Duchenne Muscular Dystrophy: Gastrointestinal - CARE-NMD
advertisement

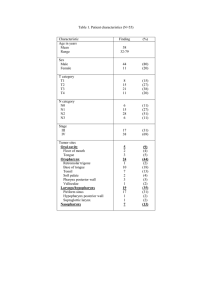
Duchenne Muscular Dystrophy: Gastrointestinal Management Introduction • Patients at risk of both undernutrition and being overweight • Range of experts may be needed as condition progresses – Dietician or nutritionist – Swallowing/Speech and language therapist (SLT) – Gastroenterologist • These experts should – Guide the patient to maintain good nutritional status and wellbalanced diet (with tube-feeding if necessary) – Monitor/treat swallowing problems (dysphagia) to prevent aspiration and weight loss, and assess/treat delayed speech/language problems – Treat common problems of constipation and gastrooesophageal reflux with medication and non-medication therapies Nutritional management (1) • Forward planning needed from diagnosis onwards to maintain good nutritional status – Poor nutrition can adversely affect almost every organ system – Patients require a well-balanced diet with a full range of food types • Weight or BMI for age should be maintained between 10th and 85th percentile on national charts Nutritional management (2) • Regular monitoring is required for – Weight – Linear height (ambulatory patients) every 6 months – Arm span/segmental length (non-ambulatory patients) • Refer to expert dietician at diagnosis and steroid initiation • Further referral triggers include – If patient is underweight (<10th age percentile), at risk of becoming overweight (85th-95th age percentile), or overweight (95th age percentile – Unintentional weight loss/gain, or poor weight gain – If major surgery is planned – If patient is chronically constipated, or if dysphagia is present Upon referral • Diet should be assessed for energy, protein, fluid, calcium, vitamin D and other nutrients • Daily multivitamin recommended (including vitamin D and minerals) • If this is not general practice, computer nutrient analysis of diet can provide evidence for possible need for specific foods or supplements • If suspicion of undernutrition/malnutrition and poor intake, serum vitamin concentrations can be obtained and supplements recommended Swallowing management (1) • In later stages, pharyngeal weakness can lead to dysphagia – Can further accentuate nutritional issues/loss of respiratory strength – Can occur gradually and be difficult to spot • Clinical swallowing examination indicated if – Unintentional weight loss of ≥ 10% – Decline in expected age-related weight gain • Referral necessary if any clinical indicators of dysphagia – Prolonged mealtimes (>30 minutes), or mealtimes accompanied by fatigue, excessive spilling, drooling, pocketing – Persistent coughing, choking, gagging, or wet vocal quality during eating/drinking • Swallowing problems necessitating assessment may also be indicated by – Aspiration pneumonia – Unexpected decline in pulmonary function – Fever of an unknown origin Swallowing management (2) • Videofluroscopic study of swallowing (modified barium swallow) necessary for patients with clinical indicators of possible aspiration and pharyngeal dysmotility • For patients with dysphagia, a Speech Language Therapist (SLT) with training/expertise in treatment of oral-pharyngeal dysphagia should be involved • They can deliver an individualised treatment plan of swallowing interventions/compensatory strategies with aim of preserving good swallowing function. Swallowing management (3) • As disease progresses, most patients begin to experience increasing difficulty with chewing, and subsequently exhibit pharyngeal-phase swallowing deficits in young adulthood • Gastric tube placement should be offered when efforts to maintain weight and hydration by oral means are insufficient – Potential risks/benefits should be carefully discussed with family. – A gastrostomy may be placed by endoscopic or open surgery, taking into account anaesthetic considerations and family/personal preferences Gastrointestinal management (1) • Most common conditions in DMD are constipation and gastro-oesophageal reflux • Constipation: typically at older age/after surgery – Laxatives, stool softeners and stimulants necessary for acute constipation or fecal impaction; daily laxatives necessary if symptoms persist – Use of enemas might be needed occasionally – Adequacy of free-fluid intake should be determined and addressed – Increased fibre may worsen symptoms, especially if fluid intake not increased Gastrointestinal management (2) • Gastro-oesophageal reflux (causing heartburn) – Typically treated with proton-pump inhibitors or H2 receptor antagonists – Prokinetics, sucralfate, and neutralising antacids are adjunctive therapies – Acid blockers commonly prescribed to children on steroid therapy or oral bisphosphonates to avoid complications • With increasing survival, other complications are being reported, including – Intestinal swelling related to air swallowing due to ventilator use – More rarely, delayed gastric emptying and ileus Speech and language Management • Delayed acquisition of early milestones common in DMD – Differences in language acquisition and language skill deficits persisting through childhood • Referral to SLT for assessment/treatment necessary on suspicion of difficulties with speech acquisition, or continuing deficits in language comprehension or oral expression • Oral motor exercises and articulation therapy necessary for young boys with hypotonia and older patients with deteriorating oral muscle strengths and/or impaired speech intelligibility • Compensatory strategies, voice exercises, and speech amplification appropriate in older boys if intelligibility deteriorates • Voice Output Communication Aid assessment appropriate at all ages if speech output is limited Oral care • Not yet part of published international consensus. Scandinavian consensus/ TREAT-NMD expert recommendations • Patients should see dentist with extended experience and detailed knowledge of DMD – Preferably at a centralised/specialised clinic – Aware of specific differences in dental/skeletal development in DMD – Will collaborate with well-informed/experienced orthodontist • Should strive for high-quality treatment, oral health and wellbeing, and function as resource for family and boy’s community dentist • Oral/dental care should be based on prophylactic measures to maintain good oral/dental hygiene • As progressive loss of arm function systematically erodes ability for independent tooth brushing, this needs to be specifically addressed as an area for attention to uphold oral hygiene • Specific alerts necessary if on bisphosphonate treatment References & Resources • The Diagnosis and Management of Duchenne Muscular Dystrophy, Bushby K et al, Lancet Neurology 2010 9 (1) 77-93 & Lancet Neurology 2010 9 (2) 177-189 – Particularly references, p186-188 • The Diagnosis and Management of Duchenne Muscular Dystrophy: A Guide for Families • TREAT-NMD website: www.treat-nmd.eu • CARE-NMD website: www.care-nmd.eu





![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)


