NURSING CARE PREPARATION
advertisement

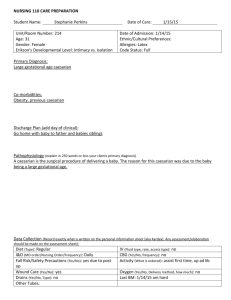
NURSING 111 CARE PREPARATION Student Name: Stephanie Perkins Unit/Room Number: PSU 377 Age: 81 Gender: Male Erikson’s Developmental Level: Integrity vs Despair Date of Care: 2/12/15 Date of Admission: 2/11/15 Ethnic/Cultural Preferences: White Allergies: NKA Code Status: DNR Primary Diagnosis: Acute respiratory failure Co-morbidities: Hx of CVA, dyspnea, COPD pneumonia Discharge Plan (add day of clinical): Integrated Pathophysiology (what is going on with your patient at the cellular level for the health condition, no more than three pages in length, including reference page) Fluid builds up in the alveoli sacs of the lungs which then causes a decrease of oxygen in the blood as evidenced by dyspnea. COPD correlates with this as it’s a chronic condition of fluid in the lungs which also causes dyspnea. Data Collection (Record exactly what is written on the personal information sheet [aka Kardex]. Any assessment/elaboration should be made on the assessment sheet): Diet (Type): Regular, vegetarian, mechanical soft I&O (MD order/Nursing Order/Frequency): no Fall Risk/Safety Precautions (Yes/No): Wound Care (Yes/No): Drains (Yes/No, Type): Other Tubes: IV (Fluid type, rate, access type): FS Sodium Chloride 0.9% 999 mL/hour over 1 H stat CBG (Yes/No, frequency): no Activity (What is ordered): Up for meals, up ad lib minimum 4 times daily Oxygen (Yes/No, Delivery method, how much): Yes 2-4 L/min NC Last BM: will assess day of clinical ASSESSMENTS (Include Subjective & Objective Data) Integumentary: Color appropriate for race, c/d/I, turgor present no wounds or lesions. Head and Neck: Normocephalic, nontender Ear/Nose/Throat: No drainage, nares patent, oral mucosa pink and intact. Mouth and tongue dry. Thorax/Lungs: Expiratory and inspiratory wheezes and rhonchi throughout lower lobes Cardiac: S1S2 heard but diminished. PP weak and easily obstructed no edema cap refill less than 3 sec Musculoskeletal: Grips equal bilaterally extremities strength equal bilaterally Genitourinary: Urine yellow no sediment or odor output 75 cc Gastrointestinal: Abdomen soft and nontender bowel sounds hypoactive in all 4Q Neurological: A/O x 3 PERRLA Other (Include vital signs, weight): BP 128/60 P 87 O2 100 Pain 0/10 RR 20 CURRENT MEDICATIONS List ALL regularly scheduled and prn medications scheduled on your client. (Due morning of clinical) Generic & Trade Name Classification Dose/Route/ Rate if IV Onset/Peak Intended Action/Therapeutic use. Why is this client taking med? Adverse reactions (1 major side effect) Nursing Implications for this client. (No more than one) Saline Flush (Sodium Chloride Flush) 0600 Albuterol/Ip ratrop (Duoneb) 0800 1200 Aspirin EC (Acetylsalicy lic Acid) 0900 Calcium Carb/Vit D (Caltrate/ Vit D) 0900 Chlorhexidi ne (Peridex) 0900 Enoxaparin (Levenox) 0900 Mupirocin (Bactroban) 0900 Paroxetine (Paxil) 0900 Maintenan ce Fluid 10 ml n/a IV patency Irritation Assess IV site Bronchodil ator 3 ml neb QID 5-15 min/0.5-2h Decrease airway resistance Worsening of breathing problems CPV assessment before and after treatment to determine effectiveness Nonnarcot ic Analgesic 81 mg 1 tab PO daily Unknown/1 5 min-2 h Pain relief of low to moderate intensity Thrombocytope nia Assess labs Fluid and electrolyte replaceme nt solution 1 tab PO daily Unknown/u nknown Calcium supplement Constipation Abdominal Assessment Germicidal 0.12% oral mouthwas rinse 15 ml h mucosal BID Anticoagul 40 mg=0.4 ant ml SC daily Unknown/u nknown Reduces bacteria in mouth Assess oral mucosa Unknown/ 3h Antithrombotic agent Severe irritation and chemical burns hemorrhage Antibiotic Not systemically absorbed 2 wk/ 5-8 h Rid of nasal bacteria Burning Assess for burning Treat depression Worsening depression Assess efficacy 2% Ointment Nasal BID Antidepres 20 mg= 1 sant tab PO Daily Assess labs Prenatal Vitamin w/ Iron 0900 Vitamin D 2000 unit 0900 Acetaminop hen (Tylenol) Albuterol HFA (Ventolin HFA) Albuterol neb sol (Ventolin Proventil) Nicotine Transderma l patch Ondansetro n (Zofran INJ) multivitam in 1 mg PO daily-meal Vitamin deficiency/supplem ent constipation Vitamin 2 tab PO daily Helps to absorb calcium and phosphorus Relieve pain none Nonnarcot ic Analgesic 2 tab PO q4h prn minor pain/HA Bronchodil 2 puff q 4 h ator prn wheezing/ SOB Bronchodil 3 ml neb ator q2h prn SOB 5-15 min/0.5-2h Smoking deterrent Antiemetic 1 patch prn nicotine cravings 2 ml IV q4h prn nausea vomiting Unknown/ 0.5-2 h Assess abdomen Acute renal failure in acute poisoning Assess labs Decrease airway resistance Worsening of breathing problems CPV assessment before and after treatment to determine effectiveness 5-15 min/0.5-2h Decrease airway resistance Worsening of breathing problems CPV assessment before and after treatment to determine effectiveness Unknown/ 8-9 h Reduce withdrawal symptoms of smoking Prevents n/v Localized edema Skin assessment Diarrhea Assess stools Unknonw/ 1-1.5 h DIAGNOSTIC TESTING Include pertinent labs [ABGs, INRs, cultures, etc] & other diagnostic reports [X-rays, CT, MRI, U/S, etc.] NOTE: Adult values indicated. If client is newborn or elder, normal value range may be different. Date 2/11 Lab Test Normal Values Patient Values/ Date of care Sodium 135 – 145 mEq/L Potassium 3.5 – 5.0 mEq/L Chloride 97-107 mEq/L Co2 23-29 mEq/L Glucose 75 – 110 mg/dL BUN 8-21 mg/dL 140 Creatinine 0.5 – 1.2 mg/dL Uric Acid Plasma 4.4-7.6 mg/dL Calcium 8.2-10.2 mg/dL Phosphorus 2.5-4.5 mg/dL Total Bilirubin 0.3-1.2 mg/dL Total Protein 6.0-8.0 gm/dL Albumin 3.4-4.8gm/dL Cholesterol <200-240 mg/dL Alk Phos 25-142 IU/L SGOT or AST 10 – 48 IU/L LDH 70-185 IU/L CPK 38-174 IU/L WBC 4.5 – 11.0 RBC 1.73 male: 4.7-5.14 x 10 female: 4.2-4.87 x 10 HGB male: 12.6-17.4 g/dL female: 11.7-16.1 g/dL HCT male: 43-49% female: 38-44% MCV 85-95 fL MCH 28 – 32 Pg MCHC 33-35 g/dL RDW 11.6-14.8% Platelet 150-450 Interpretation as related to Pathophysiology –cite reference & pg # 4.7 108 Renal failure not being able to excrete chloride 24 97 32 Renal failure not being able to excrete waste product Severe renal impairment n/a 9.2 n/a 0.6 8.3 dehydration 3.7 n/a 97 26 n/a n/a 9.8 3.82 Hemolytic anemia 11.6 Hemolytic anemia 35.2 Decrease in number or RBC 92 30.4 33.0 14.2 189 DIAGNOSTIC TESTING Date UA Normal Range Results Interpretation as related to Pathophysiology –cite reference & pg # Results Interpretation as related to Pathophysiology –cite reference & pg # Color/Appearance pH Spec Gravity Protein Glucose Ketones Blood Date Other (PT, PTT, INR, ABG’s, Cultures, etc) Normal Range ++++++ Date Radiology X-Rays Scans EKG-12 lead Telemetry Results Interpretation as related to Pathophysiology –cite reference & pg # DAR NURSING PROGRESS NOTE Include the same note that was written in the client record for the priority nursing diagnostic statement. Include the date/time/signature. 2/12/15 1230 Patient up in wheelchair. Lung sounds diminished, inspiratory and expiratory wheezing. Rhonchi and crackles present. Assisted in ordering lunch and in feeding. During feeding pt coughed after every bite. Inquired about denture use and pt stated “they’re too expensive”. Called for speech therapy consult for a swallow study which lead to diet change of mechanical soft and thick liquids with thin liquids between meals. Left pt with call light in reach, brakes on, O2 at 3 L-------------------------------------------------------------------------Stephanie Perkins SN PATIENT CARE PLAN Patient Information: Nursing Diagnosis should include Nanda Nursing Diagnostic statement, related to (R/T), as evidenced by (AEB). Problem #1 Impaired gas exchange r/t lung disease AEB dyspnea Desired Outcome: Patient will not experience s/s of dyspnea at rest during shift Nursing Interventions Client Response to Intervention 1. Assess CVP q 2 h 1. Inspiratory and Expiratory wheezing and rhonchi with crackles 2. Encourage use of incentive spirometer q1h 2. Able to get to 750 3. Educate proper use of inhalers every administration 3. n/a RT did all nebulizer treatments Evaluation (evaluate goal & interventions, what worked/what didn’t, what would you adapt if needed): This pts lung sounds were absolutely horrendous. He was able to use the incentive spirometer a few times and I educated him on how to use it correctly. I did leave it on the bedside table as well to serve as a visual reminder. I think these interventions worked well minus the inhaler/neb treatments since RT did all of those. I hope that throughout his stay the other RNs and CNAs do similar interventions to help him get better. Problem #2 Risk for Aspiration r/t swallowing difficulties AEB coughing during meal time. Desired Outcome: Patient will not show s/s of aspiration during meal time (i.e. coughing, gagging, etc.) Nursing Interventions Client Response to Intervention 1. Assess lungs before and after meal time 1. Lung sounds unchanged before and after meal, however lots of food in back of throat after swallowing 2. Assess for s/s of aspiration during meal time 2. Coughed during and after mealtime 3. Consult for swallowing evaluation 3. Diet was changed to mechanical soft and thickened liquids with thin liquids between meals Evaluation (evaluate goal & interventions, what worked/what didn’t, what would you adapt if needed): Assessing the lungs before meals helped establish a baseline so if there was an aspiration I had something to look back on. He did cough during the mealtime so that’s why I had speech therapy evaluate his swallowing. During the evaluation it was discovered that he’s a silent aspirator so his diet was changed to prevent aspiration pneumonia. In all I think these interventions worked well to help him in the future. Problem #3 Activity intolerance r/t lung disease AEB dyspnea Desired Outcome: Patient will walk at least 50 feet 4 times during shift Nursing Interventions Client Response to Intervention 1. Assess extent to which pt is able to move around 1. Pt weak, able to transfer from bed to in room at beginning of shift wheelchair with 1 person assist 2. Encourage patient to walk 50 feet 4 times during shift 3. Educate patient about controlled breathing during activity 2. Unable to walk d/t weakness 3. O2 stats raised during deep breathing exercises Evaluation (evaluate goal & interventions, what worked/what didn’t, what would you adapt if needed): Besides the walking the other interventions worked. This pt had tried to adjust himself in bed and in doing so his O2 stats dropped significantly from 92 to 85. The deep breathing exercises helped bring his O2 stats back up to 92.