Hypertension in Pregnancy
advertisement
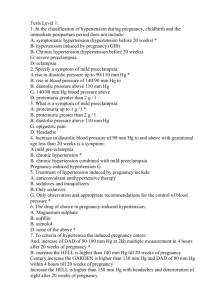
Obstetric Medicine (MDP) Workshop CSIM Annual Meeting, October 1, 2014 Hypertension, Cardiac Disease, Approach to Abnormal Liver Enzymes, VTE Dr. Paul Gibson (Calgary) – GIM & OB Internal Medicine Dr. Jonathan Windram (Edmonton) – Cardiology Dr. Rshmi Khurana (Edmonton) - GIM & OB Internal Medicine Dr. David Sam (Calgary) - GIM & OB Internal Medicine Audience Interaction Text response code to: 37607 Or use your web browser and go to: pollev.com/obmedcsim Hypertension in Pregnancy Paul S. Gibson, MD, FRCPC Associate Professor of Medicine and Obstetrics & Gynecology University of Calgary Recent Sources of Information ACOG, 2013 SOGC, 2014 What We Will Cover 1. Why hypertensive disorders in pregnancy (HDPs) matter 2. Preconception evaluation i. Risk factors for preeclampsia ii. Choice of medications 3. In-pregnancy evaluation i. Classification of HDPs ii. Pharmacologic treatment and BP targets 4. Postpartum evaluation i. Recognition and treatment of ‘postpartum preeclampsia’ ii. Implications of HDPs on women’s future health Why do hypertensive disorders in pregnancy (HDPs) matter ? Hypertensive disorders of pregnancy are a leading cause of maternal and fetal morbidity and mortality They are common (~10%): ~ 1% of pregnancies are complicated by pre-existing hypertension 5-6% of pregnancies result in gestational hypertension without proteinuria 2-4% of pregnancies result in pre-eclampsia * It can be expected that these numbers will increase given the trend towards an older and more obese obstetric population Maternal Mortality in Canada: Diagnoses associated with maternal deaths in Canada (excluding Quebec), 2002/03-2009/10. Canadian Institute for Health Information. Public Health Agency of Canada, 2011. http://www.phac-aspc.gc.ca Maternal Mortality due to HTN - USA Causes of Maternal Mortality in the UK: 2006-8 Centre for Maternal and Child Enquiries (CMACE). Saving Mothers’ Lives. BJOG 2011;118(Suppl. 1):1– 203. Saving Mothers’ Lives (2011) “It is disappointing that in this triennium … the single most serious failing in the clinical care provided for mothers with pre-eclampsia was the inadequate treatment of their systolic hypertension In several cases, this resulted in fatal intracranial haemorrhage Systolic hypertension was also a key factor in most of the deaths from aortic dissection” Case #1 23 y.o. woman, G0P0 Referred to her local General Internist for review re: HTN & proteinuria PMH: Uncontrolled HTN at age 13 Proteinuria – Bx = TBMD Ongoing anti-HTN meds since Home BP = 115-130 / 72-80 on lisinopril 10 mg/d Serum Cr = 105 Urine PCR = 40 mg/mmol, 24h urine = 500 mg/d Case #1 - continued Announces that she had just stopped her OCP, hoping to achieve pregnancy ASAP! Preconception Issues? Medication changes? Risks in pregnancy? Preeclampsia prevention? ACE-inhibitors in pregnancy Use in the 2nd & 3rd trimesters long known to cause fetal renal toxicity, leading to: oligohydramnios, IUGR, hypocalvaria, renal dysplasia, anuria, renal failure, and IUFD N Engl J Med 2006;354:2443-51 Infants exposed to ACE inhibitors in the first trimester were at increased risk for malformations of the: • cardiovascular system (risk ratio, 3.72) • central nervous system (risk ratio, 4.39) Concern that these finding were due to higher prevalence of undiagnosed DMII, rather than true medication effect What is this woman’s risk of developing preeclampsia? 1. 2% 2. 5% 3. 10% 4. 25% 5. 50% What is this woman’s risk of developing preeclampsia? Other risks of cHTN include IUGR, placental abruption, preterm delivery & prematurity Most of the morbidity and mortality are from preeclampsia What would you suggest to reduce her risk of preeclampsia? 1. Keep BP < 120/80 throughout 2. Fish oil supplements > 1000 mg/d 3. Maternal sodium intake < 2.0 g/d 4. Low-dose aspirin 5. Antioxidant vitamins (Vits C & E) Preeclampsia Prevention? SOGC Recommends (for women at increased risk): ASA 75-162 mg/d, taken at bedtime, started before 16 weeks GA and continued until delivery (for women at increased risk) Calcium supplementation (>= 1 g/d) Recommended for other established beneficial effects in pregnancy: abstention from alcohol, periconceptual use of a folate-containing multivitamin, and smoking cessation The following are not recommended: prostaglandin precursors, dietary salt restriction, calorie restriction in overweight women (during pregnancy), antihypertensive therapy specifically to prevent preeclampsia, and vitamins C and E WE GENERALLY recommend Vitamin D (1000-2000 IU/d) BP Monitoring Using Automated Devices in Pregnancy & Preeclampsia Due to altered hemodynamics in pregnancy, it is recommended that automated devices are validated specifically in pregnant women Further profound changes in hemodynamics can occur in pregnancies complicated by pre-eclampsia Some investigators have found large discrepancies between oscillometric devices and auscultation by observers, particularly in pre-eclampsia Devices for home BP monitoring? A comprehensive list of approved devices for HBPM can be found at: http://www.dableducational.org http://www.bhsoc.org/default.stm http://www.hypertension.ca/devices-endorsed-byhypertension-canada-dp1. What about home BP monitoring? A comprehensive list of approved devices for HBPM can be found at: http://www.dableducational.org http://www.bhsoc.org/default.stm http://http://hypertension.ca/en/hypertension/wha t-do-i-need-to-know/how-to-measure-my-bloodpressure/918-public/landing/249-devices-endorsedby-hypertension-canada Case #1 - continued Pt is switched to Labetalol 200 mg BID BP initially 140/90, then drops and remains ~ 130/80 Prenatal care arranged with an OB/GYN Periodic follow-up with GIM every 6-8 weeks At 31 weeks GA she is hospitalized with worsening HTN, despite labetalol 400 TID BPs exceeding 160/105 Hb=132, Plt=309, Cr=50, ALT=7, UA=380, LD=238 Repeat urine Prot:Cr = 234 mg/mmol (was 40) Diagnosis of HTN During Pregnancy HTN in pregnancy is defined as: SBP ≥ 140mmHg or DBP ≥90mmHg Severe hypertension is defined as: systolic BP of ≥ 160mmHg or a diastolic BP of ≥ 110mmHg * based on the average of at least two measurements, taken in the same arm at least 15 minutes apart What is “abnormal proteinuria” in pregnancy All pregnant women should be assessed for proteinuria Urinary dipstick testing may be used for screening for proteinuria when the suspicion of preeclampsia is low Proteinuria is highly suspect when urinary dipstick proteinuria is ≥ 1+ Proteinuria is defined as: Protein ≥ 30 mg/mmol urinary creatinine (0.03 g/mmol) in a spot urine (protein:creatinine) sample or ≥ 0.3g (300mg) in a 24-hour urine collection Classification of HTN in Pregnancy SOGC Preexisting hypertension -With Comorbid Conditions -With Preeclampsia Gestational hypertension -With Comorbid Conditions -With Preeclampsia Preeclampsia Other Hypertensive Effects Classification of HTN in Pregnancy: Co-morbid Conditions 1. Preexisting Hypertension 2. with Co-morbid Conditions Gestational Hypertension with Co-morbid Conditions Co-morbid conditions: • • Conditions such as type I or II diabetes mellitus and renal or vascular disease Strong indications for more aggressive antihypertensive therapy outside of pregnancy warrant special BP treatment thresholds and goals in pregnancy Classification of HTN in Pregnancy 1. Preexisting Hypertension 2. Gestational Hypertension 3. with Co-morbid Conditions with Pre-eclampsia with Co-morbid Conditions with Pre-eclampsia Preeclampsia Pre-eclampsia • Preeclampsia Gestational HTN PLUS New proteinuria, or One or more ‘adverse conditions’ or ‘severe complications’ • Gestational Hypertension with Pre-eclampsia New proteinuria, or One or more ‘adverse conditions’ or ‘severe complications’ Preexisting Hypertension with Pre-eclampsia Resistant hypertension (>2 drugs), or New or worsening proteinuria, or One or more ‘adverse conditions’ or ‘severe complications’ Severe Preeclampsia (SOGC) Pre-eclampsia complicated by one or more severe complications Severe preeclampsia is an indication to move to delivery (regardless of gestational age) What is your target BP (range) when treating HTN in pregnancy? 1. Anything less than 170/110 2. Less than 150/95 3. 130-155/80-105 4. 120-140/80-90 5. Less than 130/80 Pharmacologic Treatment Treatment of mild to moderate hypertension in pregnancy is controversial o Until recently, aggressive treatment has not been shown to improve major maternal and neonatal outcomes o There is concern that treatment of hypertension during pregnancy will impair fetal growth Pharmacologic Treatment Control of Hypertension In Pregnancy Study (CHIPS) International, multicentre (94 sites) RCT Women with chronic and gestational HTN Randomized to target diastolic BP of 85 vs. 100 mmHg Evaluating maternal and perinatal outcome Enrolled 1030 women Primary outcome: pregnancy loss or high level neonatal care for >48 h in the first 28d of life Secondary outcome: one/more serious maternal comps results not yet published, abstract only Arch Dis Child Fetal Neonatal Ed. 2014 Jun;99(Suppl 1):A5-A6. doi: 10.1136/archdischild-2014-306576.15. CHIPS – preliminary results 75% had pre-existing hypertension, 25% gHTN Women in 'less tight' (n=497) [vs. 'tight' (n = 490)] control had: higher mean dBP by 4.5 mmHg (95% CI 3.6, 5.4) similar rates of the primary (perinatal) outcome [31.4% vs. 30.7%; aOR 1.03] similar rates of secondary (maternal) outcome [3.7% vs. 2.0%; aOR 1.74]. Women receiving 'less tight' control more frequently developed BP ≥160/110mmHg (40.4% vs. 27.5%; aOR 1.78) 'Tight' control is safer for the mother, with no adverse effects for the baby Investigators: “A target dBP of 85mmHg should be aimed for” We should await the full published details before changing Rx Arch Dis Child Fetal Neonatal Ed. 2014 Jun;99(Suppl 1):A5-A6. doi: 10.1136/archdischild-2014-306576.15. Treatment of non-severe HTN (SOGC) For women without co-morbid conditions: For women with co-morbid conditions: drug therapy should be used to keep sBP at 130155mmHg and dBP at 80-105mmHg goal sBP < 140 mmHg and dBP at < 90 mmHg Initial therapy can be with one of a variety of antihypertensive agents: Methyldopa Labetalol Calcium channel blockers (nifedipine) Other beta-blockers (acebutolol, metoprolol, pindolol, and propranolol) Classification – our patient 1. Preexisting Hypertension with Co-morbid Conditions with Pre-eclampsia Resistant hypertension, or New or worsening proteinuria, or One or more ‘adverse conditions’ or “severe complications” Case # 1- continued In hospital x 6 days, antenatal steroids given BP initially controlled to < 160/100 with addition of Nifedipine XL (30mg BID) Seen Saturday morning BP = variable up to 180/115 Chest tightness and SOB onset overnight Orthopnea Sats 92% on room air JVP 3-4 cms, HR 130 with gallop, crackles Case # 1- continued CXR: ? Early interstitial changes Report: “low lung volumes, patchy opacities in lingula and LLL, likely related to atelectasis, pneumonia cannot be r/o” CT: No PE, interstitial/alveolar edema! Fetus doing OK BPs up to 180/115 !!! Treatment of Severe Hypertension (SBP >160 mmHg or DBP ≥110mmHg) Severe hypertension should always be treated to prevent acute end-organ damage BP should be promptly lowered to < 160 mmHg systolic and < 110 mmHg diastolic Initial therapy should be with: • Labetalol IV • Hydralazine IV • Nifedipine PO (capsules or PA tablets) Meds for Acute BP Lowering Agent Dosage Labetalol Start with 20mg iv; repeat 20-80mg iv q 30min, or 1-2 mg/min, max 300mg (then switch to oral) Nifedipine 5-10mg capsule to be bitten and swallowed, or just swallowed, every 30min 10mg PA tablet every 45min to a maximum of 80 mg/d Hydralazine Start with 5mg iv; repeat 5-10mg iv every 30min, or 0.5-10mg/hr iv, to a maximum of 20mg/hr iv (or 30mg IM) Case # 1- continued BP lowered to < 160/100 with IV labetalol Pulmonary edema = Severe Complication Decision to move to delivery! Poor fetal tolerance of labour induction C/S performed Neonatal respiratory distress – in NICU x weeks Mother and baby doing well in follow-up Case #2 • 37 y.o. African-Canadian woman, G2P2 • Uneventful pregnancy, no HTN or GDM, BPs ~ 110/70 • Induced vaginal delivery at 41 wks with epidural, sent home on PP day #2 • Progressive headache over 7 days postpartum • Taken to ER • Initial BP = 155/107 • Evaluated by MD, no labs • Given morphine, BP settled to 145/95 • Told she had a ‘migraine’ • Sent home with NSAIDs Case #2- continued • Returned to ER the next day, worse h/a, c/o visual deficits • Initial BP=170/115, • given morphine & IV labetalol x 3 • Labs: ALT 176, LD 398, 24hr U protein 1.62 g/day • Exam revealed L homonymous hemianopsia • CT head – small R occipito-parietal ICH • Admitted to Stroke service • BP controlled with nifedipine XL 60 OD • Remained on antihypertensives for 9 weeks • Aggressive rehab for vision and balance • At 9 weeks postpartum, mild visual defect remaining but otherwise normal (proteinuria resolved) Etiology of Postpartum HTN Up to 2/3 of women with postpartum preeclampsia had no HTN during pregnancy BMJ 2013;346:f894 doi: 10.1136/bmj.f894 Postpartum Preeclampsia - Symptoms Symptom Prevalence Headache 62-82 Visual Changes 19-31 Shortness of Breath/Chest Pain 13-30 Nausea 12.5-18 Vomiting 11.2-14 Abdominal Pain 7-14 Edema 9-10.5 Neurological Deficits 5.3 Al-Safi et al. Obstet Gynecol 2011;118:1102-7. Postpartum Preeclampsia - Labs • • • • • • • • Hemoconcentration (elevated Hg & Hct) Mild thrombocytopenia (plt 100-150 109/L) HELLP: hemolysis, transaminitis, thrombocytopenia Uric Acid >300 μmol/L Creatinine >70 μmol/L AST/ALT elevated LDH >235 U/L In & out cath for random urine Protein:Creatinine ratio (≥30 mg/mmol) ER Protocol Persistent Hypertension Postpartum Systolic ≥155 mmHg & 1 of (Symptoms/HTN within 4 weeks of delivery) Headache Visual changes SOB/CP Nausea/Vomiting Abdo pain Edema Neuro deficits Fast track to MD Assessment • detailed History & Physical • Labs: CBC, lytes, Cr, ALT, urate, LD, random U PCr • ECG, CXR Treat to sBP <155 mmHg • labetalol iv/PO or nifedipine fast then XL PP Preeclampsia &: Neurological Deficits PP Preeclampsia &: Pulm Edema/CP PP Preeclampsia &: HELLP MgSO4 infusion CT/CT-A Brain MRI Brain Troponins Echo Neuro/Stroke/ICU OB/MDP Cardio/MTU OB/MDP Full liver panel Including AST, Bili, BG q1h, DIC w/u If eclampsia/on Mag: ICU/OB to admit Cardio/MTU to admit OB/MTU to admit If stroke: Neuro to admit Avoid fluids Diuretic trial ACE-I OB to decide If MgSO4 *Supportive Care* If imaging N, no Mag: MTU to admit OB/MTU/MDP If worsening: -TTP/HUS -SLE -APAS -AFLP PP Preeclampsia &: Hypertension w/u for 2nd Cause HTN MTU/MDP MTU to admit (≥24 hrs) Postpartum Preeclampsia Be alert to this possible diagnosis, even if BP elevation not very ‘severe’ initially Most important to recognize and treat HTN Goal < 155/105 acutely, then < 140/90 Admit for observation for 24-48h and anticipate further worsening over first 7 days PP Avoid exacerbating with IVF and/or NSAIDs Does her HDP have future health implications for this woman? Evidence is accumulating that women who develop hypertensive disorders of pregnancy are at subsequent increased lifetime risk of vascular complications Two recent meta-analyses Bellamy et al. BMJ 2007;335:974-86. McDonald et al. AHJ 2008;156:918-30. Preeclampsia and Hypertension: RR = 3.7 Bellamy et al. BMJ 2007;335:974-86. Preeclampsia and Ischemic Heart Disease: RRs = 2.33 McDonald et al. AHJ 2008;156:918-30. Preeclampsia and Stroke RRs ≈ 2.0 McDonald et al. AHJ 2008;156:918-30. It is clear from a review of multiple recent studies that … Women with a history of preeclampsia have an increased risk for the later development of (RR): • HTN: 3.7 • IHD: 2.3 • Stroke: 2.0 • PVD: 1.9 • DVT: 1.2 • CV Death: 2.3 • Death: 1.5 Risk of Future CVD is Proportional to Timing/Severity of Preeclampsia McDonald et al. AHJ 2008;156:918-30. Chicken vs Egg Is the preeclampsia a CAUSE OF increased systemic vascular risk, or is the preeclampsia a RESULT OF an underlying systemic vasculopathy (unmeasured ?) CHAMPS study: Link with Metabolic Syndrome • CHAMPS identified higher risk of future CVD in women with a MATERNAL PLACENTAL SYNDROME who develop elements of metabolic syndrome (obesity, HTN, DM, dyslipidemia) • 1-2 features: AHR = 4.5 • 3-4 features: AHR = 11.7 Ray et al. Lancet 2005;366:1797-803. CV Risk with MPS and features of Metabolic Syndrome History of preeclampsia/MPS adds to CV Risk of traditional CV Risk Factors Some women who experience a HDP also have (or develop) features of the METABOLIC SYNDROME (obesity, hypertension, diabetes, dyslipidemia) Women with these features are at MUCH HIGHER risk of vascular complications How does this all tie together? Microvascular dysfunction, metabolic disturbance, endothelial dysfunction and inflammation play a role in the pathogenesis of preeclampsia similar to the pathogenesis of atherosclerosis Preeclampsia and subsequent cardiovascular disease may both be manifestations of the metabolic syndrome Women who have a predisposition for the metabolic syndrome are more likely to: • develop preeclampsia during pregnancy • subsequently develop clinically evident hypertension, obesity, atherosclerosis and type 2 diabetes • eventually develop CV disease Pregnancy is a metabolic stress test Powe et al. Circulation 2011;123:2856-2869. Can preeclampsia cause an increased risk of vascular complications? MAYBE Shared risk factors, but: • Risk of complications is higher in women following preeclampsia than in women simply sharing the same metabolic risk factors • It appears that changes in vascular endothelial function can “outlive” the preeclamptic event This is an important point for preconception counseling regarding subsequent pregnancies Population at Risk Women who have experienced an (early/severe) preeclamptic pregnancy are an at risk population who may benefit from primary prevention regarding modifiable CV risk factors Primary Prevention Strategies To Consider Following Preeclampsia • Weight control/exercise programs • Return to pre-pregnancy weight / BMI<25 • Hypertension screening/monitoring and treatment • Smoking cessation • Diabetes screening • Lipid monitoring +/treatment Conclusions Hypertensive disorders of pregnancy are common, and remain an important cause of maternal morbidity and mortality Limited options for preeclampsia prevention in high-risk women ASA and Calcium (+/- Vit D) in high-risk women Proteinuria Dipstick = screen (≥ 1+) Diagnosis: Urine protein: Cr ratio (≥ 30 mg/mmol Cr) 24-hour collection (≥ 0.3 g/24h) Conclusions HTN in Pregnancy is SBP >= 140 and/or DBP >= 90 mmHg but treatment target is wide (130-155/80-105) Results from CHIPS may change practice/targets Preeclampsia may present/worsen within the first week postpartum Recognition and prompt BP lowering is critical Women with a history of preeclampsia have increased risk for vascular disease and chronic renal disease later in life Opportunity for counseling, screening and possibly enhanced primary prevention of CVD THANK YOU for your time and attention! Questions during the Panel Discussion