Dr. Ndugga Baker Maggwa
advertisement

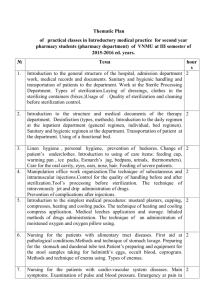
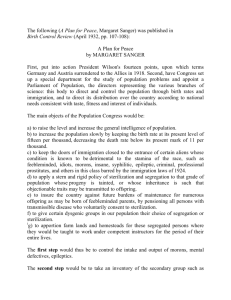
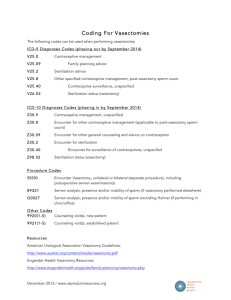
Ligation, excision, occlusion, oh my!: Recent research for expanding access to permanent methods of contraception Presentation to the RESPOND Research Working Group Dr Maggwa Baker Ndugga PROGRESS Project Director March 18, 2010 Presentation Outline I. II. III. IV. Programmatic/Operations Research New methods and techniques Research opportunities Questions Context • Female sterilization one of the most commonly used methods globally, but underutilized in many developing countries, including Sub-Saharan Africa • Male sterilization also underutilized in Sub-Saharan Africa • Male and female sterilization are among the most costeffective contraceptive methods available • Continuing efforts for non-surgical options Cost-effectiveness of LA/PMs 13 FP/RH Tier One Countries $16.00 $12.00 $10.00 $8.00 $6.00 $4.00 $2.00 on pl an Im lle de Ja M PA D O C C M PA D G en m St er Fe p Si no Im r eS te M al D $0.00 IU Service Delivery Cost/CYP $14.00 Female Sterilization Photo from: Minilaparotomy For Female Sterilization: An Illustrated Guide for Service Providers. EngenderHealth: 2003. Contraceptive Use Among Married Women 15-49, Female Sterilization (%) Source: Population Reference Bureau http://www.prb.org/Datafinder/ Programmatic Evidence • Interval sterilizations are more common than postpartum sterilizations in many countries located in North Africa, Sub-Saharan Africa, and South Asia. In contrast, postpartum sterilizations are more common in some countries in Latin America and the Caribbean. • Prevalence of female sterilization and the age at which women obtain a sterilization are inversely related: In countries where prevalence is high, the median age is generally low, while in low-prevalence countries, women often are not sterilized until older ages. • Mini-lap can be provided by a range of providers (physicians, clinical officers, nurse-midwives) with surgical skills and training and in health centers with basic surgical capacity (including via outreach teams) Can Nurses provide surgical contraception? Physician (N=279) Nurse (N-54) Surgical Difficulties 2.2 3.1 Tubal Injuries 0.4 0.2 1 year follow up (pain at incision site, adenexial pain, hardening of scar, vaginal bleeding) 3.9 4.4 Complications requiring hospital admission 0.8 0.4 Complication Source: International Family Planning Perspectives, Vol.6 No2, June 1990. Post Partum Sterilization by Nurse Midwives in Thailand Issues of acceptability and access • Common factors linked to regret: – Age at sterilization – family size – number of male offspring – timing of sterilization • Reasons for choosing FS =achieved desired family size, economic concerns • Barriers to accessing FS may include restrictive policies (age, parity, spousal consent), provider bias, lack of knowledge among potential clients Vasectomy Photo by D. Shattuck, February 2010 Rwanda Contraceptive Use Among Married Women 15-49, Male Sterilization (%) Source: Population Reference Bureau http://www.prb.org/Datafinder/ Programmatic Evidence • Success rates can vary depending on the skill of the surgeon and technique used. • Vasectomy can be performed safely and effectively by junior level doctors. • Many health care professionals in developing countries are not knowledgeable about vasectomy. • Culturally relevant counseling, including a discussion of culturally relevant motivators, is important for successful promotion • A mass media campaign in Ghana promoting vasectomy was successful in increasing demand and uptake Issues of acceptability and access FHI/EngenderHealth qualitative research in Kigoma, Tanzania (2004) • Six themes contributing to the vasectomy decision-making process: – Economics – spousal influence – Religion – provider reputation and availability – uncertainty about the future poor vasectomy knowledge and understanding FHI/EngenderHealth qualitative research in Uttar Pradesh, India (2007) • Barriers = misconceptions/misinformation among potential clients, lack of trained providers • Reasons for choosing NSV=did not want spouses to undergo FS, spouses could not undergo FS Revitalizing Vasectomy in Rwanda • Building on training in NSV done by IntraHealth Capacity Project • February 2010: FHI supported TOT for 3 physicians in cautery and FI – 3 districts, 5 days, 5 health centers, 67 vasectomies performed—more men came than could be operated – Time of procedure improved from 20 minutes to 10 minutes over 5 days – Reasons for seeking vasectomy: • Financial challenges of large families • Side effects of hormonal methods (wives) • Possibly the first-time cautery introduced in natl programs in Africa Photo by D. Shattuck, February 2010 Rwanda New and emerging technologies At least 55 near-, mid-, and long-term options exist in global contraceptive pipeline Development projects Discovery projects Early Development (Pre-clin, Ph1, Ph2) Late Development (Ph3) Developing world registration / Launch • GnRH II receptor antagonists • • • • • • Estetrol + Progestin OC LNG butanoate Ulipristal Vaginal Ring Nestorone/E2 Vaginal Ring Nestorone/E2 gel or spray Single-rod gestodene implant • • • • • • • DMPA + Uniject Nestorone/EE Vaginal Ring Gestodene and EE Patch ellaOne BufferGel Generic LNG IUS LNG as pericoital OC • • • • • PC6-inhibitor • LIF and IL-11 • SGK1/AKT • • • • Meloxicam β-hCG Erythromycin sterilization Polidocanol sterilization • • • • SILCS Diaphragm Quinacrine pellets PATH woman's condom C31G (spermicide) • • • • • Faslodex • SARMS • • • • TU + ENG MENT DMAU Oral testosterone • • • • TU TU + NET-EN DMPA + TU Desogestrel + Testosterone • • • • • • • • • • • • BDADs Carica papaya extract Testicular ultrasound HIFU (High intensity focused ultrasound) • RISUG Hormonal Non-hormonal Male Horm Non-horm. Female Discovery (Target ID, proof-of-principle) Post-development Eppin RAR antg'nists CatSper α-adrenoreceptor GAPDHS Adjudin TEX14 H2-Gamendazole Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 Sino-implant (II) Cyclofem Ortho Evra Progesterone Only Vaginal Ring • Femilis IUS Reddy latex FC Centchroman Female Condom 2 (FC2) Essure New Technologies— Female Non-surgical Sterilization • Essure • Quinacrine • Erythromycin • Polidocanol Essure Conceptus, Inc. Product: Essure Delivery: Tubal occlusion through bilateral fallopian tube micro-insert (PET) Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Sterilization Female Non-hormonal Long-acting Regulatory TBD 2010-2012 $1300 - once Advantages / value proposition: • Non-surgical permanent female sterilization contraceptive option for females • Highly effective method; 5-year data show an efficacy rate of 99.74% with proper protocol / compliance • Few adverse events, especially when compared with traditional methods requiring abdominal incision Risks / challenges: • Requires sophisticated HC infrastructure as well as training to administer device as well as an clinician who is experienced in hysteroscopy and has received company approved training • Requires follow-up hysterosalpingography (HSG) to ensure device was properly inserted per US label, but outside the US some physicians use ultrasound to confirm proper placement • Patient must use other contraceptive methods for initial 3 months until tubal occlusion is achieved • Currently, procedure costs $1300 in United States • Procedure is non-reversible Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 Quinacrine Non-surgical Female Sterilization Regimen: Seven 36mg quinacrine hydrochloride inserted twice into endometrial cavity one month apart. Applicability: Non‐surgical female sterilization method which can be performed in low‐resource settings at low cost. Quinacrine pellets FHI Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Sterilization Female Non-hormonal Long-acting Phase III TBD 2014-2016 $1 Advantages / value proposition: • Non-surgical female sterilization method which can be performed in low-resource settings at low cost • Some studies have shown low failure rate when performed by trained provider – However, published pregnancy rates vary considerably; 4.3% to 12.1% for 10-year cumulative pregnancy probabilities • Estimated at least 140,000 women in 34 countries have undergone procedure as method of non-surgical sterilization • Recent follow-up of 1,492 Chilean women found rates of cancer amongst women exposed to intrauterine quinacrine similar to population-based rates • A case control study of gynecological cancers in 12 provinces in Northern Vietnam also found no relationship between quinacrine use and cancer Risks / challenges: • Quinacrine as a method of non-surgical sterilization has not been approved by any regulatory body • Concerns about long-term safety profile, including potential risk of cancer – Currently available genetic toxicity data are sufficient to support quinacrine is genotoxic in vitro – Studies in mice found a dose-related increase in incidence of both benign and malignant tumors of the vagina, cervix, and uterus • Expert panel convened by WHO recommended to reevaluate quinacrine once additional retrospective safety data is available • Buffett Foundation concluded method was not worth pursuing after funding safety studies and analyzing findings Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 Erythromycin Non-surgical Sterilization Family Health International Product: Erythromycin lactobionate Delivery: Transcervical administration of gel to the uterus Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Sterilization Female Non-hormonal Long-acting Pre-clinical TBD TBD $15 (target) Advantages / value proposition: • • • • • • Non-surgical female sterilization method which can be performed in low-resource settings at low cost Fills unmet need, no other low cost permanent female sterilization methods available Proven efficacy in animal models Gel delivery method evaluated in humans, but needs optimizing Preliminary efficacy studies have been completed in humans using a crushed tablet delivery system Similar method using quinacrine hydrochloride was found to be acceptable to women, but efficacy was less than optimal Risks / challenges: • Efficacy of this method in humans needs further evaluation • An erythromycin formulation for this indication is not yet well-defined • Total development costs and time are uncertain and potentially substantial Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 Polidocanol Non-surgical Sterilization (NSS) Family Health International Product: Polidocanol Delivery: Transcervical administration of foam to the uterus Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Sterilization Female Non-hormonal Long-acting Concept TBD TBD $15 (target) Advantages / value proposition: • • • • • Non-surgical female sterilization method which can be performed in low-resource settings at low cost Fills unmet need, no other low cost permanent female sterilization methods available Proven efficacy as sclerosing agent in varicose veins Foam formulation exists for vein sclerotherapy and is in Phase III trials in Europe and Phase II trials in the U.S. Similar method using quinacrine hydrochloride was found to be acceptable to women, but efficacy was less than optimal Risks / challenges: • Efficacy of this method for NSS in humans is unproven • Efficacy of the foam delivery system is unproven in this application • Total development costs and time are uncertain and potentially substantial Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 New(er) male permanent methods No Scalpel techniques Thermal cautery High Intensity Focused Ultrasound FSHβ-Melphalan Conjugates No-scalpel vasectomy: • Equally effective as “traditional” approach to vasectomy • Takes less time to perform • Associated with quicker return to sexual activity • Causes less bleeding, infection and pain • Ligation and excision or thermal cautery, with and w/out facial interposition • Evidence suggests that cautery is more effective—FHI conducting a RCT in India Vasectomy Failure* Rates: Ligation & Excision vs. Cautery *Definition of failure: > 10 million sperm / mL at 12 weeks or later NB: Almost all failures were attributed to recanalization. 14 12 10 8 6 4 2 0 L&E WITHOUT L&E WITH Cautery Fascial Inter.** Fascial Inter.** Techniques*** Data sources: **Sokal et al, BMC Med, 2004; ***Barone et al, BMC Urol, 2004; Sokal et al, BMC Urol, 2004. Labrecque, BMC Urol, 2006. Why Bother with Cautery & NSV? • NSV => safer & less pain • Cautery => low pregnancy rate – If a woman gets pregnant after vasectomy => possible marital conflict – Semen analyses commonly not available => need a good vas occlusion method • Cost-effectiveness is good (Seamans, 2007) Thermal Cautery Device for Low-resource Settings ABS finger pad Nichrome wire Swages Brass contacts Fig. 2 Fig. 1 Handle Cautery tip ($4) Contains two AA Alkaline batteries PATH* showed tips can be sterilized for reuse * Program for Appropriate Technology and Health, Seattle High Intensity Focused Ultrasound (HIFU) Vitality Medical Products Product: High Intensity Focused Ultrasound Delivery: Vas occlusion through tightly focused sound waves from external device Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Sterilization Male Non-hormonal Long-acting Pre-clinical < $10M 2013-2015 $6-10 - once Advantages / value proposition: • • • • • • • • Nonsurgical vasectomy alternative does not require specialized training or sterile operating theater Eliminating surgical element removes one important psychological barrier and is likely to expand male sterilization uptake Male sterilization is one of the most cost-effective contraceptive methods, and HIFU is even lower-cost than vasectomy Likely to be popular in Asia, where surgical vasectomy prevalence already exceeds 6% in 4 countries Would leverage Engender Health and JHBSPH Pop. Reports’ strong vasectomy standardization and promotion campaigns Similar equipment already in use for treating heart defects; contraceptive application tested successfully in dogs Low development cost and quick regulatory path due to medical device, not drug, status Capable company actively seeking foundation partnership and committed to public-sector pricing Risks / challenges: • Even eliminating the surgical nature of vasectomy and resultant psychological and infrastructure/training issues, use of HIFU may be limited in SSA by psychological issues around male role (e.g. condom use is also low) and around permanent methods in general (e.g. female sterilization in SSA stands at ~1.5%) • Lack of awareness, erroneous beliefs, and religious beliefs discourage use of male sterilization • Family planning clinics are generally not geared towards male involvement; successful programs embracing a policy of male involvement in family planning such as those in Latin America would have to be adopted h Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 From Bill Bremner FSHb-Melphalan Conjugates University of Washington/Focused Scientific Product: FSHb-Melphalan Conjugates Delivery: Single-Dose Method of Male Sterilization Type: Target: Mode: Duration1: Stage: Dev. cost2: Launch3: User cost: Advantages / value proposition: • • • • • Non-surgical method of male sterilization Low-cost technology using available compounds, likely to be inexpensive Low risk of side effects Easily administered in developing world settings by injection No need for surgery or surgical expertise Risks / challenges: • Irreversible • Potential for testicular toxicity such as hypogonadism and/or late testicular neoplasms from the melphalan Source: Contraceptive Technology Experts Meeting: Bill &Melinda gates Foundation Feb 2010 Injection Male Non-Hormonal Long/Permanent Pre-clinical 10 million Unknown Unknown Additional research opportunities • Appear to be existing gaps in research on permanent methods, especially FS (existing literature is somewhat dated) • More research needed on: – Factors affecting acceptability of both male and female sterilization (including of non-surgical FS) – Barriers to accessing female sterilization and program approaches to addressing the barriers (cost, availability of services, provider attitudes) – Who can successfully provide sterilization services (task shifting) – Successful communication strategies for sterilization services (mass media, community engagement, etc) – Developing non-surgical female sterilization technologies THANK YOU! Questions?