Skin Structure and Color
advertisement

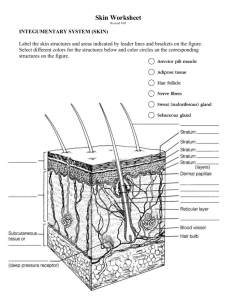
Skin Structure and Color The Integument Fun Facts What Makes it up It’s the body largest organ composed of all four tissue It covers your body- (skin types and its derivatives: nail, Surface is covered by epithelium hair, sweat glands and with an underlay of connective sebaceous glands) tissue Skin is also known as the Smooth muscles control blood vessel diameter and hair position cutaneous membrane Neural tissue provides the sensory reception What are the major characteristics of the skin? Waterproof, stretchable,washable, and permanent, automatically repairs small cuts, rips and burns and is guaranteed to last a lifetime. Surface area of up to 1-2 square meters 11 pounds 12-15% of total body weight Pliable yet tough 1-2 mm thick Integumentary System Includes: Skin (cutaneous membrane) Subcutaneous tissue below the skin Accessory Structures Sweat glands Sebaceous or oil glands Hair Nails What are the 3 major layers of the skin? Epidermis (epi-upon) Composed of epithelial tissue (stratified squamous) Non-vascularized The superficial portion of skin Dermis – underlies the epidermis Tough leathery layer composed of fibrous connective tissue Good supply of blood The deeper layer of skin Primarily made up of connective tissue i.e. dense irregular tissue Hypodermis (not considered skin) Made of adipose and areolar tissue Stores fat, anchors skin, protects against blows Epidermis Dermis Basement membrane Overview of the Epidermis Remember from the last unit: It is avascular Stratified squamous (more than one layer of squishy cells) Made up of four types of cells Has five distinct layers Mitotic (25-45 day turnover rate) No nerves or sensory receptors Oxygen and nutrients diffuse from the underlying dermis The epidermis is a keratinized stratified squamous epithelium. Cells of the Epidermis Keratinocytes-produce keratin which protects the skin and underlying tissues, 90% of epidermal cells are kertanized Melanocytes-produce melanin which contributes to skin color and absorbs UV light, 8% of epidermal cells Langerhans cells-participates in immune response and is derived from bone marrow and present in lymph nodes Merkel cells-contain a sensory structure called a tactile (Merkel) disc and function in the sensation of touch, least numerous of epidermal cells Main Epidermal Cell Types Keratinocytes All strata (layers) Melanocytes Stratum basale What are the different types of cells in the epidermis? Keratinocytes Produce a fibrous protein called keratin Are formed in the lowest levels of the epidermis. Pushed upward by the production of new cells beneath them. Become dead and scale-like Millions rub off everyday What are the different types of cells in the epidermis? Melanocytes Synthesizes the pigment melanin (Melan-black) Can transfer melanin to keratinocytes Protects skin from ultraviolet light. melanocyte Melanin in keratinocytes What are the different types of cells in the epidermis? Langerhans’ cells Formed in bone marrow. Move to the skin Macrophages Easily damaged by UV light Langerhans’ cell What are the different types of cells in the epidermis? Merkel Cells Has a spiked appearance Connected to nerve cells from dermis (deepest layer) Function as sensory receptors for touch. 5 Epidermal Strata First Layer of the Epidermis The stratum basale AKA stratum germinativum is the deepest layer of the epidermis (closest to the dermis). It is found close to the dermal blood supply. It consists of a single layer of columnar or cuboidal cells which rest on the basement membrane. Basal cells are the stem cells of the epidermis. Their mitotic activity replenishes the cells in more superficial layers as these are eventually shed from the epidermis. The renewal of the epidermis takes about 3 to 4 weeks in humans as millions of cells are produced daily. Cells die as they are pushed away from the source of nourishment. Cells undergo keratinization as a tough protein, keratin, is deposited within the cell. Keratin hardens and flattens the cells as they move outward and it waterproofs the skin. Merkel cells, melanocytes, keratinocytes and stem cells divide rapidly here and if this is damaged new skin cannot regenerate with a skin graph. Optional Epidermal Layers In the stratum spinosum, the cells become irregularly polygonal. The cells are often separated by narrow, translucent clefts. These clefts are spanned by spine-like cytoplasmatic extensions of the cells (hence the name of the layer and of its cells: spinous cells), which interconnect the cells of this layer. Provides strength and flexibility, 8-10 cell layers thick, intermediate layer, contains keratinocytes. The stratum granulosum consists, in thick skin, of a few layers of flattened cells. Only one layer may be visible in thin skin. Transition between the metabolically active cells and the dead cells from the more superficial layers; 3-5 layers of dying cells on the most superficial part More Layers The stratum lucidum consists of several layers of flattened dead cells. Nuclei already begin to degenerate in the outer part of the stratum granulosum. In the stratum lucidum, faint nuclear outlines are visible in only a few of the cells. The stratum lucidum can usually not be identified in thin skin. (ONLY found in palms and soles of feet)-3-5 layers of clear, flat, dead cells; contains a precursor to keratin . Final Epithelial Layer In the stratum corneum,cells are keratinized and form a layer that is about 30 cells thick. Individual cells are difficult to observe because (1) nuclei can no longer be identified, (2) the cells are very flat and (3) the space between the cells has been filled with lipids, which cement the cells together into a continuous membrane. Closest to the surface of the epidermis, the stratum corneum has a somewhat looser appearance. Cells are constantly shed from this part of the stratum corneum. This layer makes up three fourths of the epidermal thickness. The protection of the body by the epidermis is due to the functional features of the stratum corneum. Continuously sheds cells, 25-30 layers of flat dead cells filled with keratin and surrounded by lipids; barrier to light, heat, water, chemicals and bacteria (calluses form-caused by an abnormal thickening of the epidermis) Dandruff Average person shed 40 pounds of these cells in their lifetime. Everything you see on a human is dead! Growth Newly formed cells in stratum basale undergo keratinazation as they are pushed to the surface They accumulate more keratin during the process They then undergo apoptosis Eventually they slough off and are replaced The process takes about 4 weeks Rate of cell division in the stratum basale increases during injury Now to the Dermis Composed of collagen (makes up 70% of the dermis), elastic fibers, fibroblasts, macrophages and fat cells (connective tissue) Contains hair follicles, glands, nerves and blood vessels (which means its vascular) Mitotic Is divided into two major regions: papillary and reticular regions Dermis or corium The dermis, or corium, consists of dense fibrous connective tissue with numerous collagenous and elastic fibers. The dermis is much thicker than the epidermis. In thick skin, dermal papillae create a very irregular border between epidermis and dermis. Blood vessels, nervous tissue, some muscle tissue, certain glands, hair and nails are found in the dermis. Nerve endings allow us to sense pain, temperature, pressure, and touch. 2 Dermal Strata Papillary layer Reticular layer Dermis Regions Papillary Reticular Top 20 % of the dermis Made of dense irregular connective Forms fingerprints Contains finger-like projections called dermal papillae which Anchors epidermis to dermis Contains capillaries the feed epidermis Contains nerve endings for sensations of heat, cold, pain, tickles and itches tissue Contains interlacing collagen and elastic fibers,provides strength and elasticity (stretch marks are dermal tears in the skin) Packed with oil glands, sweat glands ducts and fat and hair follicles Matrix is filled with thick bundles of collagen fibers (give the skin strength) Less dense regions are called lines of cleavage or tension lines; surgeons use these to make incisions because they heal quicker. Fingerprints! E=eponychium N=nailbed H= hyponychium DP= distal phalanx Dermal Cell Types Fibroblasts Collagen fibers Elastic fibers Collagenous Fibers Close-up of a single fiber Interwoven strands of the protein collagen. The most abundant protein in the human body. Thick fibers with great tensile strength – i.e., it’s tough to pull them apart. In fresh tissue, they have a white appearance, so they are sometimes called white fibers. In stained slides, they are often pink and they usually appear quite wavy. Tendons, ligaments, and the deep layer of the skin (the dermis) are made primarily of collagenous fibers. Multiple fibers arranged in the extracellular matrix Elastic Fibers Made primarily of a protein called elastin, whose coiled structure allows it to stretch and snap back like a rubber band. Account for the ability of the lungs, arteries, and skin to spring back after they are stretched. Fresh elastic fibers are yellowish and thus often called yellow fibers. In this slide, “A” is an elastic fiber Below the Dermis Deep to the dermis is the subcutaneous layer or hypodermis This is NOT part of the skin Consists of areolar and adipose tissue Used for fat storage, blood vessel passage and is an area of pressure sensing nerve endings Attaches the skin to underlying organs and tissues Subcutaneous Tissue Location & tissue type… Adipocytes What causes the color of skin? The red and yellow hues of the skin are due to hemoglobin in the red blood cells, which pass through the capillaries beneath the epidermis, and carotene (yellowish pigment), which accumulates in fat cells found in the dermis and hypodermis (subcutaneous layer beneath dermis). 3 pigments contribute to skin color Melanin- protein pigment (natural sunscreen) Can range in color from yellow to reddish-brown to black Everyone has the same number of melanocytes but make varying amounts and colors (differences in skin color) Increased melanin production can caused by sunlight by protectsing the chromosomes of mitotically active basal cells against light-induced damage. Carotene-yellow to orange pigment found in carrots. Most commonly found in the palms or soles. Most intense when large amounts of carotene-rich foods are eaten. Hemoglobin- Red blood gives a pinkish hue to fair skin Hormonal Control of Pigmentation • Pigmentation is not just under the control of light. Hormones produced by the pituitary and the adrenal glands also affect pigmentation. Diseases of these two endocrine organs often result in changes of pigmentation of the skin. Malfunctioning Melanocytes Albinism – melanocytes completely fail to secrete melanin. Hair, skin, and iris are white. Vitiligo – loss of pigment in certain areas of the skin producing white patches. Freckles and moles are formed when melanin becomes concentrated in local areas. Malignant melanoma – a cancerous change in a mole that may metastasize (spread) rapidly and is most difficult to treat. Exposure to sunlight increases risk. Other Pigments in Skin Carotene – a yellow pigment in skin usually hidden by the effects of melanin. Asians have little melanin which allows the yellow to show more than other nationalities. Pinkish color – seen in fair-skinned persons because the vascular dermis is visible. Cyanosis – blue look to skin due to poorly oxygenated blood Blushing – caused by dilation of blood vessels Pale by fright – caused by restriction of vessels Response to Disease Jaundice – caused when bilirubin is deposited in skin because a diseased liver is unable to excrete this pigment Skin may appear bronzed due to the deposit of excess melanin when a person’s adrenal gland is functioning poorly. A bruise indicates that blood has escaped from the blood vessels and has clotted under the skin. Over eating carotene-rich vegetables such as carrots may cause skin to have a yellow tint. Albinism-can’t produce melanin