline-Rogers, Frederick A. Anderson, Jr.,
Keith A.A. Fox, Joel M. Gore, Robert J. Goldberg and Kim A. Eagle for the GRACE Investigators
Ann J Cardiol 2003;92:1031-1036
Major bleed
Stroke
Cardiac arrest
Pulmonary edema
Shock
Death
Adjusted ORs for Hospital
Events in Patients with ACS and
New-Onset Atrial Fibrillation
AF Better AF Worse
0 0.5 1 1.5 2 2.5 3 3.5 4
Odds Ratio
Am J Cardiol 2003;92(9):1031-6
Major bleed
Stroke
Cardiac arrest
Pulmonary edema
Shock
Death
Adjusted ORs for Hospital Events in Patients with ACS and Previous
Atrial Fibrillation
AF Better AF Worse
0 0.5 1 1.5 2 2.5
Odds Ratio
Am J Cardiol 2003;92(9):1031-6
Determinants and Prognostic Impact of Heart
Failure Complicating Acute Coronary
Syndromes: Observations From the Global
Registry of Acute Coronary Events (GRACE)
Philippe Gabriel Steg, Omar H. Dabbous, Laurent J. Feldman, Alain
Cohen-Solal, MarieClaude Aumont, José López-Sendón, Andrzej
Budaj, Robert J. Goldberg, Werner Klein, Frederick A. Anderson, Jr, for the Global Registry of Acute Coronary Events (GRACE)
Investigators
Circulation. 2004;109:494-499
Impact of Heart Failure on
Admission on Hospital Mortality
>75 years
65-74 years
55-64 years
<55 years
3.1
(2.4,3.9)
3.3
(2.3,4.8)
5.0
(2.9,8.3)
Lower odds ratio for death
*Relative to patients without HF
1 10 20
Higher odds of death
Circulation 2004;109:494-499.
10.1
(5.3,19.2)
Death Rates from Hospital Admission to 6-Month Follow-Up for Patients
According to Timing of Heart Failure
Circulation 2004;109:494-499.
Group
All patients
STEMI
Hospital Case-Fatality Rates
According to Development of
Heart Failure
Non-STEMI
Unstable angina
HF (+)
12.0%
16.5%
10.3%
6.7%
HF (-)
2.9%
4.1%
3.0%
1.6%
Circulation 2004;109:494-499.
Stenting and Glycoprotein IIb/IIIa Inhibition in
Patients With Acute Myocardial Infarction
Undergoing Percutaneous Coronary Intervention:
Findings From the Global Registry of Acute
Coronary Events (GRACE)
Gilles Montalescot, Frans Van de Werf, Dietrich C. Gulba, Àlvaro
Avezum, David Brieger, Brian M. Kennelly, Tomasz Mazurek,
Frederick Spencer, Kami White, and Joel M. Gore for the GRACE
Investigators
Catheterization & Cardiovascular Interventions. 60:360-367 (2003)
Probability of Survival at
6 Months (all PCI)
Death rates:
+GP +stent 7.3%
-GP +stent 6.7%
+GP –stent 12.8%
-GP – stent 14.4%
Montalescot G et al.Catheter Cardiovasc Interv 2003;60:360-7.
Probability of Survival at
6 Months (Primary PCI)
Death rates:
+GP +stent 7.7%
-GP +stent 8.7%
+GP –stent 7.4%
-GP –stent 20.1%
Montalescot G et al.Catheter Cardiovasc Interv 2003;60:360-7.
Six-Month Outcomes in a Multinational
Registry of Patients Hospitalized With an
Acute Coronary Syndrome (The Global
Registry of Acute Coronary Events [GRACE])
Robert J. Goldberg, Kristen Currie, Kami White, David Brieger,
Phillippe Gabriel Steg, Shaun G. Goodman, Omar Dabbous, Keith
A.A. Fox and Joel M. Gore for the GRACE Investigators
Am J Cardiol 2004;93:288-293
Six-Month Follow-Up*
STEMI NSTEMI UA
Death 5% (480/9414) 6% (496/7977) 4% (349/9357)
Stroke 1% (110/9173) 1% (103/7749) 1% (79/9176)
Rehospitalized 18% (1619/9147) 19% (1501/7721) 19% (1761/9150)
*Excluding events that occurred in hospital
Goldberg RJ et al.Am J Cardiol 2004;93:288-93.
20
15
Discharge to 6 Month Outcomes:
Cardiac Interventions
Scheduled and unscheduled procedures
16.2
14.7
15.7
STEMI (5,476)
NSTEMI (5,209)
UA (6,149)
10
9.3
8.0
8.3
5.0
7.1
6.1
5
0
Cardiac cath PCI CABG
Goldberg RJ et al.Am J Cardiol 2004;93:288-93.
6 Month Follow-up
10
5
0
30
25
20
15
UFH
LMWH
UFH + IIb/IIIa
LMWH + IIb/IIIa
12.2
7.8
23.1
18.1
19.7
18.5
27.6
19.0
5.8
6.4
4.1
5.7
Death MI Rehosp
Cannon CP et al.Eur Heart J 2001;22(Abstr Suppl):592.
Total Outcomes:
Admission to 6 Months
30
20
10
0
STEMI (2075)
NSTEMI (1856)
UA (2883)
12
13
8
Death
3 3
1.5
Stroke
17
20 20
Urgent readmission for cardiac event
Survival Rate 6 Months Post
Discharge for STEMI, NSTEMI, and UA Patients
100
90
80
70
60
50
STEMI Non-STEMI
0 1 2 3 4
Months after hospital discharge
Goldberg RJ et al.Am J Cardiol 2004;93:288-93.
5
UA
6
Factors Associated With An
Increased Risk of Post-Discharge
Death
Characteristic
Age (yrs)
65-74
>75
Medical history
HF
MI
TIA/Stroke
STEMI
HR 95% CI
3.48
8.95
2.21
1.69
2.00-6.06
5.28-15.20
1.61-3.04
1.28-2.22
Non-STEMI
HR 95% CI
2.17
5.30
1.27-3.72
3.19-8.80
2.20
1.71-2.84
1.37
1.03-1.84
Hospital complications
Cardiogenic shock
HF
Stroke
1.94
1.20-3.15
2.16
1.65-2.83
2.51
1.32-4.78
1.91
Goldberg RJ et al.Am J Cardiol 2004;93:288-93.
1.49-2.44
Factors Associated with an
Increased Risk of Post-Discharge
Death in Patients with UA
Characteristic
Age (yrs)
55-64
65-74
Medical history
HF
MI
PCI
Hospital complications
Cardiogenic shock
HF
HR
3.34
5.29
2.23
1.44
0.52
4.01
1.67
95% CI
1.81-6.19
2.88-9.72
1.61-3.08
1.09-1.91
0.35-0.77
1.73-9.28
1.17-2.37
Goldberg RJ et al.Am J Cardiol 2004;93:288-93.
From guidelines to clinical practice: the impact of hospital and geographical characteristics on temporal trends in the management of acute coronary syndromes:
The Global Registry of Acute Coronary Events
(GRACE )
Keith A.A. Fox, Shaun G. Goodman, Frederick A. Anderson Jr.,
Christopher B.Granger, Mauro Moscucci, Marcus D. Flather ,
Frederick Spencer, Andrzej Budaj, Omar H. Dabbous, Joel M. Gore on behalf of the GRACE Investigators
European Heart Journal 2003;24:1414-1424
Temporal Trends in
ACS Diagnostic Categories
STEMI Non-STE MI UA
50%
40%
30%
20%
10%
0%
1999
(n=5513)
2000
(n=8787)
2001
(n=8934)
Year of Discharge
2002
(n=8944)
2003
(n=5924)
Temporal Trends STEMI:
In-hospital Therapies
LMWH Ticl/Clop GPIIb/IIIa*
60
40
20
0
*without PCI
Jul-Dec
1999
Jan-Jul
2000
Jul-Dec
2000
Jan-Jul
Year of Treatment
2001
Fox KAA et al. Eur Heart J 2003;24:1414-24.
Jul-Dec
2001
Temporal Trends STEMI:
Reperfusion
Lytics Primary PCI* No reperfusion
60
40
20
0
*within 12 h
Jul-Dec
1999
Jan-Jul
2000
Jul-Dec
2000
Jan-Jul
Year of Treatment
2001
Fox KAA et al. Eur Heart J 2003;24:1414-24.
Jul-Dec
2001
Temporal Trends NSTEMI:
In-hospital Therapies
LMWH Ticl/Clop GPIIb/IIIa
80
60
40
20
0
Jul-Dec
1999
Jan-Jul
2000
Jul-Dec
2000
Jan-Jul
Year of Treatment
2001
Fox KAA et al. Eur Heart J 2003;24:1414-24.
Jul-Dec
2001
GRACE Palm Pilot Software
In-hospital, 6-months
Death, Death/MI Prediction Model
GRACE PDA Software
GRACE PDA Software
At Admission Risk Model
At Discharge Risk Model
GRACE Publications
100%
80%
60%
40%
20%
0%
Abstract Acceptance Rate
(1999 to 2006)
Overall rate = 59%
Number of abstracts accepted = 94
77%
57%
43%
ESC ACC AHA
Manuscript Status
Published/in press
Provisionally accepted
Submitted
Being revised following submission
Edit/write assistance
Top priority independent
Medium priority
Low priority
1
5
7
7
7
8
12
0 10 20 30
46
40 50
GRACE Quarterly Reports to
Investigators
Quarterly Report
Current Quarter vs. Overall
Quarterly Report
Temporal Trends
Unique Features of GRACE
Multi-national perspective
Full spectrum of coronary syndromes
Increased data on demographics, presentation, management and outcome
Regular audits of data quality
Feedback to participating sites
6-month follow-up