Unit 22: Human Reproduction & Devlopment PowerPoint
advertisement

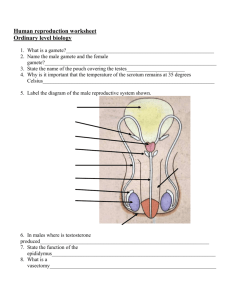
Human Reproduction Anatomy of the human male Main functions: The production of sperm, the male gametes; Spermatogenesis begins at puberty and continues until death; Delivery of functional sperm to the female reproductive system Anatomy of the human male Anatomy of the human male Production of Semen (a fluid comprised of): Sperm, which are expelled through the ducts during ejaculation (≈1% of semen volume); Glandular secretions that carry, nourish, and protect the sperm (mostly sugars & buffers) Testes (plural): Glands that produce sperm; located outside abdominal cavity within the scrotum Scrotum ≡ (saclike pouch ≈ 1-3°C below normal body temperature - sperm can only form at this lower temperature) How sperm leave the testes Seminiferous tubules: carries/stores sperm in testes Epididymis: a series of coiled ducts for maturation & temporary storage of sperm Vas deferens: tube which carries sperm past connecting lubricating and support glands How sperm leave the testes Lubricating and support glands: (a.) Seminal vesicles: secrete sugar-rich fluid that protects & nourishes sperm (b.) Prostate gland: produces an alkaline fluid that neutralizes both urine in the male urethra and the acidic environment of the vagina (c.) Bulbourethral glands: secrete fluids that lubricates the male urethra and allows easier coitus (intercourse) How sperm leave the testes Urethra: tube in the penis that transports semen out of the male’s body; also transports urine from the urinary bladder Penis: copulatory organ; transient tumescence Ejaculation: the release of semen through rhythmic contractions of smooth muscle in the Vas deferens Anatomy of the human male Anatomy of the human female Main functions: To produce the female gametes (ova); To receive sperm; To provide a suitable environment in which a fertilized ovum might develop during pregnancy Anatomy of the human female Anatomy of the human female Ovaries: Contain follicles that nurture ova; Produces sex hormones; Functional from puberty to menopause Anatomy of the human female Oviducts (Fallopian Tubes): Convey (move) ova towards the uterus; Muscular contractions & cilia draw ovum (egg) into oviduct; Location for fertilization to occur Anatomy of the human female Uterus (womb): Nourishes development of fertilized zygote; Opens into the vagina at cervix Vagina: Receives the penis during coitus; Forms the birth canal; Multiple layers of expandable smooth muscle; Potential, not defined, space Anatomy of the human female Anatomy of the human female Puberty Puberty: when secondary sexual characteristics develop and the potential for sexual reproduction is reached (sperm production or ovulation) Changes are controlled by hormones that initiate development of secondary sex characteristics; Primary sex characteristics are internal and external reproductive organs (genitalia) Puberty in males (♂) Secondary sex characteristics: Primary hormone: testosterone (testes); 2° Characteristics: increased hair (body, pubic, & facial), muscle development, deeper voice; Spontaneous ejaculation Puberty in females (♀) Secondary sex characteristics: Primary hormone: estrogen (ovaries); 2° Characteristics: breast development, broadened pelvis, distribution of body fat; increased hair (body & pubic); Menarche (onset of menstruation) Reproductive hormones Testosterone (♂ testes): Sperm production & secondary sexual characteristics Estrogen (♀ ovaries); Ova production, preparing uterus for fertilized zygote & secondary sexual characteristics Hormonal control of the testes Stimuli from other areas in the brain Androgens, (testosterone Hypothalamus most important), stimulate sperm production Releasing hormone They also maintain Negative Anterior feedback pituitary homeostasis by a negative feedback mechanism that inhibits FSH LH the secretion of FSH Androgen (follicle-stimulating production Testis Sperm hormone) and LH production (luteinizing hormone) Oogenesis: Production of ova Oogenesis occurs within the ovaries Lifetime supply of primary oocytes is present at birth that are ‘frozen’ in Prophase I One (maybe more) primary oocyte matures each menstrual cycle to form a secondary oocyte + polar body If the secondary oocyte is fertilized, it completes meiosis and becomes a haploid ovum + another polar body Oogenesis: Production of ova Ovum maturation in ovary releases progesterone maintains uterus lining produces estrogen Reproductive Cycle of the Adult Human Female A cyclical pattern of hormone secretion and reproductive events. Humans and many other primates have menstrual cycles. If implantation of a fertilized zygote does not occur, the endometrium (lining of uterus) is shed through the cervix and vagina in the process called menstruation. The Menstrual Cycle • The series of changes in the female reproductive system that includes producing an ovum and preparing the uterus for receiving it. • Once an ovum has been released during ovulation, the part of the follicle that remains in the ovary develops into a structure called the corpus luteum. • The menstrual cycle begins during puberty and continues for 30 to 40 years, until menopause. • At menopause, the female stops releasing ova and the secretion of female hormones decreases. The Menstrual Cycle • Divided into three phases: the flow phase, the follicular phase, and the luteal phase. • The timing of each phase of the menstrual cycle correlates with hormone output from the pituitary gland, changes in the ovaries, and changes in the uterus. Menstrual cycle 1. 2. 3. 4. LH Controlled by a complex interaction of 4 egg development hormones: follicle stimulating hormone (FSH); estrogen luteinizing hormone (LH); estrogen; progesterone Days 0 7 FSH ovulation = egg release corpus luteum progesterone lining of uterus 14 21 28 Menstrual cycle: Flow phase Day 1 of the menstrual cycle (1st phase) is the day menstrual flow begins. The shedding of blood, fluid, mucus, and epithelial cells that make up the endometrium (the internal lining of the uterus) begins. Contractions of the uterine muscles help expel the uterine lining and can cause discomfort in some females. The level of FSH in the blood begins to rise, and a follicle in one of the ovaries begins to mature as meiosis of the prophase I cell proceeds. Menstrual cycle: Follicular phase Follicular (2nd) phase lasts from about day 6 to day 14. As the follicle containing a primary oocyte continues to develop, it secretes estrogen, which stimulates the repair of the endometrial lining of the uterus. Day 14 ovulation occurs: Ovulation ≡ follicle enlarges and ruptures ovary wall; ovum is released to oviduct. Mittelschmerz: ovulation pain Menstrual cycle: Luteal phase Luteal (3rd) phase begins after ovulation (≈ day 15). Progesterone increases the blood supply of the endometrium. These changes correspond to the arrival of a fertilized ovum (zygote). If the ovum is not fertilized, the rising levels of progesterone and estrogen from the corpus luteum cause the hypothalamus to inhibit the release of FSH and LH. Menstrual cycle: Luteal phase Without fertilization, the corpus luteum degenerates and stops secreting progesterone or estrogen. As hormone levels drop, the thick lining of the uterus begins to shed. If fertilization occurs the endometrium begins secreting a fluid rich in nutrients for the embryo. Female reproductive cycle egg matures & is released (ovulation) estrogen builds up uterus lining Feedback corpus luteum ovary progesterone FSH & LH maintains uterus lining fertilized egg (zygote) HCG yes pituitary gland pregnancy GnRH hypothalamus no corpus luteum breaks down progesterone drops menstruation corpus luteum progesterone maintains uterus lining Female hormones FSH & LH released from pituitary gland; stimulates ova development & hormone release; peak release = release of ova (ovulation) Female hormones Estrogen released from ovary cells around developing ova; stimulates growth of lining of uterus; decreasing levels initiate menstruation Female hormones Progesterone released from corpus luteum in ovaries stimulates blood supply to lining of uterus; decreased levels sustains menstruation Hormonal coordination of the menstrual and ovarian cycles FSH (follicle stimulating hormone) produced by pituitary gland stimulates development of follicle LH (luteinizing hormone) stimulates the development of the corpus luteum; stimulates ovulation Hormonal coordination of the menstrual and ovarian cycles Estrogen: secreted by ovaries, stimulates development of uterine lining before implantation Progesterone: secreted by corpus luteum, maintains uterine lining during pregnancy Fertilization Fertilization is the union of a sperm and an ovum to form a diploid zygote. Fertilization results in a zygote and triggers embryonic development. Occurs normally inside of fallopian tube (oviduct). Fertilization is NOT pregnancy! (PATHWAY) Tens of millions of sperm enter the vagina cervix uterus oviducts (fertilization) sperm + ovum zygote 23(n) + 23(n) 46(2n) Fertilization Only one of the many millions of sperm entering the vagina will penetrate this human ovum to initiate fertilization Fertilization The shape of a human sperm cell is adapted to its function Sperm cell is enzymes, DNA & mitochondria! Multiple Fertilizations If two (or more) ova are released in the same cycle and fertilized fraternal siblings (different DNA) If one ova is fertilized and mitotically divides into two (or more) separate zygotes identical siblings (same DNA) Fertilization Implantation Implantation: The fertilized zygote implants into thickened uterine lining and the embryo starts to secrete the hormone human chorionic gonadotropin (HCG) (the hormone used for pregnancy tests) HCG keeps the corpus luteum functional and continuing to secrete progesterone. By the third or fourth month, the placenta takes over for the corpus luteum, secreting enough estrogen and progesterone to maintain the pregnancy. Implantation = Pregnancy! Embryonic Development Development: series of orderly, precise steps that transform a zygote into a multicellular embryo Embryo ≡ early development stages of a multicellular organism Includes: 1. cell division (mitotic) 2. cell growth 3. cell differentiation ≡ altering of unspecialized mitotic embryonic cells into specialized cells, tissues,& organs Early Embryonic Development Cleavage is the first major phase of embryonic development It is the rapid succession of cell divisions (Mitotic) It creates a multicellular embryo from the zygote NO growth Embryonic growth cannot occur until implantation occurs ZYGOTE Blastocoel BLASTULA Cross section of blastula (hollow ball) Early Embryonic Development Stages: 1. Morula ≡ solid ball of cells 2. Blastula ≡ single layer of cells surrounding a fluid-filled cavity called the blastocoel 3. NO growth; still dividing original single cell mass ZYGOTE Blastocoel BLASTULA Cross section of blastula (hollow ball) Embryonic Development Gastrulation is the second major phase of embryonic development The cells at one end of the blastula move inward Embryonic Development Organs start to form after gastrulation Embryonic tissue layers begin to differentiate into specific tissues and organ systems Embryonic Membranes Amnion ≡ fluid filled sac for protection Chorion Chorion ≡ will form the embryo’s part of the Amnion placenta Yolk sac Yolk sac ≡ produces first blood cells & germ cells Allantois Embryonic Membranes Allantois ≡ will form the umbilical cord (ropelike structure Chorion that attaches embryo Amnion to uterus) Umbilical cord brings Yolk sac nutrients in/wastes out of fetus Ties into hepatic artery & vein in fetus bellybutton Allantois The Placenta Placenta ≡ A growing fetus exchanges nutrients, oxygen, and wastes with the mother through the placenta Made of maternal and fetal tissues Substances pass both ways, but blood does not mix Placenta Nutrients, wastes, & gasses diffuse across capillaries Fetal Development Gestation is pregnancy It begins at implantation and continues until parturition (birth) ● Pregnancy in humans usually lasts about 280 days, calculated from the first day of the mother’s last menstrual period. Embryonic development of essential organs occurs in early pregnancy. The embryo may encounter risks from faults in its genes & from mother’s exposure to environmental factors. Human fetal development is divided into equal trimesters First trimester (0 to 3 months) The most rapid changes occur during the first trimester (most developmentally important)10 weeks 4 weeks 10 weeks 7 weeks eeks10 weeks 10 weeks Human fetal development is divided into equal trimesters Second trimester (4 to 6 months) Increase in size of fetus General refinement of human features 12 weeks Human fetal development is divided into equal trimesters The fetus spends much of the 2nd & 3rd trimesters just growing… …and doing flip-turns & kicks inside amniotic sac Week 20 Human fetal development is divided into equal trimesters 24 weeks (6 months; 2nd trimester) • Fetus is covered with fine, downy hair called lanugo • Its skin is protected by a waxy material called vernix Human fetal development is divided into equal trimesters Third trimester (7 to 9 months) 30 weeks (7.5 months) Human fetal development is divided into equal trimesters 32 weeks (8 months) The fetus sleeps 90-95% of the day & sometimes experiences REM sleep, an indication of dreaming Human fetal development is divided into equal trimesters Third trimester Growth and preparation for birth Provides time for maternal body to prepare for birth Nooo!!! I don’t want to go to Murdoch’s class! Three stages of labor Dilation of the cervix is the first stage Cervix starts at less than 1 cm dilation (open) and reaches full dilation at 10 cm Longest stage of labor (6-12 hours or longer; maybe MUCH longer!) Three stages of labor Expulsion is the second stage Period from full dilation of the cervix to delivery of the infant Uterine contractions occur every 2-3 minutes (positive feedback) Three stages of labor Expulsion is the second stage Mother feels urge to push down with her abdominal muscles Infant is forced down and out of uterus and vagina within a period of about 20 minutes Three stages of labor The delivery of the placenta is the final stage of labor Usually occurs within 15 minutes after the birth of the baby Some placenta’s are saved and frozen as they are a source of stem cells Labor & Birth: Positive Feedback positive feedback The end of the journey! And you think 9 months of Biology is hard! Lactation: the ‘mam’ in mammal • Lactation ≡ milk production • Lactation is another positive feedback system • Suckling stimulates the hypothalamus pituitary gland to release oxytocin • Oxytocin stimulates mammary glands to secrete milk • Continued suckling continues milk production Yes, males have mammary glands too! Growth and Aging Once a baby is born, growth and learning continue. Human growth varies with age and is somewhat gender dependent. Females develop earlier An adult ages As an adult ages, his or her body undergoes many distinct changes: -Slower metabolism -White hair -Thinner bones -Vision & hearing diminish