Overview of Calcium and Phosphate 4
advertisement

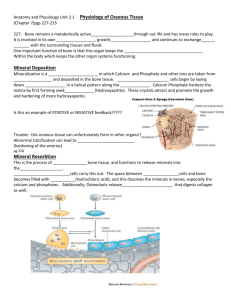
Overview of Calcium and Phosphate Regulation in the Extracellular Fluid and Plasma Dr. Shafali Singh Objectives • Explain primary physiological actions of calcium and phosphate. • Understand the importance of maintaining homeostasis of bodily calcium and phosphate concentrations, and how this is accomplished. • Describe the bodily pools of calcium, their rates of turnover, and the organs that play central roles in regulating movement of calcium between stores. • Define the basic anatomy of bone. • Delineate cells and their functions in bone formation and resorption Calcium • Calcium plays a key role in many physiologic processes, • contraction of skeletal, cardiac, and smooth muscles; blood clotting, transmission of nerve impulses etc • 0.1% –ECF • 1 %- inside CELLS • 99%-BONES Plasma Ca : 9.4mg% Phosphate Phosphate have role in ATP formation, act as biological buffers, modifiers of protein. • <1 %-ECF . • 14 to 15 %-inside cells, • 85 %- bones, Plasma Phosphate: 3-5 mg% Inorganic phosphate in the plasma is mainly in two forms: HPO4- and H2PO4- • Plasma calcium represents 45% ionized free, 40% attached to protein, 15% associated with anions such as phosphate and citrate. • The free calcium is the physiologically active and precisely regulated form. • The most accurate determination of free calcium is via a calcium-selective electrode Factors that may alter the ionized Ca2+concentration 1. Acid-base abnormalities alter the ionized Ca2+ concentration by changing the fraction of Ca2+ bound to plasma albumin. 1. Changes in plasma protein concentration: 3. Changes in anion concentration alter the ionized Ca2+ concentration: Non-Bone Physiologic Effects of Altered Calcium Concentrations in the Body Fluids • Hypocalcemia Causes Nervous System Excitement and Tetany. Signs and Symptoms of Hypocalcemia • Extensive spasms of skeletal muscle, involving especially the muscles of the extremities and the larynx. Neurol Trousseau’s (carpopedal spasm) Chvostek’s (CN VII spasm) Paresthesias Lethargy, seizures Respiratory arrest Cardio Heart block, CHF Derm Dry skin, brittle hair Trousseau’s (carpopedal spasm) Symptoms of tetany appear at higher total calcium levels if the patient hyperventilates, thereby increasing plasma pH. Plasma proteins are more ionized when the pH is high, providing more protein anion to bind with Ca2+. • Hypercalcemia Depresses Nervous System and Muscle Activity Signs and Symptoms of Hypercalcemia • If calcium is > 12 mg/dl, one may see: Neurol Lethargy, confusion, coma Psych Depression, psychosis Cardiol decreases the QT interval of heart Nephrol nephrolithiasis (>17mg/dl) GI Nausea/emesis, anorexia Constipation, Intestinal Absorption and Fecal Excretion of Phosphate • Except for the portion of phosphate that is excreted in the feces in combination with non absorbed calcium, almost all the dietary phosphate is absorbed into the blood from the gut and later excreted in the urine. • Phosphate excretion by the kidneys is controlled primarily by an overflow mechanism : When less than this amount of phosphate is present in the glomerular filtrate, essentially all the filtered phosphate is reabsorbed. When more than this is present, the excess is excreted. Relationship Between Calcium and Phosphate • Whether calcium and phosphate are laid down in bone (precipitate from solution) or are resorbed from bone (go into solution) depends on the product of their concentrations rather than on their individual concentrations. • When the product exceeds a certain number (solubility product or ion product), bone is laid down: [Ca2+] x [P04] > solubility product = bone deposition Relationship Between Calcium and Phosphate • Under normal conditions the ECF product of calcium times phosphate is close to the solubility product. • Thus, an increase in the interstitial fluid concentration of either Ca2+ or phosphate increases bone mineralization. • For example, • an increase in plasma phosphate would increase the product of their concentrations, promote precipitation, and lower free calcium in the interstitial fluid. • A malignant increase in the concentration of calcium or phosphate due to chronic renal disease or rhabdomyolysis can cause the precipitation of calcium phosphate within tissues. • When the product is below the solubility product, bone is resorbed: [Ca2+]x [P04] < solubility product = bone resorption • Thus, a decrease in the interstitial concentration of either Ca2+ or phosphate promotes the resorption of these salts from bone (demineralization). • For example, a decrease in plasma phosphate alone would promote bone demineralization. Increasing renal excretion of phosphate would promote bone demineralization and a rise in interstitial free calcium. BONE PHYSIOLOGY Bone is involved in overall Ca2+ and PO43– homeostasis. It protects vital organs, and the rigidity it provides permits locomotion and the support of loads against gravity Bone formation: Bone is a special form of connective tissue with a collagen framework impregnated with Ca2+ and PO43– salts, particularly hydroxyapatites Mechanism of Bone Calcification Secretion of collagen molecules and ground substance by osteoblasts collagen fibers form;the resultant tissue becomes osteoid, Ground substance is an amorphous, gel-like matrix of glycosaminoglycans, proteoglycans, glycoproteins, salts, and water that fills the space between cells in all tissues. Bone ground substance is saturated with Ca2+ and PO4- . OSTEOID The combination of colla-gen fibrils and ground substance is called osteoid Initial calcium salts to be deposited are amorphous compounds (noncrystalline), then by a process of substitution and addition of atoms, or reabsorption and reprecipitation, these salts are converted into the hydroxyapatite crystals (Crystal Seeding) • Maturation few per cent salt may remain permanently in the amorphous form. These amorphous salts can be absorbed rapidly when there is need for extra calcium in ECF • Bone contains a type of exchangeable calcium that is always in equilibrium with the calcium ions in the extracellular fluids. • This amounts to 0.4% to 1% of the total bone calcium. • This calcium is deposited in the bones in a form of readily mobilizable salt such as CaHPO4 and other amorphous calcium salts. • Exchangeable calcium is that it provides a rapid buffering mechanism • Hydroxyapatite Does Not Precipitate in Extracellular Fluid Despite Supersaturation of Calcium and Phosphate Ions. inhibitor pyrophosphate • Precipitation of Calcium in Nonosseous Tissues Under Abnormal Conditions:Arterial wall, degenerating tissue, old blood clot REMODELLING OF BONE Is a continuous process BONE CELLS: Osteocytes, Osteoblasts and Osteoclasts Osteocytes & Osteoblasts: Bone deposition Osteoclasts: Bone absorption Is In equilibrium Importance of Remodelling of Bone 1. 2. 3. To adjust the strength: proportionate to degree of bone stress Shape of the bone can be rearranged – repair of fracture Old bones are replaced by new bones Causes of Bone remodeling 1. Mechanical Stress 2. Microdamage( Microfissures and microscopic cracks) 3. Hormones-parathyroid hormone [PTH] from the parathyroid gland and calcitonin from the thyroid) and by vitamin D. Remodeling Sequence 1. Activation Weight-Bearing Stress • Though poorly understood, weight-bearing mechanical stress increases the mineralization of bone. • The absence of weight-bearing stress (being sedentary, bedridden, or weightless) promotes the demineralization of bone. • Under these conditions, the following occurs: Plasma Ca2+tends to be in the upper region of normal. Plasma PTH decreases. Urinary calcium increases Indices can be utilized to detect excess bone demineralization and remodelling Resorption • C-telopeptide (C-terminal telopeptide of type 1 collagen (CTx)) • Collagen cross-links (PYD,DPD) • Tartrate-resistant acid phosphatase (TRAP) • Hydroxyproline (OHP) • Hydroxylysine-glycosides (Hyl-Glyc) • Bone Sialoprotein (BSP) • Gamma Carboxyglutamin acid (GLA) Bone formation • P1NP (Procollagen type 1 N-terminal propeptide) • Bone-specific alkaline phosphatase (ALP) • B-ALP • Osteocalcin (bone gla protein) Osteoporosis—Decreased Bone Matrix • most common of all bone diseases in adults, especially in old age. • Diminished organic bone matrix. • causes of osteoporosis• (1) lack of physical stress on the bones because of inactivity; • (2) malnutrition to the extent that sufficient protein matrix cannot be formed; • (3) lack of vitamin C, • (4) postmenopausal lack of estrogen secretion • (5) old age, in which growth hormone and other growth factors diminish greatly. (6) Cushing’s syndrome, Parathyroid hormone(Parathormone) • PTH is released from parathyroid glands in response to a decline in circulating Ca2+ and Mg2+ levels. PTH actions are geared toward increasing Ca2+ availability. Regulation of secretion • In most cells exocytosis depends on a rise in intracellular free calcium. • In the parathyroids that role is taken by magnesium. • Depletion of magnesium stores can create a reversible hypoparathyroidism • Clinical correlation:• Lithium sensitizes the Ca2+ receptor to changes in plasma Ca2+, causing increased PTH release in response to a given Ca2+ stimulus. This is the reason why bipolar patients on lithium salts for manic episodes can also have hypercalcemia PARATHYROID HORMONE-RELATED PEPTIDE • PTHrP is a paracrine factor secreted by many tissues; e.g., lung, mammary tissue, placenta. • The majority of humoral hypercalcemias of malignancy are due to over-expression of PTHrP. • PTHrP has a strong structural homology to PTH and binds with equal affinity to the PTH receptor. Actions on bone, kidney and intestine KIDNEY PTH increases reabsorption of calcium & reduces reabsorption of phosphate. increases the rate of reabsorption of magnesium ions and hydrogen ions while decreases the reabsorption of sodium, potassium, and amino acid Net effect of its action is increased calcium & reduced phosphate in plasma BONES Increases Calcium and Phosphate Absorption from the bone RAPID PHASE (min) SLOW PHASE (days-weeks) INTESTINE Increases calcium reabsorption via vitamin D Actions of PTH • Rapid actions of PTH – PTH increases Ca2+reabsorption in the distal tubule of the kidney and decreases phosphate reabsorption in the proximal tubule. By decreasing renal phosphate reabsorption, PTH lowers plasma phosphate. This causes the product of the Ca2+and phosphate concentrations to be less than the solubility product. This, in turn, promotes the resorption of these ions from bone and raises their concentration in the circulating blood. Slower actions of PTH • PTH slowly increases the formation and activity of osteoclasts, which resorb bone, releasing Ca2+. • PTH increases the formation of 1,25 di-OH D3 (active vitamin D) in the proximal tubules of the kidney, which leads to increased absorption of Ca2+and phosphate from the small intestine. skin 7- dehydrocholesterol diet uv Vita D induced incr synt of proteins--role in small intestine Vit D binds to nuclear Vitamin D receptor that complexes with an RXR and induces transcription from the Vit D response elements. Role of vitamin D GI Stimulates GI absorption of calcium Promotes Phosphate Absorption by the Intestines. Effects of vitamin D Kidney (weak Decreases Renal Calcium and Phosphate Excretion. effect) Bones The resulting high concentrations of Ca2+and phosphate in the extra-cellular fluid exceed the solubility product, and precipitation of bone salts into bone matrix occurs. At abnormally high activity levels Vit D increases bone resorption and release of Ca2+and phosphate from bone. Receptors for 1,25 di-OH D3are on the nuclear membranes of osteoblasts. Through communication from osteoblasts, activated osteoclasts carry out the bone resorption. Rickets—Vitamin D Deficiency • lack of 1,25-(OH)2D3 can result from • low exposure to sunlight, • lack of access to dietary sources of vitamin D or • a genetic disorder pro-ducing a low functioning 25(OH)D1-alpha-hydroxylase. Rickets—Vitamin D Deficiency • Vitamin D deficiency results in calcium or phosphate deficiency in the ECF. • The plasma Ca concentration in rickets is only slightly depressed, but the level of PO4 is greatly depressed. • Rickets Weakens the BonesCompensatory PTH activity causes – osteoclastic absorption of the bone, progressively weaker bones Rapid osteoblastic activity osteoblasts lay down large quantities of osteoid, which does not become calcified. Chest X – RAY showing promient costochondral joints bilaterally - a "Rachitic Rosary." Osteomalacia—“Adult Rickets” • • • • Causedietary deficiency steatorrhea (failure to absorb fat) because vitamin D is fat-soluble and calcium tends to form insoluble soaps with fat. Renal rickets congenital hypophosphatemia, vitaminD– resistant rickets. Excess vitamin D • • • • Raises plasma Ca Secondary hypoparathyroidism Phosphates levels rise Bone resorption and bone mass decrease Exposure to UV light directly facilitates which of the following? A) Conversion of cholesterol to 25hydroxycholicalciferol B) Conversion of 25-hydroxycholicalciferol to 1,25- dihydroxycholicalciferol C) Transport of calcium into the extracellular fluid D) Formation of calcium binding protein E) Storage of vitamin D3 in the liver Calcitonin • Calcitonin is a peptide hormone secreted by the parafollicular or “C” cells of the thyroid gland • It is synthesized as the preprohormone & released in response to high plasma calcium. • Calcitonin acts on bone osteoclasts to reduce bone resorption. • Net result of its action is a decline in plasma calcium & phosphate • Calcitonin is useful in the treatment of Paget’s disease. • Calcitonin is not a major controller of Ca2+ in humans. Removing the thyroid (with the C cells) or excess of calcitonin via a C cell tumor (medullary carcinoma of the thyroid) has little impact on plasma calcium. Summary • PTH & calcitonin release are regulated by plasma Ca levels • Bone Ca & phosphate serve as a ready reserve for maintenance of plasma levels • Bone, kidney & intestine participate in the regulation of plasma calcium • PTH, Vitamin D, & calcitonin balance plasma [Ca++] conc Effects of Other Hormones & Humoral Agents on Calcium Metabolism Positive Ca balance Negative Ca balance • Growth hormone • Insulin • Insulin-like growth factor I (IGF-I) • Estrogen • Glucocorticoids • Thyroid hormones Q. A patient with parathyroid deficiency 10 days after inadvertent damage to the parathyroid gland during thyroid surgery would probably have? a) Low plasma phosphate and calcium levels and tetany b) Low plasma phosphate and calcium levels and tetanus c) A low plasma calcium level, increased muscular excitability and a characteristic spasm of the muscles of the upper extremity. d) High plasma phosphate and calcium levels and bone demineralization e) Increased muscular excitability ,a high plasma calcium level ,bone demineralization Q. Which of the following is not involved in regulating plasma calcium levels? a. b. c. d. e. Kidney Skin Liver Lungs intestine Q. 1,25dihydroxycholecalciferol affects intestinal calcium absorption through a mechanism thata) b) c) d) e) Includes alteration in the activity of genes Activate adenyl cyclase Decrease cell turnover Change gastric acid secretion Is comparable to the action of polypeptide hormone Q. Which of the following would you expect to find in a patient whose diet has been low in calcium for 2 months? a) Increased formation of 24,25dihydroxy cholecalciferol b) Decreased amount of calcium binding protein in intestinal epithelial cells c) Increased parathyroid hormone secretion d) A high plasma calcitonin concentration e) Increased plasma phosphates PATHOPHYSIOLOGY OF PARATHYROID HORMONE PATHOLOGIC DISORDERS • HYPERPARATHYROIDISM primary Secondary ( as compensation for hypocalcemia) • HYPERVITAMINOSIS D 1.Primary Hyperparathyroidism • Cause - tumor of one of the parathyroid glands. • 80% due to a single parathyroid adenoma • Extreme osteoclastic activity in the bones • Increased plasma alkaline phosphatase, osteocalcin and increased excretion of cAMP (second messenger for PTH in the kidney), and hydroxyproline. Effects of Hypercalcemia in Hyperparathyroidism • Plasma Ca level to rise to 12 to 15 mg/dl and, rarely, even higher. • Elevated Ca levels, cause • depression of the central and peripheral nervous systems, • muscle weakness, • constipation, abdominal pain, peptic ulcer, lack of appetite, • depressed relaxation of the heart during diastole. Metastatic deposition of calcium • calcium and phosphate in the body fluids become greatly supersaturated. • calcium phosphate (CaHPO4) crystals begin to deposit in the alveoli of the lungs, the tubules of the kidneys, the thyroid gland, the acidproducing area of the stomach mucosa, and the walls of the arteries. Related causes of hypercalcemia • Lithium shifts the sigmoid Ca/PTH curve to the right. Higher calcium levels are thus needed to suppress PTH. A rare familial defect which reduces the Ca receptor sensitivity in a similar way results in hypercalcemia. • Sarcidosis and other granulomatous disorders (10%) due to increased activity of vitamin D • Thyrotoxicosis, milk-alkali syndrome II. Secondary Hyperparathyroidism • High levels of PTH occur as compensation for hypocalcemia . • Caused by vitamin D deficiency or chronic renal disease in which the damaged kidneys are unable to produce sufficient amounts of the active form of vitamin D(1,25dihydroxycholecalciferol). Differential diagnosis and treatment • Elevated plasma calcium and PTH normal or elevated; conclusion is primary hyperparathyroidism • Elevated plasma calcium and decreased PTH; conclusion is something other than primary hyperparathyroidism • Treatment is usually surgery; i.e., removing the adenoma or with hyperplasia removing most of the parathyroid tissue. Hypoparathyroidism • With insufficient PTH, the osteocytic reabsorption of exchangeable Ca decreases and the osteoclasts become almost totally inactive. • Commonest cause is -thyroidectomy, the Ca level in the blood falls from the normal of 9.4 mg/dl to 6 to 7 mg/dl within 2 to 3 days, and the blood phosphate concentration may double. • Signs of tetany develop. Management: • Administration of extremely large quantities of vitamin D, along with intake of 1 to 2 grams of calcium, keeps the calcium ion concentration in a normal range. • Treatment with PTH less effective. Additional causes of hypocalcemia Acute hypocalcemia can occur even with intact homeostatic mechanisms. • Included would be alkalosis via hyperventilation, transfusions of citrated blood, rhabdomyolysis or tumor lysis, and the subsequent hyperphosphatemia • Hyperphosphatemia of chronic renal failure • Congenital absence of parathyroids rare (DiGeorge’s syndrome) Parathyroid hormone directly A) controls the rate of 25hydroxycholicalciferol formation B) controls the rate of calcium transport in the mucosa of the small intestine C) controls the rate of formation of calcium binding protein D) controls the rate of formation of 1, 25dihydroxycholicalciferol E) stimulates renal tubular phosphate reabsorption A 40-year-old woman comes to the emergency room with a fracture in the neck of the femur. Radiographs reveal generalized demineralization of the bone in the area. Her plasma calcium ion concentration is significantly greater than normal: 12.2 mg/dL. Which of the following conditions is consistent with this presentation? A) Osteoporosis B) Rickets C) Hyperparathyroidism D) Renal failure The function of which of the following is increased by an elevated parathyroid hormone concentration? A) Osteoclasts B) Hepatic formation of 25hydroxycholecalciferol C) Phosphate reabsorptive pathways in the renal tubules D) All of the above A sustained program of lifting heavy weights will increase bone mass. What is the mechanism of this effect of weightlifting? A) Elevated metabolic activity stimulates parathyroid hormone secretion B) Mechanical stress on the bones increases the activity of osteoblasts C) Elevated metabolic activity results in an increase in dietary calcium intake D) Elevated metabolic activity results in stimulation of calcitonin secretion Extracellular calcium concentration remains only slightly below normal for many months even when dietary calcium intake is minimal. What accounts for this ability to maintain calcium concentration in the extracellular fluid? A) Only a slight reduction in plasma calcium concentration stimulates large, sustained increases in parathyroid hormone secretion B) Osteoclasts stimulated by high levels of parathyroid hormone remove calcium from the large quantity stored in the bone, thereby maintaining the nearnormal extracellular calcium level C) Renal excretion of calcium is greatly reduced under the influence of high concentrations of parathyroid hormone D) All of the above