Common Blood Abnormalities
advertisement

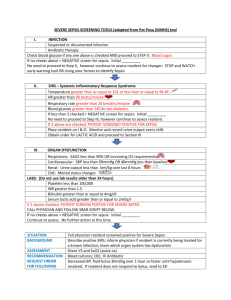
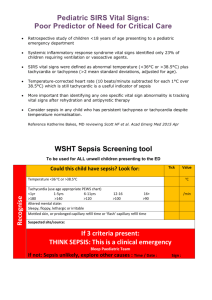
Common Blood Abnormalities Miss Samantha Chambers CT1 General Surgery 3rd August 2015 Aims Recognising common blood abnormalities including; Deranged potassium, sodium, phosphate, magnesium and haemoglobin Learn how to manage these in an acute setting Understand importance of the clinical picture, not just the numbers Hopefully feel a little less scared about Wednesday! Case 1 Mrs A is an 83 yr old lady on the surgical ward admitted today with an incarcerated inguinal hernia You check the bloods for Mrs A at 4.30pm, just as you are about to leave Unfortunately her blood results are as follows; Hb110, WBC 12, CRP 25, Na 138, K+6.5, Ur 6, Creat 102 How are you going to manage this lady? High potassium (hyperkalaemia) Normal range 3.5 – 5.5 >5.5mmol considered raised Threshold for treatment is 6.0 or ECG changes/symptoms Can be caused by AKI (or ESRF) ECG changes in hyperkalaemia: Low, flat p waves Broad, bizarre QRS Slurring into the ST segment Tall tented T waves Management Acute treatment: ECG Stop any antagonistic drugs 10mls 10% Calcium Gluconate (cardiac monitoring) 10 units actrapid insulin in 50mls of 50% dextrose(can do 20%) dextrose over 30 mins Salbutamol 5mg nebs Repeat K+ 4 hours post infusion Longer-term treatment Find cause Calcium resonium 15g TDS Case 2 75 yr old lady, Mrs B, has been on the medical ward with a LRTI for a few days You check her blood results at 6pm, just as you are about to leave and they are as follows (sorry!); Hb 120, WBC 6, CRP16, Na 136, K+2.0, Urea 4.3, Creat 99 How would you manage this lady? Low potassium (hypokalaemia) • Lethargy • Cardiac arrhythmias • Management; • Depends on level • Find the cause • <3 IV replacement – max 80mmol KCl per day via peripheral line • 40mmol in 5% Dextrose or 0.9% N Saline over 412 hours • >3 oral – 2 tablets Sando-K TDS for 3 days only (monitor K+) You are an excellent F1 doctor and have been diligently replacing Mrs B’s potassium inravenously for the past two days You check her blood results today at 7pm, ad are certain that they will have improved; Hb 120, WBC 5, CRP10, Na 135, K+1.9, Urea 4.0, Creat 97 Uh oh! Why hasn’t Mrs B’s potassium improved? What else do you need to check? Remember; In hypokalaemia, always check the magnesium level K+ will not rise if Mg low Low magnesium (hypomagnesaemia) Can be due to poor diet, diuretics (loop), refeeding syndrome Can lead to arrhythmias! Replace as per trust guidelines Either: Magnesium Glycerophosphate 2 tabs (8mmol) TDS for 3 days Or 20mmols MgSO4 in 500/1000ml N.Saline/5% dextrose over 4-8 hours Low phosphate (hypophosphataemia) Can be due to poor diet, GI losses (diarrhoea) Beware REFEEDING SYNDROME If patient not eaten for 5/7 at risk When fed, serum levels of Ca, Mg, PO4, K all plummet Low PO4 can lead to seizures See Intranet guidelines for replacement regimes: Phosphate Sandoz 2 tabs TDS for 3 days Or if <0.5 – Phosphate polyfusor as per guidelines Rate of 9mmol over 12 hours 500ml bag contains 100mmol phosphate So give 100ml over 24 hours – will deliver 20mmol phosphate (must discard rest of bag) Indications for haemofiltration Persistent hyperkalaemia, resistant to treatment Acidosis, resistant to treatment Pulmonary oedema, resistant to treatment Low sodium (hyponatraemia) <135mmol Very common – causes are many, commonest are drugs! PPIs, Diuretics, SSRIs In reality unlikely to cause problems unless < 120-125 Can cause seizures If <135 & >125 and stable can usually just observe Trust guideline on hyponatraemia is good Treatment depends on cause (hypovolaemic, euvolaemic, hypervolaemic) Management; Find the cause; Send urine osmolality and serum osmolality, urine sodium and serum sodium Check drug kardex for culprit drugs Can fluid restrict to 1.5L per day (not if hypovolaemic!) High sodium (hypernatraemia) >145mmol Usually due to dehydration, or too much 0.9% Saline! Treat with IVI (Dextrose, not Hartmann’s or 0.9% Saline!!) If the patient is well, ask them to drink more! Recheck U&E’s Low haemoglobin (anaemia) With low MCV With normal MCV With high MCV Consider the cause Is the patient acutely bleeding? Occult haemorrhage? Post-op? Chronic disease/malignancy? Renal failure? Management; If Hb <80 or patient is symptomatic then usually a role for transfusion – discuss with senior as some clinicians may wish for higher levels in specific situations Transfusion written as RBC to be given over 2-3 hours (in stable patients) If acutely bleeding and massive haemorrhage suspected then activate MHP by calling 2222 High WBC (leucocytosis) Usually a sign of infection Elderly or immunosuppressed (eg. steroids or transplant patients) – dampened immune response so may not mount a leucocytosis in response to sepsis Remember SIRS – WBC <4 or >12 N.B. Patients on steroids may have a neutrophilia Low WBC (neutropenia) Can be caused by sepsis (e.g. atypical infections or elderly) Or by bone marrow suppression e.g. post chemo, or bone marrow failure e.g. MDS Neutropenia <1.0 x109 If <1.0 and signs of SIRS/Sepsis – follow trust neutropenic sepsis guidelines Side room Cultures and CXR IV Abx ( as per guidelines) IVI Discuss with haematology Raised CRP Acute phase inflammatory marker 24 hour lag Can be raised in inflammation, infection, malignancy Will be raised postoperatively Management; Search for cause/source Are there obvious signs of infection eg. urine, chest? If signs of SIRS/sepsis then do a septic screen – CXR, urine dip, ABG, blood cultures, bloods, if indicated: wound, line, drain cultures If suspected source of infection then treat accordingly – sepsis six Do not treat purely on basis of the numbers SIRS and Sepsis SIRS criteria; Temperature <36 or >38 HR >90 bpm RR >20 or PaCO2 >4.3kPa WBC <4 or >11 Sepsis = SIRS + source of infection/suspected source Septic shock = Sepsis + organ hypoperfusion leading to organ dysfunction Low platelets (thrombocytopaenia) Sepsis Post-chemotherapy Coagulopathy Drugs LMWH-induced thrombocytopaenia HITT syndrome If <80 can’t have procedures e.g. liver biopsy or surgery If <50 hold LMWH Management; May need discussion with haematology May require platelets prior to procedure Raised platelets (thrombocytosis) Usually a reactive finding Can be raised due to infection, inflammation, surgery, hyposplenism, splenectomy If persistently raised platelets with no explanation – discuss with haematology re: further investigations ? myelodysplastic syndrome eg. polycythaemia rubra vera, CML Deranged clotting factors DIC – low fibrinogen, raised PT, INR, low platelets Raised INR; Stop warfarin (if on warfarin) Look for cause (if not on warfarin) Trust guidelines for management If INR raised but no acute bleeding – Vitamin K 5mg PO, or Vitamin K 5mg IV – depends on level, and whether operation is likely to take place If acutely bleeding and INR >8 then prothrombin complex (octaplex) needs discussion with haematology first LFT’s made easy… Standard LFTs: Albumin, Bilirubin, ALT/AST, ALP/GGT Raised bilirubin = Jaundiced (>50) Pre-hepatic (unconjugated) e.g. haemolysis, Gilbert’s syndrome Hepatic (mixed) e.g. viral hepatitis, drugs, ischaemia Post hepatic/ obstructive (conjugated) – dark urine, pale stools ALP/GGT are markers of obstructive jaundice i.e. gallstone in CBD ALT/AST are makers of hepatic damage i.e. viral hepatitis If ALP/GGT rise is > than ALT/AST it’s a post hepatic problem If ALT/AST rise is >ALP/GGT it’s a hepatic problem Hepatitis screen Serology – Hep B, Hep C, (Hep A and E), HIV Autoantibodies – AMA, SMA, ANCA, LKM Iron studies – Ferritin, Serum Iron, TIBC, Transferrin sats Others – A1AT genotype, Caeruloplasmin & Copper levels Don’t forget to USS the liver P.S. You don’t need to get a gastro review before doing these! Low albumin (hypoalbuminaemia) Negative phase inflammatory marker In sepsis it will drop – this doesn’t mean they’re malnourished Can be low as a marker of malnutrition if chronic (but Anorexics often have normal levels) When <20-24 can develop oedema No role for IV albumin replacement!! Low calcium (hypocalcaemia) Can occur due to drugs (diuretics), poor diet, refeeding syndrome <2.2 (adjusted calcium) Symptoms includes cramps and tetany Management; ECG AdCal1-2 tabs OD or IV replacement 10mls 10% Calcium gluconate Prolongation of QT interval (QTc) Raised calcium (hypercalcaemia) Can occur in renal failure, Management; dehydration and malignancy (particularly breast) Stones, bones, moans, psychological groans Renal tract calculi Bone pain / fractures Constipation Depression ECG IV fluid replacement Bisphosphonates eg. Pamidronate – only if calcium >3 Discuss with renal team if associated renal failure Shortening of QT interval Case 3 78 yr old man, Mr C PC – ‘Off legs’ HPC – Care staff state he has been unwell for past few days in the care home. No appetite. Unable to mobilise today. Seems more confused PMH – IHD, MI x 3 previously, previous TIA’s, prostate cancer and chronic back pain Allergies – Nil Medications – Ramipril, spironolactone, omeprazole, MST (recently started by pain team) Social – Lives in a care home, usually lucid and able to undertake personal care for himself O/E: Unkempt and strong smell of urine Temp 38.6, BP 130/80, HR 68bpm, regular, RR 16, 02 sats 98% on air Appears very confused – believes he is at his marital home, and that the year is 1972 Not oriented in time/place/person HS 1+11+0 Chest - Reduced air entry at left base Abdomen soft, non-tender Investigations Bedside Urine dip – positive for leucocytes, nitrites and protein ECG- no acute ischaemic changes Bloods Hb 120, WBC 16, Ur 8.9, Creat 109, K+4, Na 125, CRP 40, INR 1 Imaging CXR- cardiomegaly, shadowing at left base suggestive of consolidation Differentials? Acute confusion secondary to; UTI LRTI Hyponatraemia Opioids Confusion screen Acute confusion, acute delirium or undiagnosed dementia? Septic screen inc FBC, U&Es, LFTs, CRP, BCMs, urine dip, CXR Check TSH, B12, Folate Consider CT head Check the drug chart!! Case 4 A 92 yr old gentleman, Mr D, is admitted having sustained a right NOF fracture. He was given diclofenac in A&E as he was in a lot of pain. He is operated on, on the same day of admission (which is a Saturday, Jeremy), and is taken back to the orthopaedic ward. Unfortunately they are extremely understaffed, and Mr D, who usually requires assistance to eat and drink, gets slightly overlooked as there is a very sick patient overnight who is periarrest His initial blood results were; Hb 140 WBC 6 CRP 6 Na 140 K+4.5 Ur 5 Creat 90 You are the F1 on call on Sunday and are asked to recheck his blood results… His blood results today are; Hb 135 WBC 10 CRP 15 Na 144 K+4.4 Ur 10 Creat 190 O/E: Appears very dehydrated, with dry mucous membranes Observations stable No oozing from wound site HS1+11+0 Chest clear Abdomen soft, non-tender Urine output for past 3 hours ~ 15ml How will you manage Mr D? Acute kidney injury In adults, a diagnosis of AKI can be made if: Blood creatinine level has risen from the baseline value for that person (by 26 micromoles per litre or more within 48 hours) Blood creatinine level has risen over time (by 50% or more within the past 7 days) Oliguria (less than 0.5ml per kg per hour for more than 6 hours) Management; Try to identify a cause eg. recent contrast? Dehydration? Stop any culprit drugs (especially NSAID’s in elderly) IV fluid replacement Discuss with renal team Dehydration A proportional rise in both urea and creatinine membranes, patient feels thirsty, oliguria or anuria However, urea may be slightly more raised than creatinine Note: If urea is dramatically raised out of proportion to creatinine – suspect GI bleed (as the blood acts as a protein meal) Clinically – dry mucous Management; Search for the cause IV fluid replacement Catheterise patient Meet fluid demand eg. if high output fistula/stoma Discuss with renal team Summary Remember to repeat the sample if you suspect a spurious result Common things are common – low/high potassium and sodium and anaemia Trust guidelines can be very useful Don’t panic! If in doubt, ask! Questions?