NUR103Abdomen
advertisement

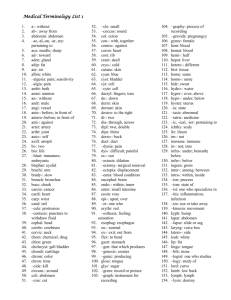
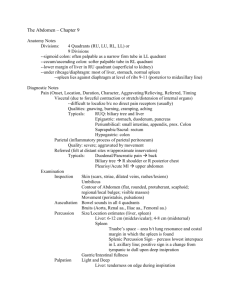
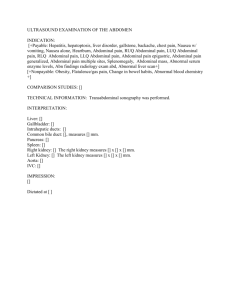
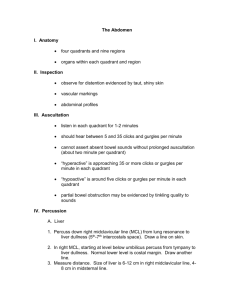
NUR 103 Health Assessment The Abdomen Objectives: • Define terminology related to assessment of the abdomen. • Describe anatomy and physiology of abdomen. • Identify equipment. • Identify positioning. • Identify techniques. • Explain the process of performing an assessment of the abdomen. • Recognize normal and abnormal assessment data. • Differentiate between normal and abnormal assessment data. Terminology • Abdomen- a large oval cavity extending from the diaphragm down to the brim of the pelvis. • Aneurysm- defect or sac formed by dilation in artery wall. • Anorexia- loss of appetite. • Ascites- abnormal accumulation of serous fluid within the peritoneal cavity. • Borborygmi- loud gurgling bowel sounds- inc. motility or hyperperistalsis. • Bruit- blowing, swooshing sound heard through stethoscope when artery is partially occluded. • Cecum- first or proximal part of large intestine. • Cholecystitis- inflammation of the gallbladder. • Costal margin- lower border of rib margin formed by dedial edges of 8th, 9th, and 10th ribs. • Costovertebral angle (CVA)- angle formed by the 12th rib and vertebral column on posterior thorax, overlying kidney. • Diastasis recti- midline longitudinal ridge in abdomen, separation of abdominal rectus muscles. • Dysphagia- difficulty swallowing. • Epigastrium- name of abdominal region between the costal margins. • Hepatomegaly- abnormal enlargement of liver. • Hernia- abnormal protrusion of bowel through weakening in abdominal musculature. • Inguinal ligament- ligament extending from pubic bone to anterior superior iliac spine, forming lower border of abdomen. • Linea alba- midline tendinous seam joining the abdominal muscles. • Paralytic ileus- complete absence of peristaltic movement. • Peritoneal friction rub- rough grating sound heard through stethoscope over site of peritoneal inflam. • Peritonitis- inflam. of peritoneum. • Pyloric stenosis- congenital narrowing of pyloric sphincter, forming outflow obstruction of stomach. • Pyrosis- (heartburn) burning sensation in upper abdomen, due to reflux of gastric acid. • Rectus abdominis muscle- midline abdominal muscles extending from rib cage to pubic bone. • Scaphoid- abnormally sunken abdominal wall. • Splenomagaly- abnormal enlargement of spleen. • Striae- (linia ablicantes)- silvery white or pink scar. • Suprapubic- name of abdom. Region just superior to pubic bone. • Tympany- high-pitched, musical, drumlike percussion note heard when percussing over stomach and intestine. • Umbilicus- depression on abdom. Marking site of entry of umbilical cord. • Viscera- internal organs. • Solid viscera- characteristic shape (liver, pancreas, spleen, adrenal glands, kidneys, ovaries, and uterus). • Hollow viscera- shape depends on contents (stomach, gallbladder, small intestine, colon, and bladder). Anatomy of the Abdomen Divided into 4 quadrants Right upper quadrant: Liver Gallbladder Duodenum Head of Pancreas Right kidney and adrenal Hepatic flexure of colon Part of ascending & transverse colon Left upper quadrant: Stomach Spleen Left lobe of liver Body of pancreas Left kidney & adrenal Splenic flexure of colon Part of transverse & descending colon Right Lower Quadrant: Cecum Appendix Right ovary and tube Right ureter Right Spermatic cord Left Lower Quadrant: Part of descending colon Sigmoid colon Left ovary and tube Left ureter Left spermatic cord Midline: Aorta Uterus (if enlarged) Bladder (if distended) The Right Quadrant of the Abdomen: The Liver The liver is located in the upper right portion of the abdominal Cavity, just below the diaphragm. Partially surrounded by the ribs, Extends from the level of fifth Intercostal space to lower margin of the ribs. Gallbladder The gallbladder is a pearshaped sac located in a depression on the Inferior surface of the right hepatic lobe. Duodenum The duodenum is part of the small Intestine. Approx. 25 cm Long and 5 cm in diameter. It passes in front of the right kidney And the upper three lumbar vertebrae. Right Kidney The kidney is a reddish brown, bean shaped Organ with a smooth surface. 12 cm long, 6 cm wide, 3 cm thick in adult. The right kidney lies on the right side of the vertebral column in a depression high On the posterior wall of the abdominal cavity (retroperitoneal). Right kidney is lower than Left kidney. Head of pancreas The pancreas is a soft, lobulated gland located behind the stomach. It extends horizontally across the posterior Abdominal wall with its head in the C-shaped curve of the duodenum and its tail against the Spleen. Hepatic flexure of colon, part of ascending and transverse colon: Ascending-Portion of the large Intestine that passes Upward on the right Side of the abdomen From the secum to the Lower edge of the liver. Transverse- extends across Abdomen from right to left below Stomach. Left Upper Quadrant: Stomach: Digestive organ located between the esophagus and the small intestine. The Spleen: A soft mass of lymphatic Tissue on posterolateral Wall of abdominal cavity, Immed. Under diaphragm. Lies obliquely, with long axis Behind and parallel to 10th rib. Lateral to midaxillary line. Continuation of left quadrant of abdomen: Left lobe of liver: Body of pancreas: Left kidney and adrenal Splenic flexure of colon Part of transverse and Descending colon Right Lower Quadrant of Abdomen • Cecum • Appendix • Right ureter • Right spermatic cord • Right ovary and tube Left Lower Quadrant of the Abdomen: Part of descending colon Sidmoid colon Left ovary and tube Left ureter Left Spermatic cord Midline Anatomy of Abdomen: Aorta Uterus (if enlarged) Bladder ( if distended) EQUIPMENT • Proper lighting: include strong overhead light and secondary stand light. • Stethoscope • Small centimeter ruler • Skin-marking pen • Alcohol swab (to clean endpiece) Positioning: •Position the person supine, with head on a pillow, knees bent or on pillow, and arms at sides or across the chest. Note: Discourage person from placing arms Over the head because this tenses abdom. Musculature. Techniques: • • • • • • Provide strong lighting Have person empty bladder Keep room warm to avoid chilling & tensing of muscles Position person supine Warm stethoscope and hands to avoid abdom. Tensing. Inquire re: painful areas, examine such area last to avoid musculature guarding. • Finally, learn distraction tech. Enhance muscle relaxation through breathing exercises, emotive imagery, low, soothing voice, allowing person to relate abdominal hx while you palpate. Inspection: Inspection of abdomen: • Normal Findings: • Abnormal Findings: Contour 1. Stand on person’s right side, look on abdomen. 2. Your head should be slightly higher than abdom. 3. Determine profile from rib 3. Scaphoid abdomen, margin to pubic bone. protuberant abdomen, Contour describes nutitional abdominal distention. state. Normal ranges from flat to rounded. Symmetry of Abdomen • 1. 2. 3. 4. 5. Normal Findings: Shine a light across abdom. toward you, or shine lengthwise across person. Abdomen should be symmetric bilaterally. Even small bulges are highlighted by shadow. Step to foot of examination table to recheck symmetry. Ask person to take deep breathfurther highlight any change. Abdom. Should stay smooth and symmetric. • Abnormal Findings: 2. Bulges, masses 3. Hernia- protrusion of abdom. Viscera through abnormal opening in muscle wall. Note any localized bulging. Hernia, enlarged liver or spleen may show. Inspection of Umbilicus: • Normal Findings: 1. Normally at midline, inverted, no sign of discoloration, inflam., or hernia,. Becomes everted and pushed upward with pregnancy. • Abnormal Findings: 1. Everted with acites, or underlying mass. 2. Deeply sunken with obesity. 3. Enlarged and everted with umbilical hernia. 4. Bluish periumbilical color occurs with intraabdominal bleeding (Cullen’s Sign) Inspection of skin • 1. Normal Findings: Surface smooth, even, homogeneous color. 2. Striae- pink, or blue, then silvery white pigment changes. 3. Moles-circumscribed brown macular or papular areas. 4. No lesions present. May have wellhealed surgical scar, draw location in pt. record, indicating length in cm. 5. Veins usually not seen, fine venous network may be visible in thin persons. 6. Good skin turgor- healthy nutrition. Pinch up fold of skin, release to note skin’s Immediate return to original position. • 1. 2. 3. 4. 5. Abnormal Findings: Redness with localized inflammation, jaundice, Skin glistening and taut (ascites). Striae look purple-blueCushing’s Syndrome (excess adrenocortical hormone causes skin to be fragile). Unusual color or change in shape of mole. Petechiae. Cutaneous angiomas (spider nevi) occur with portal HTN or liver disease. Lesions, rashes. Prominent, dilated veins- portal HTN, cirrhosis, ascites, or vena caval obstruction. Veins more visible – malnutrition due to thinned adipose tissue. Pulsation or movement: • Normal Findings: 1. Pulsations normally seen from aorta beneath skin in epigastric area. 2. Respiratory movement in abdomen (males). 3. Waves of peristalsis in very thin persons. (ripple slowly & obliquely across abdom.) • Abnormal Findings: 1. Marked pulsations of aorta occurs with widened pulse pressure (HTN, aortic insuff., thyrotoxicosis) & aortic aneurysm. 3. Marked visible peristalsis, with distended abdomenintestinal obstruction. Inspection of abdomen Hair distribution, Demeanor • Normal Findings: 1. Pubic hair growth normally diamond shape in adult males, inverted triangle shape in females. 2. Demeanor- comfortable person relaxed on exam. Table, a benign facial expression, slow, even resp. • Abnormal Findings: 1. Patterns alter with endocrine or hormone abnormalities, chronic liver diseases. 2. Restlessness, constant turning to find a comfortable position occur with colicky pain of gastroenteritis or bowel obstruction. Auscultation of Abdomen Note: Perform auscultation next because percussion and palp. can increase peristalsis, which could give false interpretation Of bowel sounds. Bowel Sounds and Vascular Sounds: 1. Use diaphragm endpiece- Bowel sounds are high pitched. 2. Hold stethoscope lightly against skin (pushing too hard may stim. More bowel sounds. 3. Begin in RLQ at ileocecal valve area (bowel sounds are almost always present here normally). Bowel Sounds • Normal Findings: 1. Note character of bowel sounds. Wide range of normal sounds, irreg. (5-30 times/min.) 2. Borborygmus- type of hyperactive bowel sound fairly common. (when you feel your stomach growling). 3. Note: you must listen for 5 min. before deciding if BS are completely absent. • Abnormal Findings: 1. Two distinct abnorm. sounds: A. Hyperactive- loud, highpitched, rushing, tinkling sounds-signal inc.motility. B. Hypoactive-or absent sounds. Vascular Sounds • Normal Findings: 1. As you listen, note presence of vscular sounds or bruits. 2. Using firmer pressure, check over aorta, renal arteries, iliac, and femoral arteries. No sound is normal. • Abnormal Findings: 1. Note location, pitch, and timing of vascular sound. 2. Systolic bruit is pulsatile blowing sound, occurs with stenosis or occlusion of artery. 3. Venous hum, peritoneal friction rub are rare. Vascular Sounds Femoral artery Percussion of abdomen: General tympany, liver span, splenic dullness. Percussion: • To assess relative density of abdominal contents, to locate organs, and to screen for abnormal fluid or masses. General Tympany • Normal Findings: 1. First, percuss lightlyall four quad. to determine amt. tympany & dullness. 2. Tympany should predominate. • Abnormal Findings: 1. Dullness occurs over distended bladder, adipose tissue, fluid, or mass. 2. Hyperresonance is present with gaseous distention Liver Span • 1. 2. 3. 4. 5. Normal range of findings: Next, map out boundaries of certain organs. Measure ht. of liver in right midclavicular line. Begin in area of lung resonance, percuss down interspaces until sound changes to dull quality. Mark the spot (usually in 5th intercostal space. Then find abdom. Tympany & percuss u midclavicular line. Mark where sound changes from tympany to dull sound, normally at right costal margin. Measure distance between two marks; normal liver span in adult ranges from 612 cm. Height of liver span correlates ht. of person, taller have longer livers. • Abnormal Findings: 2. Enlarged liver span indicates liver enlargement or hepatomegaly. 3. Accurate detection of liver borders is confused by dullness above the 5th intercostal space (Lung disease, e.g.,pleural effucion or consolidation.) Accurate detection at lower border is confused when dullness is pushed up with ascites or pregnancy or gas distention in colon. Normal range of findings, cont’d. • One variation occurs with chronic emphysema, which the liver is displaced downward by hyperinflated lungs. Although dull percussion is noted well below right costal margin, the overall span is still WNL’s. • Clinical estimation of liver span is important to screen for hepatomegly & to monitor changes in liver size. Measurement is a gross estimate, liver span may be underestimated because of inaccurate detection of upper border. • Scratch test- final tech. may help define liver border when abdom. Is distended or abdom. Muscles are tense. Splenic Dullness • 1. 2. Normal Findings: Spleen is obscured by stomach contents, may locate by percussing for dull note from 9th-11th intercostal space behind left midaxillary line. Now, percuss in lowest interspace in left anterior axillary line. Tympany should result. Ask person to take deep breath, normally, tympany remains through full inspiration • 1. 2. Abnormal Findings: Dull note forward of midaxillary line indicates enlargement of spleen (mononucleosis, trauma, infection). In this site, anterior axillary line, change in percussion from tympany to dull sound wit full inspiration is positive spleen percussion sign, indicating splenomagaly. This method will detect mild to mod. Splenomegaly before spleen becomes papable (mononucleosis, malaria, or hepatic cirrhosis). Costovertebral Angle Tenderness • • Normal Findings: 1. Indirect fist percussion 1. causes tissues to vibrate instead of producing a sound. 2. To assess the kidney, place one hand over the 12th rib at the CVA on the back. Thump that hand with the ulnar edge of other fist. No pain elicited. Abnormal Findings: Sharp pain occurs with inflammation of kidney or paranephric area. Special Procedures: Ascites • 1. Fluid Wave: First, test for a fluid wave by standing on person’s right side. Place ulnar edge of another examiner’s hand on abdomen in midline. Place left hand on person’s right flank. With right hand, reach across abdomen and give the left flank a firm strike. If ascites is present, the blow will generate a fluid wave through the abdomen, & feel distinct tap on left hand. If distended from gas or adipose tissue, no change. • Shifting Dullness: 1. In a supine position, ascitic fluid settles by gravity into the flanks, displacing air-filled bowel upward. You will hear a tympanitic note as yu percuss over the top of abdomen because gas-filled intestines float over the fluid. 2. Then percuss down side of abdomen. If fluid is present, the note will change from tympany to dull as you reach its level. 3. Now turn pt. to right side (roll toward you). Fluid will gravitate to dependent side. Begin percussing upper side of abdomen and move downward. Sound changes from tympany to dull sound as you reach fluid level. This level of dullness is higher, upward toward the umbilicus. Palpation of Abdomen 1. Palpation is performed to judge the size, location, & consistency of certain organs & to screen for an abnormal mass or tenderness. Technique for palpation 1. 2. 3. 4. 5. 6. 7. Bend the person’s knees. Keep palpating hand low & parallel to abdomen. Teach pt. to breathe slowly (in through nose, out through mouth). Keep your own voice low & soothing. Conversation may relax the pt. Try “emotive imagery”. Keep pt.’s hand under your finger curled over his/her fingers for very ticklish person. People are not ticklish to themselves. Alternatively, perform palpation just after auscultation. Keep stethoscope in place & use stethoscope until pt. is used to being touched. Light palpation: • 1. 2. 3. 4. 5. 6. Normal Findings: Begin with light palpation. With first four fingers close together, depress skin about 1 cm. Make gentle rotary motion, sliding fingers & skin together. Lift fingers, do not drag them, & move clockwise to next location around abdom. Objective here is not to search for organs but to form overall impression of skin surface & superficial musculature. Save exam of identified tender areas until last. Determine if voluntary muscle guarding & involuntary rigidity. • 1. 2. 3. 4. 5. Abnormal Findings: Muscle guarding Rigidity Large masses Tenderness Involuntary rigidity is constant board like hardness of muscles. Deep palpation • 1. 2. 3. 4. Normal Findings: Same tech. as light palp., but push down 5-8 cm (2-3 in.) moving clockwise, exploring entire abdomen. To overcome resistance of very large or obese abdomen, use bimanual tech. Place two hands on top of ea. Other. Top hand does pushing; bottom hand is relaxed, concentrating on sense of palpation. Note location, size, shape, consistency (soft, firm, hard), surface (smooth, nodular), Mobility (including movement with respiration), pulsatility, tenderness • Abnormal Findings: 1. Tenderness occurs with local inflammation, with inflammation of peritoneum or underlying organ, & with an enlarged organ whose capsule is stretched. 2. Abnormal enlargement. 3. Tenderness. 4. Masses. Palpation of Liver • 1. 2. 3. 4. Normal Findings: Place left hand under person’s back parallel to 11th & 12th ribs and lift up to support abdominal contents. Place deeply down & under right costal margin. Ask person to take a deep breath. Normal to feel edge of liver bump fingertips as diaphragm pushes it down during inhalation. Feels like firm regular ridge. May not be palpable, may feel nothing. • Abnormal Findings: 1. Except for depressed diaphra, l liver palpated more than 1-2 cm below right costal margin is enlarged. 2. Record number in cm it descends & note consistency (hard, nodular), and tenderness. Palpation of spleen • 1. 2. 3. 4. Normal Findings: Normally spleen is not palpable, must be enlarged three times its normal size to be felt. To find, reach your left hand over abdomen & behind the left at 11th & 12th ribs. Lift up for support. Place right hand obliquely on LUQ with fingers pointing toward left axilla & just inferior to rib margin. Push hand deeply down & under left costal margin & ask person to take deep breath. You should feel nothing firm. • Abnormal Findings: 1. Spleen enlarges with mononucleosis and trauma. 2. Describe number of cm it extends below left costal margin. 3. When spleen is enlarged, it slides out & bumps fingertips. Can grow so large that it extends into lower quadrants. 4. May roll person onto right side to displace spleen more forward & downward. Palpation of kidneys • 1. 2. 3. Normal Findings: Search for right kidney by placing hands together in a “duck-bill” position at person’s right flank. Press two hands together firmly & ask person to take deep breath. In most people, feel no change. Occ. You feel lower pole of right kidney as round, smooth mass slide between fingers. Either is normal. Left Kidney sits 1 cm higher than right, not palpable normally. Locate by reaching left hand across abdom. & behind left flank for support. Push right hand deep into abdom. And ask person to breathe deeply. You should feel no change with inhalation. • 1. 2. Abnormal Findings: Enlarged kidney Kidney mass Palpation of aorta • Normal Findings: 1. Using opposing thumb & fingers, palpate aortic pulsation in upper abdomen slightly to left of midline. 2. Normally- 2.5-4 cm wide in adult, pulsates in anterior direction. • Abnormal Findings: 1. Widened with aneurysm 2. Prominent lateral pulsation with aortic aneurysm. Special procedures for abdominal palpation: • Normal Findings: 1. Rebound tenderness: (Blumberg’s Sign)-Assess when person reports abdom. Pain or when elicit tenderness during palpation. Hold hand perpendicular to abdom., push down slowly and deeply, lift up quickly. A normal, or negative response is no pain on release of pressure. • Abnormal Findings: 1. Pain on release of pressure confirms rebound tenderness, reliable sign of peritoneal inflammation. Murphy’s Sign (Inspiratory arrest) • Normal Findings: 1. Normally, palpating will cause no pain. 2. Ask person to take deep breath. Hold fingers under liver border. 3. A normal response is to complete deep breath without pain. • Abnormal Findings: 1. Positive test: as descending liver pushes inflamed gallbladder onto examining hand, person feels sharp pain & abruptly stops inspiration midway. Iliopsoas Muscle Test • Normal Findings: 1. Perform when acute abdom. Pain of appendicitis is suspected. 2. With pt. in supine pos., lift right leg straight up, flexing at hip, then push down over lower part of right thigh as person tries to hold leg up. 3. Negative test when pt. feels no pain • Abnormal Findings: • When iliopsoas muscle is inflamed (Inflamed or perforrated appendix), pain is felt in right lower quadrant. Obiturator Test • Normal Findings: • Test done when appendicitis is suspected. • With person supine, lift right leg, flexing at hip, and 90 degrees at knee. Hold ankle & rotate leg internally & externally. • Negative or normal is no pain. • Abnormal Findings: 1. Perforated appendix irritates the obturator muscle, producing pain. Developmental Considerations: • Normal Findings in the infant, child, adolescent, and aging adult: • Abnormal Findings: • Scaphoid shape occurs with dehydration in infant and child. Dilated veins. • Only one artery in umbilical cord in infant, inflammation, drainage after cord falls off. • Under 7 yrs., absence of abdom. Resp. occurs with inflammation of peritoneum. • Abdom. Rigidity with acute abdom. Conditions less common in aging persons. • Acute abdom, aging person complains of less pain than younger person.