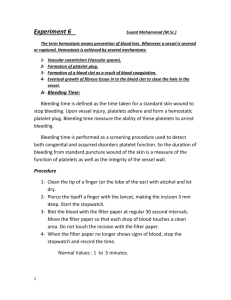
Haem Module 1
advertisement

1.1 – INITIATION OF COAGULATION 1. Tissue factor is the primary initiator of coagulation Structure of TF 47kDA integral membrane protein Is the only pro-coagulant factor that does not require proteolytic cleavage for activation Physiology of TF normally located on extravascular sites, namely on CSMs of VSMCs & Fibroblasts Is at higher concentrations on cell surfaces in certain organs to provide extra haemostatic protection (lungs, brain, gonads, placenta) TF has 2 functions Acts as a cellular receptor is the cofactor for factor 7/7a 2. Factor 7/7a has the typical Gla-egf-Ser domain structure Structure of F7 48kDa zymogen Gla domain – binds (Vitamin K dependent factors) to activated phospholipid membranes (i.e. PPDserine on outer surface) Serine protease domain – contains catalytic triad of his/asp/ser which cleaves after arg or lys Physiology of F7 secreted by the liver into plasma at concentration of 10nM ~10% of this is (for reasons unknown) circulating as F7a o the circulating F7a is largely inactive unless bound to TF 3. the TF-7a complex is key for the initiation of coagulation Structure/Function of TF-7a TF binds to F7a on subendothelial CSM and allosterically activates serine protease domain o the reaction has a very high affinity (Kd < 1nM) all 4 F7 domains interact with TF due to low F7a concentrations, only a small amount of TF can form the TF-7a complex at first o TF-7a can auto-activate (via proteolysis) other TF-F7 complexes 10a can also do this Initiation of coagulation involves generating small amounts of thrombin by TF-7a TF-7a activates (via proteolysis) F9 by cleaving after Arg 145 and Arg 180 TF-7a activates F10 by cleaving after Arg 191 F10, without its cofactor (F5) generates trace amounts of thrombin by cleaving prothrombin o Thrombin cleaves 8 8a o Thrombin cleaves 5 5a F9a-8a activate F10; F10a-5a cleaves prothrombin much more efficiently o hence propaogation of coagulation becomes independent of TF-7a 4. there are different forms of TFPI, each with their own roles in the regulation of coagulation Structure of TFPI 43kDa molecules acidic (-ve) N terminus and alkaline (+ve) C terminus Has 3 kunitz domains o Kunitz 2 inhibits 10a o Kunitz 1 inhibits TF-7a Physiology of TFPI The majority (80%) of TFPI is cellular: o extravascular (VSMCs etc) o endothelial o platelet Cellular TFPI is either stored and released upon demand or bound to cell surfaces. TFPI-beta is a type of membrane bound TFPI made by alternative mRNA splicing The remaining (20%) circulates free in the plasma. of this proportion, most is truncated by binding to lipoproteins, and only ~0.25nM is at its full length and active Functions of TFPI TFPI uses its own Arg and Lys residues at ‘P1’ regions on the Kunitz domains to act as mock substrates for 10a and TF-7a respectively The interaction with 10a comes first after it has dissociated from subendothelial membrane. this interaction is usually slow as the concentration of active TFPI in the plasma is low o Protein S increases the rate of the first step by binding 10a to phospholipid surfaces o TFPI-beta can then bind 10a to phospholipid surfaces, which reduces dependence on protein S the subsequent interaction between TFPI-10 and TF-7a forms an inactive quarternary complex Roles of TFPI during coagulation Extravascular TFPI regulates the very 1st step of coagulation initiation at subendothelial sites endothelial TFPI localises coagulation to the site of injury and prevents spread of the plug to neighbouring/distant sites Platelet TFPI regulates TF in a developing haemostatic plug (and possibly microparticles) Plasma TFPI regulates TF-7a at all sites (and possibly microparticles) 5. TF microparticles are a controversial issue, but if they do exist they offer a different model of coagulation propagation Idea behind microparticles It is very difficult for circulating factors to get through the fibrin meshwork in a growing plug Experiments have shown that [TF] increases at site of injury as the haemostatic plug forms o Hence circulating TF may be another mechanism which propagates coagulation it is thought that microparticles, derived largely from monocytes, express TF and circulate in the plasma Microparticles bind to P-selectin on activated platelets and/or endothelial cells via PSGL binding is thought to ‘decrypt’ this TF, initiating coagulation all over again Evidence suggests cancer patients have higher circulating microparticles, which could account for their pro-thrombotic state if being produced by tumour cells. 6. Knockout studies in mice have shown that factors in initiation coagulation are key to survival Factor knocked out TF F7/10 TFPI Result Death in utero haemorrhagic death after birth death in utero F7 and F10 can cross the placenta 1.2 – FIBRINOGEN, FIBRIN & FIBRINOLYSIS 1. Fibrinogen is the product of multiple genes Fibrinogen Structure fibrinogen is encoded by 3 coding genes on chromosome 4 (gamma, alpha, beta in direction of transcription) The resulting molecule is symmetrical; 2 of each chain connect terminal D domains to a central E domain the whole protein is roughly 350kD big fibrinogen is soluble (polymerised and cross linked fibrin are not) Fibrinogen physiology It is an acute phase protein so transcription is induced by pregnancy, inflammation, steroids The central E region contains the key peptides, FpA & FpB which thrombin cleaves 2. cleavage of fibrinogen by thrombin produces monomers that spontaneously polymerize Thrombin cleaves the alpha chain between arg16 and gly17 (at FpA) to expose the polymerisation domain 17-20 Thrombin also cleaves the beta chain between arg 14 and gly15 (at FpB) to expose its polymerisation domain (15-18) D domains on fibrinogen always have an exposed polymerisation domain hence, the cleaved E domains polymerise with D domains on other molecules to form a ‘halfstaggered’ fibrin clot gamma chains also interact linearly 3. Thrombin activates F13a, which is key in cross-linking fibrin polymers Structure of F13 Only transglutaminase enzyme involved in coagulation exists as a tetramer (320kDa) Physiology of F13 Circulates in plasma bound to the d-domain of fibrinogen thrombin cleaves the activation peptide of F13 on the surface of the fibrin clot o this is much more efficient than thrombin-F13 in vitro F13a uses calcium ions to create covalent (isopeptide-gamma-glutaminyl-epsilon-lysyl) bonds between adjacent fibrin polymers o this cross linking usually occurs between lysine and glutamine residues (lysine acting as an acid/ electron donor) cross linking between gamma chains occurs first, then alpha chains 4. One of the functions of fibrin it to provide the trigger for its own dissolution Functions of fibrin provides mechanical meshwork/matrix for wound repair supports platelet adhesion/aggregation provides trigger for its own dissolution (fibrinolysis) Initiation of Fibrinolysis is driven by fibrin by two major mechanisms Plasminogen is a zymogen synthesised in the liver. tPA is expressed by endothelial cells. It circulates as an active enzyme with low intrinsic activity. o Both plasminogen and tPA bind to fibrin via lysine residues on fibrin kringle domains o this brings plasminogen & tPA into close contact and thus reduces the (Km) minimum concentration of plasminogen required for a reaction to occur Fibrin also directly enhances tPA (increased Vmax for reaction) Fibrin enhances tPA to cleave plasminogen on the surface of fibrin to produce plasmin o Another plasminogen activator, uPA is involved extravascularly and is not influenced by fibrin. uPA is involved in extraceullar matrix degradation (which contributes to cell motility) and growth factor activation via plasmin 5. Plasmin is the key molecule in fibrinolysis. Its broad specificity highlights the need for antiplasmin and other anti-fibrinolytic molecules Plasmin has broad substrate specificity and cleaves after lysine and arginine residues Plasmin breaks fibrin into ‘D-dimers’; it has the ability to break 50-60 bonds at once Plasmin generated by uPA can activate other proteases and cellular growth factors hence plasmin is implicated in a wide arrange of disease o tPA plasmin – CVS disease, atherosclerosis o uPA pasmin - cancer Anti-fibrinolytic molecules Antiplasmin Plasimogen-activator-inhibitors 1 & 2 (tPA inhibitors) o these are both serine proteases Thrombin-activated-fibrinolysis-inhibitor (TAFI) o carboxypeptidase enzyme which removes lys or arg residues from C-termini of fibrin to prevent it from stimulating tPA o hence, when thrombin binds to thrombomodulin, it is not only an anti-coagulant (protein C) but also an anti-fibrinolytic (TAFI) 6. Synthetic plasminogen activators have therapeutic uses thanks to their fibrinolytic properties tPA (alteplase) used in MI, stroke, PE Streptokinase (bacterial product which stimulates plasminogen and causes plasmingoen to act like tPA) used in MI, VTEs and arterial thrombi TNKase (tenecteplase) is a synthetic tPA with a longer half life and greater bioavailiability used in MI Desmodus rotundus PA (from bats which use it to keep sucked blood liquid) for stroke uPA used for MI/PE 1.3 – ANTITHROMBIN & HEPARIN 1. Antithrombin is the key anti-coagulant molecule in the termination of coagulation Structure of antithrombin 8kDa serine protease Has 3 main ‘parts’ to the molecule – the main body, a bait loop, and a helical area for GAG/heparin attachment Physiology of Antithrombin Circulates in plasma at higher concentration than most coagulation factors effectively inhibits free circulating serine proteases, but principally Thrombin and F10a Its action is enhanced by endogenous heparan sulphate (GAGs) and exogenous heparin, both of which have a similar structure 2. Antithrombin inactivates thrombin by use of a ‘moustrap’ mechanism Antithrombin is inactive when its ‘bait loop’ is partially contained within the main body of the molecule The active conformation exposes P1 residues on the bait loop P1 residues bind to thrombin covalently and irreversibly o the ‘captured’ thrombin has its structure changed so it loses functionality o the T-AT complex is subsequently cleared from the bloodstream Some thrombin molecules can cleave the bait loop, if this is successful they are not captured and the antithrombin molecule is rendered inactive 3. Heparan Sulphate and Heparin have similar structures and both stimulate antithrombin Heparan sulphate is present on the surface of endothelial cells Heparin is stored in mast cells (and rarely ‘sees’ bloodstream) and can be administered in a number of different formulations relating to molecular weight Both molecules are compromised of repeating disaccharide residues of D-glucosamine and one of uronic or iduronic acid. the major difference between the two is that Heparin contains an essential pentasaccharide sequence, which is not fully developed (/sulphated) in heparan sulphate Mechanism of action of heparin heparin pentasaccharide binds to helical area and causes antithrombin to adopt active conformation o this is enough to inhibit 10a Longer heparins (>18 saccharides) form a bridge between the helical area and a thrombin molecules = inhibition of thrombin Heparin dissociates after 10a/thrombin is bound; catalyst 4. The length/Mr of heparins determines their anticoagulant function and hence clinical use Unfractionated heparin (Mr>6000) can inhibit both thrombin and 10a Low molecular weight heparins (1500-6000) will inhibit both 10a/thrombin in a ratio determined by the specific length (shorter ones inhibit more 10a and vice versa) Heparins with a Mr<1500 (eg Fondaparinux) are essentially just the pentasaccharides i.e indirect anti-10a molecules Low Molecular weight heparins are useful in clinical practice They have a high anti 10a and anti-thrombin activity (better than heparins <1500) LMWH have better bioavailability than Unfractionated heparin hence are more predictable in their course of action LMWH have reduced interaction with neutralising proteins which leads to less heparininduced thrombocytopenia They are mainly used prophylactically and therapeutically in VTE, as well as: o treatment of arterial thrombosis o cardiovascular catheterisation o haemodialysis o DIC 1.4 – INTRODUCTION TO THROMBOPHILIA 1. Venous thromboembolism is a disorder predisposed to by a number of genetic and environmental factors The key notion is that most people with recurrent VTE disease have a transient risk factor which pushes them over their thrombotic threshold in the context or pre-existing genetic and/or environmental predispositions to clot. Genetic AT deficiency Protein C def Protein S def F5 leiden PT G20210A Environmental Antiphopholipid syndrome Myeloproliferative disease Increasing Age Previous Thrombosis Cancer Mixed Hyperhomocysteinaemia High F7/9/ fibrinogen Transient Surgery Long distance travel OCP HRT pregnancy 2. An important polymorphism is Factor V leiden confers resistance to activated protein C Normal physiology APC cleaves the 5a heavy chain in two places on phospholipid membranes of platelets and endothelial cells to inactivate it - the two places where APC splices are Arg 506 & Arg 306 Arg 506 is rapidly cleaved and cleavage makes 5a moderately less active Arg 306 is slowly cleaved and cleavage makes 5a completely inactive F5 leiden A common single polymorphism occurs at 506 Arg Gln this polymorphism is likely to have been a ‘founder’ polymorphism that has since spread amongst Europeans in particular this stops rapid cleavage of 5a and confers resistance to activated protein C slow cleavage at Arg306 still occurs F5 leiden polymorphism interacts with other genetic/environmental pro-thrombotic predispositions Genetic – F5 leiden (homozygosity), Protein C/S def, AT def, PT G20210A Environmental – OCP 3. An important polymorphism in prothrombin confers increased thrombotic potential The G20210A polymorphism increases prothrombin production, which subsequently increases thrombin production = thrombosis. 4. Polymorphisms are more common and have less thrombotic potential than single gene mutations Single gene mutations are implicated in AT def, Protein C def and Protein S def Homozygotes for single gene mutations tend to be severely disabled or die in utero. Heterozygotes do not have increased mortality but may experience the following symptoms due to increased risk of thrombosis: Common – DVT/PE/ pregnancy associated thromboembolism Rare – warfarin induced skin necrosis, clotting in other veins (i.e not legs) and arteries o warfarin inhibits protein C/S so if the person is already deficient then the drug makes the problem worse F5 leiden and PT G20210A are atleast twice as common but have half the thrombotic risk 1.5 – UNDERSTANDING ENZYMES IN HAEMOSTASIS 1. Km & Kcat are important measure of enzyme function (Michaelis Menten mechanism) Km = the [substrate] at which the reaction is catalysed at ½ Vmax also known as the dissociation constant of an enzyme substrate complex (i.e. at equilibrium/ Km; half substrate will have reacted and half will not) A low Km value denotes a high affinity If the Km value is >[substrate] the reaction will not occur Units = M (nm microM etc) Kcat = is the number of times the enzyme reacts with the substrate per second also known as turnover No; proportional to Vmax Units = s-1 Kcat/Km = specificity constant and is a measure of catalytic efficiency Units = s-1M-1 in haemostasis this should be of the order >106 2. Surfaces and cofactors have predictable effects on Km & Kcat Surfaces bring reagents together. This reduces the substrate concentration for the reaction to occur (less reaction-by-chance) This reduces Km = increases affinity Shifts reaction curve left but same Vmax is reached Cofactors cause conformational changes in substrates which make them more reactive This increases Kcat = increased Vmax This may also reduce Km = increased affinity AN INCREASE IN ENZYME CONCENTRATION DOES NOT CHANGE Km This change only increases Vmax hence the 1/2Vmax value is faster, but occurs at the same substrate concentration as before 2. Activation of Prothrombin, Plasmin and antithrombin are all important examples of how enzymes make sure reaction only happen where they are supposed to Prothrombin Thrombin is catalysed by 10a 5a is the cofactor for 10a (increases Kcat) Platelet phospholipid is the surface (reduces Km) o Prothrombin concentration is low in plasma. this reaction would not occur if it weren’t for phospholipids Km would be too high. Plasminogen Plasmin is catalysed by tPA Fibrin is the cofactor for tPA (increases Kcat) and the surface (reduces Km) Thrombin antithrombin/thrombin complex is catalysed by Antithrombin Heparan Sulphate is the surface (reduces Km), but also increases Kcat slightly COFACTORS AND SURFACES ACT AS ENHANCING MECHANISMS FOR REACTIONS AND AS REGULATORY MECHANISMS MAKING SURE REACTIONS HAPPEN WHERE THEY ARE SUPPOSED TO 1.6 – WON WILLEBRAND FACTOR 1. vWF factor is the largest circulating protein in human plasma Structure of vWF Large (upto 20000kDa) multimeric glycoprotein Largest molecules bind to subendothelial collagen with greater affinity and have greatest pro-thrombotic ability Physiology of vWF Majority is synthesised by vascular endothelial cells o Expression is highest in brain, lungs and heart (greater haemostatic protection) o expression seems to be higher in venous endothelium than in arterial Minority is released from alpha granules on platelet activation o thought to be a compensatory mechanism if there is a lack of endothelial vWF Plasma levels vary greatly o low in blood group O (ADAMTS13 susceptibility) o increased during preganancy/ birth and possibly with ageing o Wiebel-Palade body release from endothelial cells is stimulated by stress, inflammation, DDAVP 2. the vWF monomer has a number of important domains relating to its function Domain D1-D2 D’-D3 A1 A2 A3 C1 CK Function Propeptide, multimerisation F8 binding, multimerisation Gp1b (platelet) ADAMTS13 (regulation) Collagen 3 (subendothelium) GP2b3a (activated platelet) dimerisation (ER) 3. vWF undergoes extensive post-translational modification Intracellular Modification ER – N linked glycosylation & dimerisation o Dimerisation is achieved by disulphide knots via CK domains. the propeptide acts as a catalyst for this because it has disulphide isomerise activity. o diemerisation is the cue for peptide to leave ER (not enough space in ER for multimers) Golgi – O linked glycosylation & start of multimerisation o multimerisation achieved via d-domains Post-golgi – addition of ABO blood sugars (vWF is the only circulating protein that expresses ABO) Wiebel-Palade Bodies store large vWF Most vWF are transiently stored in these and subsequently released, a small proportion remain intracellular to be released on a stimulus (eg stress, DDAVP) WPBs are only found in endothelial cells (hence can act as a marker for these [+CD34]) vWF’s propeptide induces WPB formation (+ve feedback) WPBs contain other molecules involved in adhesion (p-selectin) and F8 Extracellular modification Furin removes the propeptide (some of this happens intracellularly) The resulting vWF can adopt either a globular or linear structure. the linear structure exposes binding domains. 4. The primary role of vWF is in primary haemostasis – making GP1b its most important protein Shear Stress and endothelial binding forces globular vWF to unfold Shear stress from blood flow will cause vWF to spontaneously unfold/refold whilst circulating in the plasma due to varying blood speeds (?threshold for unfolding in 5000s-1) Similarly, when vWF binds to sudendothelial collagen, one end is anchored and shear stress subsequently unfolds the rest of the molecule, exposing binding sites o vWF binds to subendothelial collagen type 3 via its A3 domain (A1 binds to different collagens). A1-GP1b binding slows platelets down and RGD-2b3a binding fixes them vWF-A1 domain binds to Gp1b on platelets – forcing them to slow down in circulation o this bond is rapid on-rapid off (high dissociation rate) platelets roll along vWF under torque of blood flow and become activated o hence platelet-GP2b3a becomes activated o platelets also degranulates – initiating aggregation vWF uses RGD sequence on its C1 domain to bind to 2b3a and fix platelets 5. the secondary role of vWF is in coagulation as a carrier of F8 F8 and vWF circulate as a complex in plasma. complex formation is rapid. o the complex dissociates once F8 is activated by thrombin vWF protects F8 from degradation from activated protein C, prevents premature association with F10 & hence increases its half life defect of vWF-F8 binding = Type 2N vWD 6. The functions of vWF are regulated by the MMP ADAMTS13 By cleaving large vWF molecules, ADAMTS13 prevents excessive clotting that would be otherwise associated with lots of large circulating vWF molecules. TTP is associated with low ADAMTS13 Proteolysis is enhanced by elevated shear stress, type 2A vWD and deanaturants like urea because these all unfold vWF and lead to exposure of the A2 binding site for ADAMTS13. Blood group O is more sensitive to ADAMTS13 cleavage because vWF expresses no ABO sugars, which provide a degree of resistance to cleavage in blood groups A/B/AB. 7. vWD is a quantitative/qualitative deficiency on vWF The hallmark is prolonged bleeding time and ?APTT (haemophilia would not prolong bleeding time) it is a defect of primary haemostasis (impaired platelet binding) and coagulation (F8 ‘deficiency’) High circulating vWF may be implicated in cardiovascular disease (stroke, MI). Anti 2b-3a is used therapeutically in CVD in reproductive medicine. 1.7 – POST-TRANSLATIONAL MODIFICATION OF COAGULATION FACTORS 1. Glycosylation is an important post-translational modification Involves covalent attachment of a glycan to a protein different cell lines produce different glycosylation patterns, which makes it difficult to make synthetic fully functioning coagulation factors alterations in glycosylation patterns are observed in a variety of pathologies there are two types of glycans: o Linear (GAGs) o Branched N-linked O-linked N-linked O-linked attaches to aspargine as part of a N-X-S/T triplet attaches n-acetylgalactosamine to threonine or where X is any AA except for proline serine residues not truly post-translational; occurs in ER occurs in Golgi – true post translational involved in protein folding, bond stability, less well understood – provide stability and may solubiolity, protection for proteolysis, clearance have roles in clearance 2. N & O linked glycosylations play important roles in the function of vWF Importance of N Linked glycosylations (NLG) – 12sites on vWF Formation of vWF dimers/ multimers o inhibition of NLG = retention of monomeric vWF in endothelial cells Disulphide bond formation = maintenance of globular structure of vWF o inhibition of NLG = ‘early’ exposure of binding sites = tendency to clot Presenting ABO blood sugars o inhibition of NLG = increased cleavage of ADAMTS13 Importance of O linked glycosylations (OLG) – 10sites on vWF OLG has a tetrsaccharide t antigen whose plasma concentration is inversely proportional to vWF Inhibition of vWF A1-Gp1b binding o Inhibition of OLG = increased binding and tendency to clot Steric hindrance increases stability of molecule Protection of ADAMTS13 o Inhibition of OLG = increased clearance vWF without a terminal sialic acid is cleared more quickly from bloodstream because of increased affinity to ASGRP receptor; sialic acid protects VWF against proteolysis by serine and cysteine proteases but specifically enhances susceptibility to ADAMTS13 proteolysis 3. importance of glycosylatons in other clotting factors F& - has 2 N- & 2O glycosylation sites which are important for normal secretion F8 – glycans are important for interaction with chaperone proteins in ER F9 – recovery, activity, efficacy 4. importance of gamma-carboxylation occurs on glutamic residues of Gla domains on F2,7,9,10, Protein C/S the catalysing enzyme, gamma-glutamyl carboxylase is vitamin K dependent warfarin blocks recycling of Vit K = impaired gamma carboxylation = impaired binding of factors to platelet phospholipids due to inability to bind calcium 1.8 – MOLECULAR MODELLING WORKSHOP 1. Why protein structures are important SHAPE DETERMINES ACTICITY. KNOWLEDGE OF SHAPE = Understanding the effect of gene mutations o Protein structures allow you to see the location of a missense mutation. o A mutation in the core of a domain often leads to misfolding, a failure to secrete protein from the cell and therefore low plasma level. (Type I mutations: most common) o Some mutations cause disease because they are in a functionally important part of the protein (Type II mutations: less common). Understanding how drugs affect enzymes Understanding research papers Essential tool in research 2. How protein structures are derived X-ray crystallography • high resolution but need large sample size, time consuming and gives static picture NMR (nuclear magnetic resonance) Spectroscopy • high resolution and gives information about mobility but protein needs to be soluble and not good for large molecules (size limited) Homology modelling (prediction of structure) • involves using homolgous proteins as templates as a last resort basically • medium resolution (limited accuracy)and structure of homologus protein needed using computer algorithms to predict structures when all else fails 3. 4. What is being shown in protein molecular graphics pictures of different types What you can do with molecular graphics Show representations of molecules in different presentation styles, colours &c Explain functional features (e.g. enzymatic activity or receptor binding) at molecular level Qualitatively interpret amino acid substitutions (missense mutations) in disease states Hypothesise about unknown structures or interactions Explain functional features (e.g. enzymatic activity or receptor binding) at molecular level 4 types of molecular graphics: • Ball and Stick • can view interior of molecules but only gives partieal view (no sense of density) • Secondary Structure • good view of domains but no representation of surface • Spacefill • good view of surface but cant see inner structure • Surface representation • accurate and realistic • can show charge/ surface hydrophobicity 5. What you need to produce your own molecular graphics 6. To download a structure from the PDB Database and produce a graphic in Pymol. 1.9 – RARE COAGULATION DISORDERS 1. Coagulation disorders apart from haemophilia are very rare and are classified based on severity Haemophilia A/B and vWD account for 97% of all inherited coagulation disorders Incidence - Haemophilia A 1/10k o Haemophilia B 1/50k o F7 def is the most common of the others – order is 1/500k o The others are about 1/million Inherited disorders of primary haemostasis eg Glanzmanns are of the order 1/million Most rare bleeding disorders are classified based on severity An assay reading of less than 1 IU/dL is deemed as an absence Heterozygotes (>20) may still have a bleeding problem <20IU = homozygote/compound heterozygotye o a compound heterozygote is someone who has inherited to different mutant polymorphisms <10IU = homozygote Type 1 disorder = absence. Type 2 disorder = dysfunction The concentration of coagulation factor required for haemostasis to occur is much lower than the lowest boundary of the normal range. Hence bleeding severity vary rarely correlates with deficiency (except for fibrinogen, f10, f13), bleeding patterns are variable, and heterozygotes/carriers may still have bleeding problems. 2. The majority of rare coagulation disorders follow an autosomal recessive inheritance and demonstrate largely unpredictable bleeding patterns Factor Deficiencies Fibrinogen (AD) Type 2> Type 1; majority of Type 2 are acquired eg Liver dx PT/F2 Rarest of them all Always fatal F5 F5+F8* F7 Type 1> type 2 Always fatal F10 F11 (AI) F13 Result of absence Not fatal Commonest of them all (Arg353G mutation & environmental influences cited) Always fatal Particularly common in Ashkenazi jews (f7 levels low in liver dx, preg) Bleeding ‘pattern’ PT APTT TT Umbilical cord, oral, muscle/joint, nose, periods. Thrombosis if mutation near to thrombin cleavage site Nose, periods, oral, muscle/joint Nose, periods, oral Nose, periods, oral (mild) Nose, periods, oral - - + + + - + + + + + - - Joints, GI/urinary Genitourinary, oral, nose, tonsils (injury related; mild) Umbilical, intracranial, miscarriages, impaired wound healing + - + + - - - - *Combined F5/F8 deficiency is not due to mutations in the genes but due to problems in intracellular traifficking 3. The management of rare bleeding disorder is difficult Rare disease = limited expertise and resources Haemophilia centres will usually cover these patients FFP/Promthrombinase concentrates (PCC )are usually the only resource, recombinant factors are being developed but they are expensive and the market is very narrow. Adjuvants like TAFI, DDAVP, OCP, IUCD can be used Offer advice to communities where consanguinuity is more common (AR diseases) 1.10 – LABORATORY TESTS OF COAGULATION 1. Patients usually bleed because of defects in their procoagulant activity i.e. having an inherited excess anticoagulant/ fibrinolytic activity is rare Low Procoagulant activity can be qualitative or quantitative Type 2; Qualitative – poorly functioning protein - usually inherited Type1; Quantitative – low circulating protein – usually inherited but acquired causes included liver failure, excess consumption (DIC), drugs (warfarin) 2. PT & APTT are practical screening tests but not unphysiological PT initiates coagulation via Thromboplastin (TF) until thrombin is generated. Normal range 9.6-11.6 Elongated in extrinsic/ common pathway deficiencies APTT works in the same way but uses partial thromboplastin in the presence of a contact activator eg kaolin, silica, elagic acid, glass Normal range 26-32 Elongated in intrinsic/common patway deficiencies TT uses a small amount of thrombin to measure the time taken to convert fibrinogen into fibrin. Normal range 15-19 Elongated in a/dysfibrinoginaemias, heparin (and other thrombin inhibitors) Unphysiological nature of coagulation tests aptt seems to be sensitive to F12 which we know plays little part in coagulation in vivo – false positive they do not have appropriate sensitivity for factors that we know play bigger roles – false negatives they do not detect a number of disorders eg vWD, platetlet disorders, vessel wall/ fibrinolytic disorders different reagents in different labs mean that the results are not standardised 3. Antigenic assays and functional assays are being used for specific factor deficiencies Antigenic assays are precise but give only quantitative (not qualitative) data ELISA is the assay usually used – the principle is catching the antigen with one antibody and measuring the titre using another, labelled antibody o Time consuming Immunoturbidimetric assays use reactions that create agglutination and shine a light through the solution to measure a change in light intensity at a sensor The specificity of antigen-antibody reactions means that antigenic assays are not prone to interference Functional assays are imprecise but are more reflective of coagulatory function to an extent One stage clot based assays compare the test plasma to a standard one by adding each solution to a factor-deficient plasma. Time to clot vs Dilution is plotted on a graph and then you can say how ‘dilute’ the test is in comparison to the standard for that given clotting factor. Chromogenic activity assays use a chromogenic substrate which is cleaved by the factor of interest to produce colour. These may be more reproducible than clot based assays but are not always physiological Subject to interference PFA100 is a useful assay in measuring primary haemostasis Bleeding time used to be used – but this is no longer the case because it has poor sensitivity, specificity, reproducibility and poor predictive value PFA 100 forces blood through a collagen-lined aperture. Blood flow is terminates when a haemostatic plug is formed. o Sensitive to platelet number, function, vWF function & Hct o But not sensitive to Thrombin, drugs (clopidogrel) i.e. haemophiliacs would have a normal PFA-100 test; you would need another test for coagulation disorders in conjunction with this 4. Laboratory tests can be misrepresentations of the clinical sample Variables that are due to the sample Some clotting factors (8, vWF) are acute phase proteins that can be induced by stress Collection of blood may have been inadequate o Fill blue bottles to the top – need to ensure anticoagulant volume does not dilute sample o Haemolysis Transport to laboratory should not exceed half life of clotting factor Centrifugation & storage are different depending on where you are Variables that are due to computers/analytical machines Computers usually use electrical- or light-transmission based methods to analyse concetrations Automation is good because it increases throughput of samples, has good reproducibility The bad parts of automation is that they are susceptible to end point errors (i.e if the end point takes part in the initial reaction) and can introduce artefact 1.11 - HAEMOPHILIA 1. There are broad patterns of bleeding concerning primary and secondary haemostatic defects Primary haemostatic defects essentially cover platelet disorders and vWD Vessel wall & collagen disorders are also in this bracket, but are comparatively rare Bleeding is from small vessels, involves no delay and doesn’t stop Secondary haemostatic defects are usually due to procoagulant deficiencies Haemophilia is the commonest Heaprin therapy may produce a similar type of bleeding Bleeding is from deep structures, involves a delay (the time in which the plug is stable; before it breaks apart) and doesn’t stop from then on Fibrinolytic disorders are rare 2. The genetic basis of haemophilia concerns an inversion mutation of chromosome X Female carriers are not safe Circulating factor levels in women are extremely variable A carrier may display very low circulating F8 and then experience symptoms Conversely, a female may have high circulating F8 but is obviously not homozygous for the disease. The inversion mutation causes 45% of severe haemophilia A cases The mutation tends to occur in spermatogenesis Essentially, two homologus regions on the X chromosome recombine to give a gene that is subsequently un-transcribable A number of other polymorphisms have been implicated in haemophilia A & B (B is not associated with the inversion phenomenon) Some patients produce antibodies against F8/9 3. The pathogenesis of haemophilia involves the inability to generate a thrombin burst Lack of either factor 8/9 means that the propagation stage of coagulation cannot occur Failure of a thrombin ‘burst’ in haemophilia slow thrombin generation = weak, unstable platelet aggregate The platelet aggregate will break due to lack of fibrin production NO factor 13 cross linking = any fibrin generated is insecure NO TAFI activation = any fibrin generated is more prone to fibrinolysis 4. Haemophilia is particularly prone to bleeding in joints and muscles Haemophilia A & B are clinically indistinguishable. It was discovered thatthey were different diseases when two patients (one A one B) could cure each others’ clotting abnormality. Classification of bleeding in Haemophilia Severe (factor level <1%) o Spontaneous bleeding, from joints/muscles, which is delayed but prolonged. Moderate (factor level 2-5%) o Prolonged/excessive bleeding after minor trauma Mild (factor level 6-40%) o Prolonged bleeding after major trauma and/or surgery HAEMOPHILIA CAN BE FATAL (surgery in undiagnosed patients) Haemarthrosis is a vicious cycle and a hallmark of haemophilia Joint bleeding may be spontaneous (preceded by ‘tingling sensation’) and ceases when the joint pressure gets too high for bleeding to continue Following bleeding, the synovium ‘mops up’ blood and undergoes hypertrophy. Hypertrophied synovium is friable and prone to subsequent bleeding Recurrent bleeding leads to loss of cartilage and joint space Because joints become immobile – muscles begin to undergo disuse atrophy Muscle bleeds in haemophilia may result from exertion. The psoas muscle is commonly involved – bleeding in this muscle may result in compression of the femoral nerve and/or a compartment syndrome. 5. The treatment of haemophilia is switching to a prophylactic scheme The major advantage of a prophylactic scheme is decreased bleeding! ‘saves’ patients from haemophilic arthopathy No need for patients to carry around their own FFP Brings mortality rate upto normal Major disdavtages concern frequency of injections. Cost is also an issue o Half life of F8 = 8-12h = 3 injections a week o Half life of F9 = 18-24h = 2 injections a week Adjuvant treatments may be used in haemophilia treatment Tranexamic acid reduces clot lysis but may be teratogenic DDAVP stimulates circulating vWF-F8 concentration via its V2 receptor New developments in the management of haemophilia Anteneatal diagnosis allows prophylactic treatment from birth o Pre-implantation genetic diagnosis Designer molecules like recombinant F8 which have longer half lives & lower immunereactivity o A therapy linking F9 to the Fc portion of immunoglobulin has been shown to increase the half life to 60hrs o Pronlonging half life of vWF may prolong F8 half life indirectly? o Non-peptide cofactors may stimulate existing reservoirs Gene therapy – has a role in haemophilia B The main concerns about novel therapies are their thrombogenic potential and their cost 1.12 – THE CONTACT ACTIVATION SYSTEM 1. The contact activation system is the part of the intrinsic pathway which does not really contribute to coagulation The CAS occurs primarily on polyphosphate surfaces (platelet dense granules) Collagen is also touted as another -ve surface where this may occur The activation phase involves production of alpha12a o F12 binds with the help on zinc ions and a conformational change occurs o This leads to a cleavage at R353/V354 to produce alpha12a Alpha12a cleaves F11 & PK The fluid phase is driven by kallikrein (K) o K autostimulates 12a12a cleavage o K also cleaves 12a into smaller forms like beta12a. beta 12a is involved in PK/ C1 esterase activation but not F11 activation o K cleaves HMWK to release bradykinin o K cleaves c3/c5 into their active forms 2. The main products of the CAS are 12a, kallikrein, 11a and Bradykinin F12a may have pro-inflammatory function Promotes (Il1/6-) monocytes and neutrophils B12a cleaves C1 in the complement cascade 12a cleaves plasminogen slowly Is mostly regulated by C1 esterase (negative feedback control) Kallikrein/fletcher factor 75% is bound to HMWK Apart from what has been mentioned within the CAS, K also cleaves plasminogen Inhibited by c1 esterase HMWK is a source of bradykinin and may be anti-thrombotic HMWK binds to -ve surface with the help of Zn via their D5 domains. When doing so it displaces fibrinogen HMWK can cleave PK & F11 via its D6 domains When bradykinin is released, HMWK binds to surfaces more tightly and prevents other cells/molecules from doing so Apart from releasing bradykinin, HMWK inhibits neutrophil adhesion, enhances fibrinolysis Kininogens tend to have a number of antithrombotic domains and can achieve this function by: o Preventing thrombin binding to and activating platelets o Inhibiting calpain, which is a molecule released by thrombin o Inhibiting cleavage of PAR1 by thrombin HMWK is upregulated in pregnancy/ HRT 3. The CAS has a number of biological functions but it is unclear how far its role in coagulation is in humans a) Bradykinin formation a. Inmportant for vasodilation, platelet inhibition, inhibition of SMC proliferation, pain. (?excessive CAS shock) b. Promotion of tPA release from endothelial cells (fibrinolysis) b) Complement activation a. Pro-inflammatory b. C1 esterase deficiency = excessive complement activation = heridtary angioedema c) Thrombin inhibition by HMWK d) Fibrinolysis a. Cleavage of plasminogen by F12a and K e) Anti-adhesive a. HMWK inhibits protein/cell binding f) Angiogenesis a. HMWK & F12 bind to the uPA receptor on endothelial cells g) ?coagulation a. F12, HMWK & PK deficiencies both increase APTT but are not associated with bleeding b. F12 deficient mice taken longer to form clots but this is not seen in humans. (This could be because humans lack the PAR3 receptor which 12a otherwise activates) 1.13 F5 & F8 1. F5 & F8 have similar domain structures and similar physiological roles F5 physiology Synthesised only in hepatocytes Plasma F5 is taken up (not synthesised) by platelets, where they are stored in a partially active form that confers some APC resistance in platelet granules. Circulates as a single chain molecule Binds to and stimulates TFPI Acts as the cofactor for F10 within the prothrombinase complex F8 physiology Synthesised in hepatocytes and in some groups of endothelial cells It is stored with vWF in WPBs in endothelial cells and circulates as a heterodimer in a complex with vWF in plasma o vWF increases its t1/2, protects it from APC and prevents premature association with F10 o removal of vWF leads to change in conformation and circulation as an unstable heterotrimer circulating levels vary considerably because F8 is an acute phase protein acts as the cofactor for F9 within the intrinsic tenase complex F5/F8 have homologous domain structures The common template is A1-A2-B-A3-C1-C2 o This domain sequence is also homologous to ceruloplasmin and hephastin A domains are responsible for inter-protein interactions C domains are responsible for phospholipid binding B domains have very low sequence similarity between F5 & F8 and play different roles between the two F8 has additional acidic peptides which are responsible for its additional functions eg a3 binds vWF 2. The B domain is a key difference in the structure/function relationships between F5/F8 The F8 B domain is important for intracellular trafficking but NOT coagulation B domain allows F8 to bind to chaperone proteins within the ER Examples of such chaperone proteins are CNX/CRt and LMAN1/LMAN2; chaperone proteins facilitate folding, quality control etc for transport into the Golgi and, ultimately, secretion Removal of B domain does not alter F8 half life/ cofactor activity and hence has no role in pro-coagulant function Thrombin cleaves the B domain as well as the bond between A1/A2 to activate F8 The F5 B domain is important for coagulation F5 B domain also interacts with chaperone proteins for trafficking, but it is conserved in the circulating protein Some polymorphisms in F5 lead to truncation of the B domain - truncations that lead to the loss of a key regulatory sequence leads to a pro-thrombotic activity Like F8, thrombin activates F5 by cleaving the B domain Inactivation of F5/F8 is another key difference in their physiology Active F8 is an unstable molecule - the majority of F8 inactivation is spontaneous dissociation of the heterotrimer APC can inactivate remaining F8 by cleaving the A2 domain in 2 places (336,562) F5 is only inactivated by APC cleavage at 3 sites in the A1/A2 domains (306,506,679) o FV Leiden is the Arg506Gln mutation that prevents ‘fast cleavage’ 3. Combined F5/F8 deficiency occurs because the factors share trafficking pathways Both F5 & F8 have heavily glycosylated B domains which allow interactions with ER chaperone proteins Combined ‘deficiency’ is a rare AR disease associated with mutations in LMAN1/LMAN2 Blood levels vary but are never severely deficient - this is not a problem of transcription/translation; merely a problem in transport 4. F5 & f8 are both implicated in important disease processes concerning coagulation The major disease concerning F8 is haemophilia Low levels = Haemophilia A o Can be ‘mimicked’ by Type 3 vWD High levels are associated with increased risk thrombosis F5 & disease Low levels = ‘parahaemophilia’ (rare) High levels are not associated with increased risk of thrombosis FV leiden = APC resistance = pro-thrombotic SUMMARY Mr [] Domains B domain Production Circulation Distribution T1/2 Activation complex Inactivation High levels Low levels F8 Mr 3mill 0.4nM A1-A2-B-A3-C1-C2 + acidic peptides Not important for coagulation Liver & endothelium Heterodimer+vWF Plasma & VPBs 8-12h Thrombin cleavage of B domain heterotrimer Intrinsic Tenase Dissociation of heterotrimer + APC Thrombosis Haemorrhage F5 Mr 3.3mill 20nM A1-A2-B-A3-C1-C2 Important for coagultion Liver Single chain Plasma & Platelets 20h Thrombin cleavage heterodimer Prothrombinase APC cleavage No Thrombosis Haemorrhage 1.14 - ACTIVATED PROTEIN C 1. Protein C is the key anti-coagulant pathway in regulating the propagation of coagulation Summary of Protein C activity Produced in liver and circulates in plasma ~65nM Activated by T-TM complex on EC to inactivate F5a & F8a o Inactivation of 5a is by fast (but not inactivating) cleavage at 506 and slow (but completely inactivating) cleavage at 306 o Inactivation of F8a is via cleavage of Arg 336/562 APC is generates adjacent to the site of vessel injury; hence its physiological function relates to regulating coagulation, and in particular thrombin generation, to the site of injury. APC has a half life of about 30mins and is inactivated (slowly) by PC inhibitor, alpha1 antitrypsin and alpha2 macroglobulin 2. In usual circumstances, protein C binds to phospholipid membranes with poor affinity Domain Structure of Protein C Gla - EGF2 - SP o Gla domain requires Vitamin-K dependent gamma carboxylation (in 9 places) to bind to calcium ions and forming an omega loop o Gla domain facilitates binding to PL, EPCR & protein S o On its own, protein C binds PL poorly Gla - EGF2 - SP o EGF1 is beta-hydroxylated to bind to Calcium ions too o EGF2 is glycosylated (?function) 3. Thrombomodulin and EPCR are useful in bringing protein C into proximity with thrombin Thrombomodulin ‘alters’ the function of thrombin TM is a transmembrane protein (105kDa) expressed on all endothelial cells Thrombin binds to it with high affinity Binding to TM means that thrombin loses all its pro-coagulant functionality and acquires anti-coagulant (APC) and fibrinolytic (TAFI) properties EPCR binding brings protein C into closer proximity with TM EPCR is similar to MHC I and binds to protein C with high affinity o PC-EPCR affinity is considerably more than PC[Gla]-PL affinity EGF domains on TM are sufficient for protein C activation Domain structure: Transmembrane - Serine/threonine - 6EGF- lectin o Serine-threonine binds the GAG chondroitin sulphate which allows thrombin to bind with TM much more efficiently (providing a surface; reducing Km) Transmembrane - Serine/threonine - 6EGF- lectin o EGF 4 binds to the SP of protein C (low affinity) o EGF 5/6 bind to exosite ?1 on thrombin, which aligns its active site in such a way that protein C can be cleaved o Thrombin cleaves Arg 169 to release activation peptide and create APC Transmembrane - Serine/threonine - 6EGF- lectin o Lectin domain has no haemostatic role 4. Protein C is probably entirely dependent on its cofactor, protein S, to function properly Physiologically - PC is probably useless without PS; there is no change in rate of coagulation regardless of PC concentration, in plasma that is deficient of PS Structure of Protein S 69Kda protein synthesised in the liver Domain structure: Gla - thrombin sensitive - 4EGF - SHBG o 11 Gla residues (2 more than protein C) gives protein S the highest affinity for PL of all vitamin-K-dependent proteins o Gla residue also contributes somewhat to protein C binding Gla - thrombin sensitive - 4EGF - SHBG o Thrombin sensitive region is essential for co-factor binding & function Gla - thrombin sensitive - 4EGF - SHBG o EGF1 contributes to protein C binding o All EGFs are heavily beta-hydroxylated Gla - thrombin sensitive - 4EGF - SHBG o SHBG binds to complement4b binding protein c4b-bp; bound protein S cannot act as a cofactor for protein C (approx. 60% is bound) Hence the domains important for protein C binding are Gla, thrombin sensitive & EGF1 The major function of Protein S may be to increase protein C’s affinity for Pl binding Protein S increases affinity for PC/APC to bind PL and hence interact with thrombin/cleave 5a and 8a respectively Inactivation of 5a: o Protein S relocates APC active site - particularly important because this means the usually slow 306 cleavage for F5a becomes fast o Protein S may enhance inactivation of the prothrombinase complex, which otherwise confers F5a ‘resistance’ to APC by keeping the factor bound. Inactivation of 8a: o Protein S enhances APC inactivation of F8a (3fold) by enhancing the 562 cleavage and making the inactivation of F8a less dependent on its spontaneous disscoiation 5. Deficiencies in the Protein C pathway are associated with thrombophilia Protein deficiency PC PS EPCR TM F5 leiden Allele frequency Clinical result 3/1k 1/20k ? V rare ~10% European caucasians Purpura fulminans in homozygotes, VTE in heteros Purpura fulminans in homozygotes, VTE in heteros Unknown; lethal in mice PEs; MIs Only increases thrombotic risk slightly because usually only one allele is affected meaning that protein C mediated inactivation is only slowed, not terminated. Does increase thrombotic risk in context of other genetic/environmental risk factors 1.15 - ADAMTS13 1. The multimeric structure of vWF usually protects it from the MMP ADAMTS13 Structure of vWF relevant to ADAMTS13 Ck domains create dimers in ER D3 domains are key in multimerisation - larger vWF molecules have more binding sites so they adhere to collagen better and ‘catch’ platelets more effectively - more pro-coagulant activity o Larger multimers are more unstable so become linear with less difficulty A3 domain (collagen binding) is exposed in globular structure. A1/C1 (platelet binding) and A2 (ADAMTS13 binding) only become exposed in linear structure o Hence in its globular circulating form, vWF is usually protected from ADAMTS13 2. The domain structure of ADAMTS13 confers step-wise interactions with vWF, ultimately leading to proteolysis Summary of ADAMTS13 structure 190kDA zinc-dependent MMP which circulates as an active enzyme Very long half life (days) Only has one substrate and one cleavage site- the Tyr1605-Met1606 bond on the A2 domain of linear vWF Has no natural inhibitor Domain structure of ADAMTS13 CUB domains may be implicated in binding globular vWF TSP1 repeats 5-8 may also be implicated in binding globular vWF o Hence the idea is that globular vWF can carry ADAMTS13 via its c-terminal domains in the circulation without proteolysis occurring Spacer domain is essential to ADAMTS13 function o Has no disulphide bonds (only part of the molecule; hence ‘spacer’) o Arg 660, tyr 661 & tyr 665 bind to linear A2 vWF with high affinity o Hence the spacer domain is the first domain that plays a role in recognizing unfolded vWF Cysteine rich domain has an unknown function but is important for normal ADAMTS13 activity Dis(integrin) domain is the next domain that recognizes linear vWF o R349 and L350 bind linear A2 vWF (at D1614) MMP o 3 histidine residues (in a highly conserved HEXXHXXGXXH sequence amongst all MMPs) bind Zn to the active site o Zn binding leads to a shape change that ‘exposes’ or ‘activates’ the key catalytic glutamic acid residue (much like how serine is the key residue in SPs) o The activated conformation contains a ‘cleft’ for vWF to lie in; glutamic acid hydrolyses the scissile Tyr1605-Met1606 bond o Calcium ions are required for normal MMP function - but don’t know why The stepwise interactions with vWF of ADAMTS13 a) Low affinity C-terminal bonding keep ADAMTS13 in proximity with globular vWF b) c) d) e) collagen binding and/or shear stress unfolds globular vWF and exposes A2 domain Spacer domain binds linear A2 domain of vWF with high affinity Dis domain further binds A2 domain MMP binds and cleaves A2 domain at scissile bond tyr1605-met1606 3. ADAMTS13 may have its major role as soon as vWF is released form the endothelium In WPBs , vWF is in globular form and elongates under shear stress as soon as it is released ADMATS13 may act here to prevent circulation of ultra large vWF multimers In other times when unstable globular vWF spontaneously unravels under shear stress, ADAMTS13 may also act ADAMTS13 probably acts during platelet plug development to limit its size and prevent production of an occlusive thrombus. The ADAMTS13-vWF specificity is achieved in 3 ways vWF MUST unravel before it can be cleaved there are multiple sites of interaction in order to get ADAMTS13 & vWF to fit together properly vWF must fit into the active site cleft or it will not by hydrolysed by glutamic acid 4. Aberrant vWF proteolysis correlates to diseases of coagulation Excessive vWF proteolysis is implicated in Type2a (group II) vWD A2 domain mutations = easy unfolding = increased cleavage by ADAMTS13 The phenotype relates to easy haemorrhage Impaired vWF proteolysis results in TTP; thrombotic thrombocytopenic prupura Rare disease characterised by microthrombi which are rich in platelet and UL-vWF (little fibrin) o High circulating unstable Ul-vWF more spontaneous unravelling inappropriate primary haemostasis (thrombotic) o Platelets are used up (thrombocytopenic) o MAHA occurs because red cells get damaged against micro0thrombi/ occluded vasculature Disease process is seen when ADAMTS13 activity drops to <5-10% of normal Congenital TTP: o Most mutations impair secretion o Heterozygotes tend to be asymptomatic Acquired TTP o Usually due to IgG antibodies produced against the spacer domain, in particular the sequence which allows vWF A2 binding Untreated = mortality >90%. Principle of treatment lies with plasma exchange every 2-3 weeks to give a source of ADAMTS13 and remove the auto-antibodies in acquired disease 1.16 - PATHOPHYSIOLOGY OF vWD 1. Diagnosing vWD requires a number of laboratory tests assessing vWF quantity & function There are a number of problems when it comes to assessing vWF - it is difficult to say what is normal It has multiple binding interactions and hence multiple functions; one or many of which may be lost It has a multimeric structure There are different pools of human vWF (plasma, WPB, subendothelium, platelets) The ABO blood group plays an influence on circulating vWF concentration. In addition vWF levels increase with age Stress induces vWF release from stored WPB In vivo function is shear dependent, and this is difficult to replicate in a lab Antigenic assays only measure vWF quantity Methods include Laurell rocket (not in use), ELISA & Immunoturbidometric (more commonly used) analyses Although accurate, sensitive and reliable - gives no reflection of functional activity and hence is not applicable to Type2 vWD Rco and RIPA are two tests that assess vWF-platelet binding Both tests use the antibiotic Ristocetin, which mimicks shear stress and thus causes globular vWF to unfold and interact with platelets The vWF-platelet agglutinate causes turbidity The Rco test uses an excess Ristocetin in the presence of a low concentration of vWF [dilute plasma] to test whether vWF can bind to platelets at all o It is labour intensive, has poor reproducibility but is generally reliable o Failure of a response suggests lack of large vWF multimers or an aberrant GP1b The RIPA test uses minimal Ristocetin. In normal patients this concentration (0.7) is not enough to stimulate vWF, so this test is used to assess whether vWF is hyper-active o Hence RIPA is diagnostic for T2B vWD The other three main tests of vWF function relate to collagen & F8 binding, and ability to form multimers Collagen assays use a labelled anti-vWF Ab to pick up vWF binding on a collagen medium o Poor binding suggests lack of large multimer or an aberrant A1 domain (collagen 6) Multimer analyses compare multiemr profiles to a standard o Abnormal profile can be suggestive of a number of disease processes Only small multimers = early clearance/cleavage of vWF-Plt complex Only large multimers = failure of ADAMTS13 Loss of multimer ‘flankers’ = failure of ADAMTS13 F8 assays use a labelled rF8. vWF is in excess so there are ample F8 binding sites o Poor binding is diagnostic of T2N vWD 2. The classification of vWD relates to structure and function vWD 1 (AD) 2A (AD) 2B (AD) 2C Physiology Partial quantitative deficit Absence of large multimers defective platelet binding Hyper active vWF strong platelet binding Loss of collagen binding ability Diagnosis Difficult - bleeding score Rco with abnormal multimer analysis RIPA Collagen binding assay 2M (AD) 2N (AR) 3 (AR) Aberrant GP1b defective platelet binding Defective F8 binding Complete quantitative deficit Rco with normal multimer analysis F8 assay Antigenic assay T1 & T2 vWD are differentiated by their function:antigen ratio T1 vWD will demonstrate a concordant loss of function as antigen levels drop T2 vWD can be suspected if the loss of function is <0.7 than the loss of antigen o Function:antigen <0.7 3. The normal variation in circulating vWF makes it difficult to conclusively say whether a patient just has low normal levels or T1 vWD, and has led to production of the ‘bleeding score’ Because vWF levels vary so much amongst the population (blood group, ethnicity) and in individuals too (age, stress), it is difficult to distinguish people who have a low vWF level which is normal for them, from those who have a true partial deficiency – T1 vWD. Of people who actually have T1 vWD, only 50% have demonstratable mutations. in most cases, the defect is caused by interactions between mutant and normal subunits [dominant negative effect] The questions asked in a history might be key in highlighting T1 vWD Epistaxis lasting > 10min Large bruising, in more than one site Haematomas A Bleeding score >4 may be the most appropriate diagnostic tool in T1 vWD The bleeding score repeats the following grading for bleeding from oral cavity, minor wounds, GI, epistaxis, menorrhagia etc Blood source Dental extraction -1 none 0 Bleeding occurs <25% of the time, doesn’t require intervention 1 Bleeding occurs >25% of the time, requires intervention 2 Bleeding requires suturing/ packing 3 Bleeding requires transfusion and/or DDAVP 4. The other types of vWD are not as common as T1 vWD Type 2A = quantitative inability to bind platelets [because of loss of large multimers] Group 1 patients lose large multimers because of mutations that prevent normal secretion of vWF and hence retention of vWF in the ER o Mutations occur anywhere in the vWF gene, and large multimers are more likely to contain the mitation Group 2 patients lose large multimers because of enhanced ADAMTS13 activity o Mutations only occur in the A2 domain Some other mutations implicated are defects in di-/multimerisation & susceptibility to intracellular proteolysis Type 2B = hyperactive vWF Increased affinity for platelets = early clearance of vWF-Plt complex = loss of large multimers and thrombocytopenia o Mutations are in A1 domain Type 2M = qualitative inability to bind platelets [because of defective GP1b] All the normal multimers are there Mutations [in GP1b] are commonly found in A1 domain Type 2N = inability to bind F8 All the normal multimers are there, in the adequate quantity and can bind to platelets normally, but loss of F8 binding dramatically reduces half life of F8 Gives haemophilia-type bleeding pattern Mutations seen in D’/D3 domains Type 3 = complete loss of vWF Loss of vWF = impaired primary haemostasis and concomitant reduction in F8 half life gives a coagulation deficit too A number of mutations are implicated Heterozygotes do not suffer significant bleeding 5. Management of vWD depends on the sub-type because of different responses to treatment Options for therapy: Nothing Tranexamic acid DDAVP Replacement o Cryoprecipitate and platelets are commonly used o rF8 is being developed (human concentrates used to be used but transmitted HIV/HBV/HCV) DDAVP stimulates WPB vWF release – who responds? T1 – most patients respond o A T1 subtype named T1 ‘Vicenza’ make normal concs of vWF but cleave it rapidly, and so they display an unsustained response to DDAVP T2 – response is limited because most patients fall into a rapid clearance/ defective vWF group anyway o 2N patients will not respond because F8 just can’t bind to vWF T3 – no response 1.17 – STROKE 1. Epidemiology of stroke 3rd commonest cause of death and commonest cause of severe adult disability £3billion pounds per annum in direct costs alone in UK (versus 2bill for CHD) o 4.5bill on indirect costs? 80% of strokes are ischaemic; 20% are haemorrhagic hypertension is a strong risk factor 2. Pathogenesis of stroke Stroke is a focal neurological deficit or presumed vascular origin lasting >24hrs; the diminished blood supply leads to loss of o2, accumulation of co2, and loss of ionic gradients across membranes synaptic transmission is lost after 3 mins, no electrical excitability occurs after 5 mins the core of the lesion will not recover; the surrounding ‘penumbra’ region has the potential to mechanisms of iscahemic stroke: o carotid artery stenosis (atherosclerosis) o emboli of a cardiac origin (AF) o small vessel thrombosis/occlusion o watershed infarct in presence of systemic hypertension? mechanisms of haemorrhagic stroke: o primary/small vessel intracerebral bleed o Rupture of [berry] aneurysm subarachnoid haemorrhage 3. Risk factors for stroke AF & hypertension are strong risk factors poor diet etc – CVS/ CAD risk factors Polymorphisms that lead to a thrombophilic state (eg F5 leiden, Prothrombin G20210A) 4. Acute management of stroke as time passes, the size of the core increases and the penumbra decreases (potential to recover diminishes over time) tPA benefit is seen particularly within the first 3 hours 1.18 - PLATELETS & ANTIPLATELET THERAPY 1. Platelets have extracellular receptors and intracellular granules which are key to their function Extracellular glycoproteins are adhesive - they make the platelet ‘sticky’ GP2b3a (integrin like) binds to fibrinogen and vWF o It also binds to a number of other proteins with the key ‘RGD’ AA sequence o In its rested state it can not take part in binding; calcium influx causes it to unfold GP1b exists as a complex with 2alpha, 2beta, 2 GP9 and 1 GP5 complex (2:2:2:1). Its main ligands are vWF, thrombin and F11(a?) GP1a and GP6 complex are both involved in adhesion to collagen (GP1a- collagen 6) G protein linked receptors play a role in positive feedback after platelet degranulation ADP binds to P2Y receptors Thrombin cleaves the PAR (protease-activated-recptor) receptor 1 & 4 Thromboxane binds to its own receptor and there is also a receptor for prostacyclin Prostacyclin (and NO) produced and released by endothelial cells keeps platelets quiescent until they meet an appropriate ligand There are 2 main types of platelet granules, as well as lysosomes Dense granules contain molecules involved in positive feeDback - mainly ADP & catecholamines but also ATP, calcium ions and serotonin Alpha granules contain coagulAtion molecules - platelet factor 4, vWF, fibrinogen, F5 Lysosomes contain a number of enzymes, most of which are proteases 2. Platelet activation involving intracellular signalling pathways that result in a calcium influx Step 1 involves induction of positive feedback mechanisms a. GP1a binds to exposed collagen at low shear stress or GP1b binds exposed (subendothelial) vWF at high shear stress [probably a degree of both] b. Both activate the second messenger PLC gamma c. PLC gamma induces the IP3/DAG signalling pathway which leads to a calcium influx d. The calcium influx causes degranulation, which importantly releases ADP vWF and fibrinogen, and stimulates thromboxane A2 synthesis i. At the same time GP2b3a begins to unfold ii. Also at the same time, microtubules begin to change the structure of the platelet into a ‘spreading’ cell. The change is ultimately irreversible Step 2 causes aggregation of platelets e. ADP, thrombin and Thromboxane A2 bind to their respective receptors i. These mediators bind to platetlets they were released from and/or other local platelets f. The secondary molecule in this case is PLC beta - which also causes a calcium influx g. At this point (i.e. after thrombin and collagen binding) there is enough calcium to cause ‘inversion’ of the phospholipid membrane - which speeds up the coagulation cascade i. This is achieved by calcium inhibition of flippase (which keeps PPDserine & ethanolamine on the inner membrane) and stimulation of scramblase h. The main players in platelet aggregation are Thromboxane A2 & Gp2b3a 3. There are a number of ways that platelet number and function can be assessed in the lab a. Number - assessed using impedance studies, the same as for RBCs - technique varies from lab to lab so normal ranges (150-400e9) may differ b. PFA-100 – aspiration of blood through collagen lined aperture and measuring time for plug formation and occlusion of the aperture – upto 190s is normal c. Aggregation tests - shines light through platelet rich plasma and measure change in transmisiion following addition of an agonist eg ADP, adrenaline or collagen i. ADP & adrenaline are weak agonists for platlets so tend to show a 2 wave increase in transmission ii. A lack of secondary wave suggests receptors are ok but there is some fault downstream of this (strage pool disease) or use of aspirin iii. Lack of aggregation in all agonists except for ristocetin suggests a GP2b3a problem – Glanzmanns iv. requires large volume of blood, is poorly reproducible and is sensitive to platelet interaction with food etc d. Storage pool & release function - 3 methods: i. Measuring release reaction (Lumi - similar to aggregation tests) ii. EM iii. Measuring ATP:ADP ratio (usually <2) - this is increased in storage pool diseases because of a lack of ADP iv. very labour intensive e. Flow cytometry – sensitive, specific and only requires a few milliliters of blood. diagnostic for receptor defects f. Genetic analyses 4. Antiplatelet agents play a key role in the prevention of arterial thrombosis Aspirin irreversibly inhibits COX1 (and COX2) the mechanism of action is acetylation of serine near the active site platelets, being anucleate can not synthesise anymore COX1 low dose (75mg) aspirin is good for anti-platelet effects o half life = 15-20mins and as it is almost completely metabolised first pass, it inhibits platelets that pass in the portal circulation o mean life span of platelets ~10days so knocking them all out keeps you ‘safe’ for about this time until new ones are synthesised very high doses of aspirin would be needed for anti-inflammatory affects via inhibition of COX2 – because COX2 is induced by shear stress on endothelial cells. this is not ideal because of side effects associated with high dose aspirin (bleeding, GI ulcers) o COX2 makes prostacyclin (high shear COX2 PGI2 vasodilation less shear) Aspirin ‘resistance’ terms compliant patients who still form thrombi when on aspirin. this is mainly due to failure to suppress TXA2 production due to alternative production mechanisms in the individual: o production of TXA2 by monocytes o an unusually high/fast platelet turnover o high vWF? ADP receptor blockade Clopidogrel is a prodrug which is activated by 2 step cytochrome P450 metabolism. o it irreversibly binds to P2Y12 receptors (disulphide bond) o it causes 50-60% inhibition of ADP-induced aggregation & this lasts for several days o commonly used with aspirin post ACS (CURE study) o polymorphsims in the liver enzymes/ P2Y receptor genes can give variable responses Prasugrel is similar to clopidogrel but is more rapid (1 step) and consistent (perhaps more bleeding risk) Ticagrelor is a reversible inhibitor of P2Y12 – onset takes 2 hours and its half life is 12hours dipyridamole dimishes intracellular adenosine by preventing reuptake and inhibiting adenosine deaminase. it also inhibits phosphodiesterase which causes high intraceullar cAMP – this impairs platelet aggregation GP2b3a receptor blockade Abciximab can completely abolish aggregation if 80% of GP2b3a receptors are blocked Tirofiban is a tyrosine derivative eptifibatide is another alterntative GP2b3a blockers have been licensed for ACS/PCI but they all cuase increased bleeding Novel targets incluce P-selectin, thromboxane recptor blockade Some protocols: Aspirin + Clop; 1year post ACS with metal stent Aspirin + dipyridamole – secondary prevention of stroke Warfarin + aspirin – PCI + AF 1.19 – HERIDITARY PLATELET DISORDERS 1. Clinical picture of platelet disorders *Muco-cutaneous bleeding* in the history is suggestive of platelet disorder spontaneous skin petechiae/ purpura bleeding from mucous membranes, epistaxes prolonged bleeding after trauma/surgery bad menorrhagia at menarche for girls family history Bleeding is unusual if platelet count is >30e9; if there is a discrepanacy between bleeding history and platlet count, this may suggest a functional platelet defect. 2. classification of heridtary platelet disorders – production and function Inherited Disorders of platelet production are rare These are almost always part of a wider problem or a pre-leukaemic disease. some examples are: Congenital aplastic anaemia syndromes amegakaryocytic thrombocytopenia o mutations in TPO receptor = no megakaryocytes in BM; platelet count <20 o develops into aplasia/leukaemia, requires BM transplant thrombocytopenia with absent radii syndrome o AR disease with absent radii & phalanges although the thumb is always normal o the platelet count is <50 but normalises with age o TPO signalling pathway is probably defective; megakaryocytes (defective CFU-meg) are absent from BM MYH9 related disease o spectrum of disease associated with non-muscle myosin mutations o macrothrombocytopenia, (count <20), WBC inclusions, renal failure, hearing loss and cataracts are some clinical features o genetic analysis key to diagnosis; Dohle bodies on microscopy are pathognomonic a number of other eponymous syndromes (digeorge, , paris-trousseau) Functional disorders (covered below) can be defects in GPs, storage pool or release 3. Plasma membrane defects Bernard Soullier syndrome is due to decreased/ defective GP1b GP1b complex contains 2 disulphide linked subunits, covalently bonded to GP9 as a heterodimer. there are roughly 25k complexes per platelet this is an AR disease which has a variable but often severe bleeding pattetn mild thrombocytopenia with increased mean platelet volume and bleeding time are seen absent/reduced agglutination with ristocetin and flow cytometry may also diagnose it Pseudo-vWD is the opposite half of T2b vWD Hyper active GP1b (not hyper active vWF) is the problem in this case as with t2b vWD, low conc ristocetin (Rco) test will diagnose it, but you must treat it with platelets, not vWF Glanzmanns thrombasthenia is due to decreased/ defective GP2b3a GP2b3a complex is also a heterodimer; there are roughly 80k complexes per platelet this is also an AR disease associated with severe bleeding. there are 3 subtypes: o type 1 = Absent GP2b3a or no fibrinogen in alpha granules o type 2 = partial deficiency in GP2b3a or fibrinogen in alpha granules o Variant Glanzmanns is due to a functionally defective GP2b3a Flow cytometry and genetics are key to diagnosis Platelets to treat. formation of antibodies to normal platelet GP2b3a is associated with a worse prognosis (because you cant give them any more treatment!) Scott Syndrome is due to defective phospholipid inversion pathogenesis is a failure of platelets to generate microparticles on activation; hence PPDserine is not expressed normally and clotting factors can not bind bleeding is moderate to severe; this disease is very rare though collagen receptor defects often only causes mild bleeding because platelets have a number of membrane proteins which can bind collagen 3. intracellular disorders are subclassified by what storage granule is problematic intracellular disorders are more common but only give mild bleeding. platelet count and lifespan are usually normal and ATP:ADP ratio is an important diagnostic tool. storage pool disease - Dense granule deficiency Idiopathic (non-albino type) hermansky-pudlak syndrome o AR disease associated with mild bleeding o due to membrane and content abnormalities for dense granules o oculocutaneous albinism and very bad nystagmus are features – treat with tranexamic acid chediak higashi syndrome o AR disease associated with increased risk of infections; treat with bone marrow translpant wiskott-aldrich syndrome o due to defective WASP protein expression o associated with eczema, immune deficiency and requires splenectomy or BMT storage pool disease = alpha granule deficiency Grey platelet syndrome o AD rare disease where alpha granules are absent/empty (so platelets appear grey on blood film) quebec platelet disorder o AD disease associated with alpha granule multimerin deficiency; reduced contents combined storage pool disease defects of thromboxane generation are due to COX/ thromboxane synthetase deficiencies defects in signal transduction can be suspected if you defective aggregation responses to all agonists 4. treatment of hereditary platelet disorders requires specialist care Supportive measures (avoid aspirin, NSAIDs, give tranexamic acid) DDAVP (but not in kids as it gives hyponatraemia) platelet transfusion – HLA match if they will need lifelong transfusion to avoid Ab synthesis rF8 for Haemophil/glanzmanns patients who have developed Abs BMT – usually just for Bernard soullier and glanzmanns; 10% mortality at least 1.20 – PREGNANCY OESTROGENS AND THE COAGULATION SYSTEM 1. Oestrogens are associated with an increased risk of VTE Thrombotic changes associated with oestrogens Increased procoagulant activity o stimulation of Fibrinogen, F7-11, vWF, protein C resistance Decreased anticoagulant activity o Inhibition of protein S and antithrombin o the pill reduces transcriptional synthesis of protein S But there is some increased anticoagulant activity too o Heparin cofactor 2, protein C & alpha2 antitrypsin are stimulated Fibrinolytic changes associated with oestrogens [net reduction in fibrinolysis] Increased antifibrinolytic activity o stimulation of F13 decreased profibrinolytic activity – inhibition of tPA there is also some stimulation of fibrinolysis (via plasminogen, F12 and prekaallikrein) as well as inhibition of anti-fibrinolysis by PAI-I, there is a net anti-fibrinolytic activity though The oestrogen dose of the pill has decreased amidst evidence of VTE risk The drop from 100microg to 50 of ethinyl oestradiol gave the biggest drop in risk all contraceptive pills seem to increase risk of VTW between 4-6times o 3x risk if <30years old; higher risks with increasing age o the highest risks are seen when first starting the pill, and post partum different ‘generations’ of progesterone component of the COC were designed to reduce this risk, the 3rd generation (eg desorgestrel) however gave more risk than the second generation (eg levonorgestrel) o But note - the progesterone only pill and mirena do not increase VTE risk COCP also seems to increase risk of arterial thrombosis by 2-3x; this is a cloudy area though hence you need to balance risks with benefits (avoids unplanned pregnancies, regulates dodgy periods, controls PMS/migraine, decreases ovarian/enodemetrial cancer) 2. The pill interacts strongly and synergistically with other thrombophilias the degree on interaction is unpredictable risk increases upto 30times in F5 leiden, but only about 16x in PT G20210A o although the risk of cerebral vein thrombosis is particularly high in Prothrombin mutation patients who take the pill o also interacts with High F7 [and other factors], antithrombin/PC/PC deficiencies screening is an option but between 400k and 2mill women would have to be screened to prevent one death – not viable; better to offer patients counselling and leave treatment decision on a good history and assessing risks/ benefits – some thrombophilias can be asymptomatic 3. HRT is used in an older patient cohort – this translates to a higher relative risk of VTE than OCP HRT is now used in small doses to alleviate symptoms of menopause. it still has beneficial effects in preventing osteoporosis but does not seem to be protective for CVD risk is greatest in first year of use; otherwise relative risk seems to be about 2x transdermal HRT patches have not been shown to increase VTE risk HRT in asymptomatic thrombophilic women should be discouraged 4. Pregnancy puts women in a procoagulatory state to prevent excessive blood loss when uteroplacental separation occurs at birth Major coagulatory changes in pregnancy pre – hypercoagulable & hypofibrinolytic increased thrombin generation o vWF (and F8) increase 2-3x progressively throughout term o fibrinogen increases 2x o F7 increases 1.5x o protein S falls by half ?increased fibrin cleavage reduced fibrinolysis o PAI1 increases 5 fold o PAI2 is produced by the placenta interactions with other maternal factors 85% of pregnancy VTEs occur on the left due to anatomy of common iliac arteries Risk factors of VTE in pregnancy 1/1k pregnant women suffer VTE; the risk is highest in the first two trimesters and the post partym period women with high BMI are at an increased risk dehydration, pre-eclampsia, emergency caesareans, old age and multiple parity are all associated with increased risk Management of VTE in pregnancy improve assessment of which women are at a higher risk recognise symptoms like leg pain as early warning signs and diagnose quickly o TEDs should be worn for 2 years if a diagnosis is made; and thromboprophylaxis given for subsequent pregnancies If women are at increased risk then give thromboprophylaxis (LMWH + TEDs) and encourage mobilisation and hydration o aim for 6 months treatment in total o warfarin is teratogenic in first trimester (small molecule; crosses placenta) 5. management of obstetric haemorrhage Preconception counselling for women who have a bleeding tendency/increased risk antenatal counselling fetal sexing/ USS diagnosis/ fetail DNA sampling/ CVS/ amniocentesis upto 17weeks gestation to diagnose if the unborn child has the hereditary problem o 1% risk of miscarriage with these procedures avoiding instrumental deliveries etc if child is found, for example, to be haemophilic 1.21 - AUTO-IMMUNE DISEASE IN HAEMATOLOGY 1. Autoimmune diseases are generally acquired in haemoatology; some targets are: Target platelet F8c vWF F13c F9/10/11c GP2b3a ADAMTS13 Heparin-PF4 Prothrombin beta2GP1 Disease ITP acq Haemophilia A acq vWD acq F13 def acq factor def acq Glanzmanns TTP HITT APS APS Phenotype BLEEDING THROMBOSIS 2. Idiopathic TTP is a serious disease thought to be related to ADAMTS13 deficiency TTP is a fairly rare disorder with a high mortality incidence ~4mill/year, affecting young females commonly mortaility >90% if untreated idiopathic TTP presents without a predisposing condition or oliguric renal failure o familial disease is associated with ADAMTS13 deficiency o isolated disease is thought to be autoimmune destruction of ADAMTS13 secondary TTP is a thrombotic microangiopathy with a predisposing condition; eg: o cancer, sepsis/ HIV infection, pregnancy, pill, eclampsia o drugs eg Ticlopidine, clopidogrel, quinine, ciclosporin, mitomycin C, pentostatin HUS is a thrombotic microangiopathy with acute loiguric renal failure and sparing of the other organs – shiga toxin from E-coli seems to be causative TTP presents as a classic pentad of signs MAHA*[shistoc ytes on blood film]+ Low Plt* are key Neurological dysfunction renal failure fever Investigations may show low Hb, high creatinine, high LDH PT/APTT are normal Plasma exchange is the management of choice in initial TTP plasma exchange still has 20% mortality associated with it (within 5 weeks) o plasma esxchange 30-60ml/kg daily +methylprednisolone for 3days until there is a complete response – normalisation of platelets and LDH with stable neurological signs o continue exchange after response every other day for four days o complications of exchange include blockage of catheter or reaction against plasma/ introduction of infection o avoid platelets and anti-platelet drugs 80% respond in roughly ~16days; 40% of these have exacerbations within a week and 30% definitely relapse within 2 years o [20% dead within 5 weeks] o relapsing disease may warrant immunosuppression – rituximab/vincristine/splectomy 3. Heparin induced thrombocytopenia is a rare disease that must be diagnosed clinically non immune HIT causes mild transient thrombocytopenia(>100e9) which doesn’t require treatment; it is however a diagnosis of exclusion clinically significant HIT only occurs in 3% of people: o platelet count drops on heparin admission to <30-50% of previous or <100e9 within 5days o thrombo-embolic complications begin to occur eg VTE/ heparin induced skin lesions/ venous gangrene o prior history and use of UFH before major surgery are associated with higher risk o rapid onset/delayed onset HIT occur either side of the 5day ‘cut-off’ the differential diagnosis for HIT includes ITP, DIC. if the disease process starts <5days suspect DKA/SBE/PNH HIT score can aid diagnosis: higher the score, more likely it is that you have HIT Finding 2 1 0 thrombocytopenia fall of ~50% fall of ~30-50% fall of <30% timing day 5-10 after day 10 before day 5 thrombosis new clot, skin necrosis progress/recurrence none oTher cause none seen possible definite The pathogenesis of HIT involves widespread platelet activation PF4 normally binds to activated platelets and forms complexes with heparin autoantibodies (IgG) bind to the PF4/heparin complex platelets get activated via their fc receptors to release procoagulant microparticles Management = stop heparin, initiate alternative anticoagulant and test for antibodies o can also add direct thrombin inhibitors eg Lepirudin 4. Haemophilia A and vWD like syndromes can be acquired due to autoimmune disease Acquired Haemophilia A occurs because of antibodies against F8 presents in middle-aged/elderly patients with extensive cutaneous purpura/ internal bleeding antibody titre seems higher in pregnancy polyclonal IgG4 Abs formed against A2/C2 domains of F8 o antibodies are time-dependent (type 2 kinetics?) treat with immunosuppression eg prednisolone +/- cyclophosphamide. o some studies say 71% of people respond; with about 20% relapsing roughly 8months after stopping immunosuppresion Acquired vWD occurs in the context of a background disease process Immune mediated disease is associated with background Lymphoproliferative or autoimmune disease. DDAVP/IVIg/F8 concentrate may lead to response Proteolysis-mediated disease is associated with background thrombocytosis or conditions leading to high shear eg aortic stenosis – you must treat the underlying cause 1.22 – NOVEL METHODS OF ASSESSING HAEMOSTATIC FUNCTION 1. The traditional ‘reductive’ methods of assessing haemostatic function are limited because about 50% of patients with thrombosis do not have a specific deficit The pros of the reductive approach are specificity of diagnosis and treatment that is directly targeted to a deficiency traditional methods are less attractive for complex diseases – leading to increased popularity of global assessments of haemostasis global assessments take into account that coagulation is an integrated system 2. Some global assessments of haemostasis are not specific = high false positive rate Antibodies to measure enzyme-activation markers are not in general use Activation peptides [these are released on zymogen activation] and enzyme inhibitor complexes [the intermediate] can both be measured o it is a difficult process, has limited sensitivity in thrombophilia and is largely ineffective in predicting thrombosis – not in general use D-dimer is useful, but not specific, in ruling out thrombosis d-dimers are only released by plasmin when fibrin has been crosslinked by F13 They offer an indirect measure of thrombin generation (and F13 activity) Low/normal d-dimer = low chance of thrombosis (clinical application is ruling out [not diagnosing] VTE) o used to diagnose DIC, but, as with VTE, only by ruling it out (poor specificity) 3. Measures of coagulation potential thromboelastogram/ROTEM o involves measuring changes in clot strength on a blood sample exposed to celite o does not give a specific diagnosis but gives idea of coagulation and fibrinolyutic ‘strength’ endogenous thrombin potential o Uses TF to give real time thrombin generation using a fluorescent substrate on platelet rich/poor plasma o poorly standardised so it is primarily a research tool at the moment o may have future roles in assessing responses to therapies 4. Measures of primary haemostasis only PFA/bleeding time 1.23 – MALIGNANCY ASSOCIATED THROMBOGENESIS 1. Cancer is a big risk factor for development (and recurrence) of VTE annual incidence is roughly 1:200 o although it could be higher than this because asymptomatic VTE is common and unaccounted for, and clinical manifestations are non-specific due to background disease There is a 4-7x increased risk of VTE in cancer patients VTE is the second biggest killer in cancer patients; 1 in 7 cancer px die of a PE o the longer the time between cancer and VTE diagnosis (presumably because of undetected, asymptomatic disease) –t he greater the risk of dying Other VTE risk factors are age, stasis/surgery, family history of VTE, varicose veins, CHF/MI/Stroke, lower leg fractures, OCP/HRT/pregnancy Idiopathic VTE may be a predictor of occult malignancy Tumour type/site influences risk of VTE: RR baseline risk intermediate risk >17x highest risk >25x site lung, colon, breast, ovary, prostate leukaemia, liver, cervical/uterus pancreas, lymphoma, brain Anti-tumour therapy may play a role in increasing VTE risk too o chemo (eg Thalidomide and Lenolidomide in Multiple Myeloma) o hormones o surgery/immobility 2. The pathogenesis of VTE in cancer is complex and probably poorly understood It is possible that malignant cells induce monocytes/macrophages to produce TF Worth noting that cancer patients can often have other co-exisiting thrombophilias eg F5 leiden some tumours eg adenocarcinoma produce pro-thrombotic mucin 3. The management/secondary prophylaxis of VTE in cancer may switch to long term use of LMWH Usual management of VTE in cancer involved 5-7days LMWH until INR reaches 2 and then warfarin for 3-6months as secondary prophylaxis The CLOT study 2003 suggested long term LMWH is associated with decreased risk of VTE recurrence with no change in bleeding or mortality 1.24 – ACQUIRED HAEMOSTATIC DEFECTS (DIC/CPB/HUS) 1. DIC is an excessive and inappropriate activation of coagulation which is always secondary to an underlying disorder The pathogenesis of DIC probably involves a confluence of pro-coagulant mechanisms TF/ other procoagulant material is directly released into circulation o this can be secondary to trauma/malignancy TF expression can be increased o Either due to endothelial damage (sepsis, burns) or provoked by bacterial toxins/other cytokines (TNFalpha, IL1,6,10) Decreased expression of thrombomodulin o secondary to endothelial damage Increased degradation (by neutrophils) of antithrombin +/ impaired synthesis of antithrombin high levels of PAI-1 which depresses fibrinolysis [snake venoms activate factor 10/2] There are four main causes of DIC Infections (g-ve sepsis, malaria) Cancer (acute leukaemia) obstetric (septic abortion, placental abruption, eclampsia) tissue necrosis (burns, trauma, liver disease) The clinical picture of DIC is BAD Widespread fibrin deposition within circulation = o MAHA (shistocytes on blood film) o Compromised blood supply to organs multiple organ failure particularly wary of kidney, brain, heart, liver, lung damage Widespread consumption of platelets and clotting factors = bleeding Prolonged PT,APTT, TT with Increased FDP and D-dimer low fibrinogen, protein C, antithrombin, platelet A diagnosis of DIC is difficult but an ISTH score >=5 can be suggestive 1 2 3 Platelet <100 <50 FDP ‘moderate increase’ ‘strong increase’ PT prolonged by 3-6s prolonged by >6s fibrinogen <1 DIC is always secondary to another disease – you must treat the cause supportive measures can be given in the mean time o blood transfusion if blood loss/anaemia is severe o replacement coagulation factors (FFP/PCC) [FFP15ml/kg body weight] o platelet transfusions 1unit/10kg body weight when it drops below 50 o cryoprecipitate when fibrinogen <0.8g/l o Protein C/ TFPI have some use in sepsis induced DIC [PC causes haemorrhage] 2. Cardio-pulmonary bypass is used to prevent excessive blood loss in cardiac surgery The principle is diverting the circulation (which is heparinised) over a non-biological surface in an oxygenator. The surface is lined with polyurethane, polypropylene and PVC. Preventing excessive blood loss in cardiac surgery reduced mortality and decreases need for transfusions The risks of bleeding in CPB are largely associated with platelet dysfunction administration of preoperative aspirin turbulence/stress in the machine (extra-corporeal circuit) = MAHA & similar damaging affect on platelets [drop in platelet count by upto60%] contact with ‘alien’ surface = activation of fibrinolysis, inflammatory mediators, complement hypothermia may be experienced in surgery – this is associated with defective thromboxane A2 synthesis by platelets = impaired aggregation The dysfunction usually reverses within 3 hours of coming off the machine aprotinin is an inhibitor of plasmin and kallikrein. it used to be used to decrease bleeding risk but was associated with increased risk of MI, renal failure and stroke. [These risks are not seen with other antifibrinolytics eg tranexamic acid] if patients bleed in CPB– avoid transfusion (associated with renal failure, infection) and give platelets 3. Bleeding associated with uraemia is again largely due to platelet dysfunction The clinical picture including bruising, epistaxis, Gi bleeding and intracranial haemorrhage o uraemic haemorrhage can be fatal Bleeding is contributed to by: o platelet dysfunction impaired aggregation storage pool defects decreased thromboxane A2 production increased platelet calcium content o defective platelet/vessel wall adhesion o low haematocrit (anaemia) platelet dysfunction is caused by guanidosuccinic acid – which is produced by an abnormal ammonia detoxification pathway that occurs in uraemia Management of uraemic haemorrhage o correct anaemia (transfusion) o DDAVP o Cryoprecipitate o Conjugated oestrogens 1.25 – METABOLIC DISORDERS ASSOCIATED WITH THROMBOSIS 1. There are 7 well known disorders associated with an increased risk of thrombosis Homocyteinuria malignancy pregnancy post-operative drugs haemolytic anaemias hyperviscous blood o plasma mediated (Ig’s, myeloma, Waldenstroms macroglobinuria) o cell mediated (myeloproliferative disease, leukaemia) 2. High levels of homocysteine are associated with an increased risk of atherosclerosis Physiology of Homocysteine produced during synthesis of methionine It is usually metabolized in two pathways: o transulphuration to cysteine (vitamin B6 & cystathione beta synthetase dependent) o remethylation to form methionine (dependent on vitamin B12/folate amd the enzymes MS, MTHR) normal level 5-15microM/l; severe levels are >100microM Homocysteine promotes development of atherosclerosis by 3 mechanisms Production of oxidants o hydrogen peroxide damages endothelium o hydroxyl radicals oxidize lipids in LDL Endothelial dysfunction o inhibition of TM, heparan sulphate & NO synthase o induction of TF SMC proliferation is stimulated Homocysteinuria is associated with defects in normal homocysteine metabolism Cystathione b-synthetase deficiency is an AR disease where homocysteine level is >100microM A polymorphism in MTHFR (C677T) makes the enzyme more thermolabile – this variant is more common in CHD/ coronary stenotic patients Homocysteinuria is associated with skeletal deformities, lens dislocation and intellectual handicap alongside increased arterial, and possible venous, thrombosis Cyanide-nitroprusside test [brand’s test] can diagnose it by detecting urinary H-cytstine 3. Thrombosis in PNH is largely due to complement-mediated RBC lysis which leads to excessive free circulating haemoglobin Normal protection from complement mediated lysis The PIG-A gene codes for a protein that anchors GPI to red cells GPI has a number of surface molecules including CD55, CD59 and CD87 CD55 increases the rate of dissociation of the complement complexes c4b2a and c3bbb CD59 prevents c8-c9 interaction and this inhibits the classical complement pathway CD87 usually binds u-PAR to stimulate plasmin production PNH is an acquired somatic mutation in PIG-A lack of protection GPI makes red cells vulnerable to complement mediated lysis o this leads to intravascaular haemolysis at night and haemoglobinuria in the morning o loss of CD87 function also means there is less fibrinolysis Increased cell lysis gives high levels of circulating Hb (and arginase) which increases thrombotic risk o free Hb activates endothelium, inflammation, thrombosis and irreversibly reacts with NO to form metHb & nitrate o less NO = dystonia in VSMCs, endothelial dysfunction, platelet aggregation and platelet activation Haptoglobins usually bind free Hb and are degraded by monocytes. another safeguard is haemopexin which takes Hb to the liver Thromboembolism accounts for upto 2/3 deaths in PNH and commonly occurs in hepatic, portal, and mesenteric veins and the sagittal sinus eculizumab stops assembly of MAC and thus reduces the number of thrombotic events 3. Myeloproliferative diseases associated with the JAK2 mutation increase thrombosis risk by activation of platelets and cell-mediated blood hyper-viscosity Thrombosis is the leading cause of death/morbidity in myeloproliferative disease PRV = increased red cell mass; 12-39% patients present with thrombosis ET = increased platelet count >600 for >6weeks; 11-25% patients present with thrombosis The JAK2 V617F mutation increases thrombotic risk in myeloproliferative disease This JAK2 mutation increased Hct, WBC, TF, TM and adhesion molecule production (p-selectin) The mutation also seems to make platelets hyper-active by inducing c-mpl expression High Hct not only increases blood viscosity but increases platelet adhesion to endothelium Higher WBC contributes to thrombosis mainly via activated neutrophils and monocytes: o neutrophils aggregate with platelets o monocytes make TF o production of pro-inflammatory cytokines Large vessel thrombosis is more common in myeloproliferative disease Cells migrate axially so platelets are displaced to vessel wall o inter-platelet and platelet-vessel wall interactions increase Upto half of sufferers of hepatic vein thrombosis (Budd-Chiari) have underlying MPD thrombosis risk increase with age, previous thrombosis, raised HCT, clonality in white cells (seen in ET) Low dose aspirin can decrease the number of thrombotic events 1.26 – THE MULTIPLE ROLES OF THROMBIN IN COAGULATION 1. Thrombin has multiple procoagulant and anticoagulant roles Procoagulant Anticoagulant Anti-fibrinolytic Role Fibrinogen fibrin F5 F5a F8 F8a F13 F13a F11 F11a Cleavage of PARs & GP5 stimulates production of F10a (via 5a) and hence the 10a-antithrombin complex Activates Protein C Activates TAFI Cofactor none needed Fibrin GP1b GP1b Heparan Sulphate TM TM Exosite 1 ? ? 1 2 2 2 1 1 2. The main structural features of thrombin and 2 hidden exosites generation of thrombin from prothrombin exposes hidden exosites exosites bring substrate into the active site cleft the active site serine is number 195 3. Thrombin uses exosites to bind to different cofactors and extend the range and increase specificity of its interactions The initial procoagulant role of thrombin do not require cofactors o during fibrinogen cleavage thrombin uses exosite I, a sodium loop and its active site exosite 1 binds to the fibrinopeptides o it uses numerous different residues for recognition and interaction of F5 and F8 Thrombin uses the same residues to recognize Antithrombin, Protein C and F13 The key residues are W50, E229 and R233 to recognize antithrombin It uses exosite II to bind heparin/heparan sulphate when forming the thrombin-antithrombin complex o i.e exosite II binds the cofactor for the reaction which is catalysed by antithrombin It uses exosite I to bind TM o i.e. exosite I binds the cofactor for the reaction catalysed by thrombin By cleavage of fibrinogen, it generates its own cofactor (fibrin) for the activation of F13 4. From initial generation – the main regulation of thrombin activity is driven by exosite competition the cofactor sites on thrombin for fibrin and TM overlap – this suggests competition for exosite I o this competition halts unregulated platelet plug expansion GP1b complex assists thrombin in binding to PAR/GP5 on platelet surfaces. It competes with heparin/heparan sulphate for exosite 2 o this competietion halts unregulated platelet activation Lastly, antithrombin and heparin cofactor 2 mop up any excess thrombin 1.27 - DEVELOPMENTAL HAEMOSTASIS IN THE NEONATE 1. Differences in fetal coagulation factor and platelet quantity and quality account for coagulation disorders seen in the newborn coagulation factors do not cross the placenta; synthesis starts in utero from about 10weeks and levels increase as term progresses o hence PT, APTT and TT all decrease as term progresses haemostasis is ‘impaired in the newborn because of: o decreased synthesis & accelerated clearance of coagulation factors o synthesis of proteins with decreased functional capacity o fetal/newborn megakaryocytes are small and less mature o platelet responses to certain stimuli may be impaired in the fetus/newborn 2. Factor 8 & fibrinogen reach adult values at term, otherwise newborns are largely vitamin Kdependent factor deficient Factor % of adult value reached at term F7 53% F9 32% F10 40% Prothrombin 44% F8 94% Fibrinogen =>100% 3. Acquired coagulation/platelet disorders Acquired haemostatic disorders in the newborn: haemorrhagic disease of the newborn (HDN) DIC liver disease Neonatal thrombocytopenia HDN is due to vitamin K deficiency poor placental transfer of vitamin K low fetal vitamin K stores low vit K content of breast milk absent bacterial vit K synthesis in neonatal gut immaturity of fetal liver HDN usually presents within a week Haemorrhages in the brain, GIT, post circumcision and excessive bruising/purpura Diagnose with prolonged PT Manage with prophylactic and/or episodic Vitamin K or FFP if bleeding is severe HDN classification early classic late Time of presentation within 1 day within 1 week 2-12weeks causes maternal drugs physiological [see above] liver disease, breast feeding The principle of treating neonatal DIC is the same as always – treat the cause Infection Necrotizing enterocolitis Asphyxia Meconium aspiration Placental abruption Retained dead second twin Diagnose with prolonged PT, APTT, TT, low Plt + high FDPs. Treat underlying cause and may need to give platelets/FFP if bleeding is severs Neonatal thrombocytopenia is the commonest abnormality in newborn babies Reduced platelet production o transient - maternal HTN/ DM and fetal IU growth restriction o rare – BM failure, fanconi anaemia Increased platelet clearance o immune mediated - maternal ITP, neonatal alloimmune thrombocytopenia o non-immune mediated – DIC, infections (CMV, rubella) The mechanism of NAITP involves HPa1a antibodies Mother is HPA1a negative Fetus inherits HPA1a from father Mother produces antibodies against fetus which can cross the placenta this occurs 1in1500 preganacies – it is the commonest cause of severe thrombocytopenia in newborn infants Manage with HPA1a-negative platelet transfusion. most cases are transient and resolve within 3-4weeks as the antibodies are cleared. 4. Inherited coagulation disorders Inherited haemostatic disorders in the newborn: Haemophilia A/B T3 vWD Rare coagulation factor deficiencies Haemophilia is the commonest inherited coagulation disorder and is frequently diagnosed post circumcision affected boys may present with excessive bleeding after circumcision, cephalohaemoatomas, ICH of bruising after blood sampling long APTT and suspect factor assays give oral vitamin K 1.28 - ARTERIAL THROMBOSIS [this lecture was not actually given] 1. The intiation of atherosclerotic lesion formation starts with fatty streak formation Streaks begin to form by end of first decade Sites that are predisposed to a pattern of flow that affects endothelial permeability (high shear/ low shear bifurcations etc) are particularly affected The change in permability leads to retention of LDL which is oxidised in the ECM Oxidised LDL production leads to endothelial dysfunction: o Expression of adhesive molecules eg selectins, VCAM, ICAM and chemokines eg MCP1 o Reduced NO production Diets etc which predispose to high circulating LDL/low HDL (which usually inhibits LDL uptake into endothelium) accelerate plaque formation 2. Platelets adhere to plaque prone sites because of dysfunctional endothelium Platelets do not usually bind to endothelium (prostacyclin, NO) Decreased NO production & selectin expression allows platelets to bind to dysfunctional endothelium o Firstly platelets bind and roll, just like when they normally bind subendothelium, to endothelial p-selectin via GP1a o Secondly, Firm adhesion is mediated by GP2b3a which binds to fibrinogen or vWF - this causes degranulation of platelets Activated platelets achieve the following roles: o Release of vWF etc and subsequent thrombus formation o Recruitment and activation of monocytes via p-selectin receptor o SMC proliferation via TGF/PDGF o Further LDL retention via PF4 3. Macrophages play a key role in forming foam cells Enzymes released from macrophages may speed up LDL oxidation and cause tissue damage Macrophages eat oxidised LDL to form foam cells, which subsequently die and release of lot of TF The local tissue damage leads to fibrous cap formation on the surface of a core of dead macrophages o Necrotic lesions become calcified by pericyte-like cells in the intima Occlusion is mediated by plaque rupture and release of TF o Plaque rupture is to do with instability rather than plaque size o Plaque progression is stimulated by HTN, hormones, infection 4. The role of vWF in atherosclerosis vWF stimulates WPB production, and WPBs contain inflammatory and angiogenic mediators elevated vWF is associated with acute occlusions experiemnts in vWF deficient mice show less leukocyte recruitment and reduced atheroma formation other murine stroke models have shown vWF increases infarct size in stroke (and ADAMTS13 reduces infarct size) aptamer (anti vWF A1) and abciximab (anti GP2b3a) are both potential targets for vWF, aptamer seems to have a higher therapeutic index 5. the role of coagulation factors in atherosclerosis F5leiden prothrombin G20210A and anticoagulant deficiencies have weak associations for IHD/stroke o this may be because available data is poor warfarin is more effective than aspirin but you need to aim for INR3-4 or combine it with aspirin to prevent second MI o ACCP and NICE recommend aspirin because warfarin is more costly and has higher bleeding risk 1.29 - BLANCING THE RISK IN MANAGING THROMBOSIS 1. There are many problems associated with administrating long-term anticoagulation Fatal haemorrhage Non-fatal but clinically relevant haemorrhage o Bleeding tendency increases with age o Risk of bleeding is highest when treatment is initiated Regular blood testing Lifestyle/ diet restrictions Drug interactions 2. However, there are also clear risks in not administrating long term anticoagulation First VTE (PE can kill you. DVT won’t) Recurrent VTE o DVTs predispose to DVTs, and PEs predispose to PEs (idea that some people are just prone to forming embolic thrombi) o F5liden people tend to form DVTs if untreated Post-phlebetic syndrome o Pain, swelling, ulcerations; requires 2 years of TEDs after first clot Patient anxiety 3. They key is knowing who is at an increased risk of forming a clot, and of those, who is at an increased risk of VTE recurrence Risk factors for first VTE - asymptomatic thrombophilic patients F5 leiden is a less strong risk factor for thrombosis than PC/PC/AT deficiency Common polymorphisms can combine to increase risk of developing spontaneous VTE Warfarin does more harm than good in people with just pure AT deficiency >50% of thrombophilic people get their first VTE because of a transient risk factor o So the key might be preventing exposure to these factors Cancer also predisposes to thrombus formation Risk factors for recurrence Previous PE has higher risk of recurrence than DVT Idiopathic VTE has higher risk of recurrence than VTE due to transient risk factor (surgery) Male APS Some thrombophilias Increased levels of d-dimer Increased ETP (endogenous thrombin potential) Presence of Residual vein thrombosis 4. Simple guidelines have been developed for management There is no need to anticoagulate asymptomatic thrombophilic patients without prior clot Laboratory tests are generally poor predictors of recurrence in thrombophilic patients o Although d-dimer may be useful You should consider anticoagulation for thrombophilic people who have had a clot if the predictive risk of recurrence is >12.5% and relative risk >5% [but availability of data is poor] It seems that most people remain at a high risk of thrombosis between 3-6months after a first clot, it is unclear whether this risk plateaus after 6 months or begins to decline Genotype-based profiling may be more accurate in predicting risk of recurrence First VTE due to transient risk factor Cancer associated VTE First idiopathic VTE First VTE in thrombophilic patient Recurrent VTE Aim for an INR between 2.0-3.0 3months VKA LMWH 3-6months VKA 3-6months (?lifetime) VKA 3 months (?lifetime) Lifetime VKA 1.30 – NORMAL ENDOTHELIAL FUNCTION 1. The endothelium is an organ with a complex structure and a variety of functions Structure of endothelium it is a single flat layer of cells that forms the interface between tissues and blood endothelial cells line the entire circulatory system cells appear in a cobblestoned morphology in vitro cells appear in an aligned morphology in vivo - and this is due to the effect of blood flow/ shear stress; with cells aligning parallel to flow overlaps between cells in vivo occur at junctional areas – this helps them to regulate barrier function The endothelium has 5 main functions regulation of vascular tone barrier function pro-inflammatory anti-coagulant angiogenesis 2. the regulation of vascular tone is achieved by balancing production of vasoconstrictive and vasorelaxing mediators The immediate response of the newborn is to upregulate vasorelaxing agents and downregulate constrictive agents in small pulmonary arteries. failure to do so would result in death Nitric Oxide has differing effects on endothelial cells and SMCs It is produced in endothelial cells from arginine by NOS eNOS is constitutively expressed in endothelial cells – it maintains a constant production of NO o eNOS can be induced by shear stress, O2, ACh and bradykinin o iNOS is induced in inflammation, nNOS is only produced by neurons NO improves endothelial barrier function, growth, motility and promotes angiogenesis (by promoting VEGF) NO diffuses to SMCs to bind to solugble guanylyl cyclase. this produces cGMP which in turn produces PKG o Hence NO causes SMC relaxation but inhibits SMC growth and motility NO also has anti-inflammatory and anti-thrombotic (platelet adhesion inhibition) effects Prostacyclin causes cell membrane hyperpolarization it is produced in endothelial cells from arachidonic acid via COX it elevates cAMP in SMCs. this activates potassium channels and inhibits calcium channels – net effect is hyperpolarization of the membrane and vasodilation o it also inhibits SMC proliferation Prostacyclin also inhibits platelet aggregation Natriuretic peptides there are 3main types, synthesized in the atria (ANP), brain (BNP) and endothelium (CNP) they bind to particulate guanylyl cyclase (not soluble) on SMCs to induce cGMP formation and achieve vasodilation they are stimulated by arterial/ventricular dilation and neurohumoral factors Endothelin-1 has 2 types of receptors; only one of which is expressed by endothelial cells it is produced in the endothelium under the influence of hypoxia, shear stress, certain cytokines and toxins it binds to Eta receptors on SMCs to cause vasoconstriction and proliferation It also binds to ETb receptors on SMCs, but this only causes vasoconstriction o it has the opposite effect if it binds to ETb receptors on endothelial cells themselves, because this induces production of prostacyclin and NO o there are no Eta receptors on endothelial cells Angiotensin II also has two receptors; both of which are expressed on endothelial cells It is produced by the rennin-angiotensin system It binds to AT1 receptors to achieve the following functions: o TF & thromboxane production – procoagulant o Endothelin1 & ROS production – vasoconstrictive ROS inhibits NO when it binds to AT2 receptors – bradykinin receptor expression is upregulated and this achieves a vasorelaxing function by induction of eNOS. Summary vasorelaxing vasoconstricting Molecule NO Prostacyclin natriuretic peptides Endothelin1 Angiotensin2 Thromboxane mechanisms soluble GC cGMP; opposite effects on EC/SMC cAMP hyperpolarization bound GC cGMP Eta receptor – vasoconstrict & SMC prolif ETb receptor – opposite effects on EC/SMC AT1 – procoagulant & vasoconstrictive AT2 – upregulation of bradykinin receptor increases ROS, decreases NO 3. Barrier function is achieved by inter-ceullar junctions, and can be modified by changes in intracellular cytoskeletal properties There are 3 types of endothelial junctions 2 of them play a role in barrier function: o adherens junctions (proteins, cadherin, PECAM1) o tight junctions (occluding, claudin, JAMs) 1 of them plays a role in signaling by being permable to cyclic nucleotides (<1kDa) o gap junctions (connexins) junctional proteins adhere to intracellular actin which gives junctions stiffness and adequate positioning remodeling of actin causes leaky junctions thrombin, histamine, endotehlin, TNF and hypoxia all induce Rho GTPases o Rho GTPases inhibit MLCphosphatase and this leads to greater phosphorylation of myosin light chain o calclium influx also achieves this by stimulating MLCkinase o greater phosphorylation leads to remodlling of actin microfilaments into actinomyosin fibres; which causes cellular contractility and barrier dysfunction Barrier function is maintained by Rac1 GTPases – these confer cellular tethering o Rac1 is induced by sphingosine1phosphate and HGF 4. angiogenesis is a multi-step procedure; each step can be interfered with the main steps are: breaking cell-cell adhesions (to allow diffusion of growth factors from blood into tissue) basement membrane degradation cell migration morphogenesis of new vessels 5. The endothelium is naturally anticoagulant Anticoagulant Prostacyclin NO TM ProteinS Heparan sulphate tPA annexin5 (competes with factors to bind PL) TFPI Ecto-ADPase (inhibits ADP-mediated platelet aggregation) Procoagulant TF vWF PAI1 Inflammation, shear stress, metabolic stress (LDL) and oxidative stress (superoxide) all shift the endothelium to a pro-coagulant state 6. the endothelium produces pro-inflammatory molecules which makes it pro-coagulant the production of pro-inflammatory cytokines (IL1, TNFa) suppresses TM and stimulates TF, PAF and adhesion molecules o leukocyte adhesion triggers release of superoxide which causes endothelial damage hence inflammation leads to a pro-coagulant state o this is good because it can restrict spread of infection e.coli and salmonella have adapted by recruiting plasmin to their surface strep have adapted by the ability to produce streptokinase (tPA like) o this is bad because it can increase the risk of developing cardiovascular disease 1.31 – THROMBOSIS & EMBOLISM: GENETICS AND DETECTION 1. VTE is a single disease entity comprising both DVT & PE DVT & PE share many characteristics Identical pathophysiology o predisposing risk factors leads to thrombus formation in veins o thrombi form legs/pelvis embolise to pulmonary circulation 90% of PEs attributable to leg thrombi; 10% pelvic about 50% of people with DVT develop a subsequent PE o increasing thrombus size leads to destruction of venous valves o destruction of venous vlaves gives rise to post-phlebitic syndrome Similar risk factors o pregnancy, HRT, orthopaedic surgery, thrombophilia, flights etc o Basically, Virchow’s triad Identical therapeutic goals similar treatment strategies both DVT & PE present with non-specific symptoms and a clinical diagnosis is hence unreliable symptoms of inflammation o pain, swelling, redness, warmth unilateral signs o leg – pitting oedema, tenderness, muscle induration o lung – pleuritic chest pain, haemoptysis systemic upset – purexia, tachycardia 2. Diagnosis of DVT can make use of d-dimers and ultrasound The simplified wells score is used to assess pretest probability for DVT Risk factor Ca, paralysis, bed>3d, surgery within 4wk, vein tendereness, swollen leg, calf swollen>3cm, pitting oedema, collateral veins, previous DVT alternative diagnosis Low risk/unlikely <1 Moderate 1-2 point (any one) 1 -2 High/likely >2 If someone has a low risk from history, a negative d-dimer means they probably don’t have a DVT because d-dimers have a high negative predictive value o the cut off for d-dimer reading is proportional to its specificity if someone has a high risk from history, negative d-dimer does not mean no DVT. high risk patients should always have an ultrasound if someone has low risk from history, negative ultrasound probably confirms the diagnosis; but ultrasound is only sensitive 97% of the time – they may still require venogram/serial ultrasound within 1 week if the history points to very high risk. Venograms are rarely used these days in DVT invasive, expensive, dangerous contrast mediated effects on kidney (especially in HTN, T2DM) reserved for people with high risk from history and normal USS – this may suggest recurrent DVT (which USS is poor at picking up) o recurrence is diagnosed if vessel diameter has enlarged by 2mm or more from previous venogram 3. Diagnosis of PE can make use of d-dimers and V/Q or CTPA Simplified wells score for PE Feature DVT, tachy >100, immobility or surgery 4 weeks ago, previous VTE, haemoptysis, Ca, most likely than alternative diagnoses Score (any one) 1 PE is deemed unlikely if score is <1 V/Q is only diagnostic in 30% of cases, but it should be used before CTPA in the interest of decreasing radiation exposure V/Q may be influenced by any coexisting lung disease TTE is the test of choice in a massive PE you are looking for signs of RV stress/dilation in the emergency situation with TTE then confirm diagnosis with VQ of spiral CT avoid CTPA because it increases risk of major bleeding in massive PE patients 1.32 – ANTIPHOSPHOLIPID SYNDROME 1. The antiphospholipid syndrome is an autoimmune disorder associated with a pro-coagulant state Definition & classification of APS APS is an AI disease, where Abs react with phospholipids/ CSM glycoproteins, leading to invivo increased risk of arterial & venous thrombosis primary APS occurs in the abscence of other AI disease secondary APS occurs in conjunction with diseases eg SLE, RA, scleroderma etc catastrophic APS is a very rare variant which causes multi organ thrombosis and is always fatal Most patients develop low titre APS Abs without actually having thrombosis Lupus anticoagulant antibodies o target prothrombin and beta2glycoprotein 1 o have differing effects in vitro (anticoagulant) as opposed to in vivo (pro coagulant) o rare o beta2GP1 Abs have the highest thrombogenic potential o PT Abs associated more with arterial thrombosis rather than venous anti-cardiolipin antibodies o cardiolipin is a highly charged part of the PL bilayer o these are 5x more common than lupus anticoagulant Abs o only thrombotic when in moderate-high titres o usually IgG and/or IgM other APS Abs target lipoprotein surface antigens and components of the coagulation/fibrinolytic systems 2. the pathogenesis of antiphospholipid syndrome is unknown inhibition of protein C/fibrinolysis? inhibiting the normal anticoagulant effects of beta2GP1 stimulation of platelets, endothelial cells, monocytes o stimulation of TF production by monocytes o upregulation of adhesion molecules on endothelial cells o stimulation of thromboxane A2 synthesis by platelets? 3. antiphospholipid syndrome is diagnosed based on clinical and laboratory findings The revised Sapporo classification diagnoses APS when one clinical and one laboratory finding are met, between 12weeks and 5years of each other. Clinical criteria – vascular and obstetric events Vascular events – a history of one or more arterial/venous thrombosis episodes, objectively diagnosed by imagining, with no evidence of vessel wall inflammation Obstetric events – requires only one of the following: o >3 spontaneous and unexplained abortions prior to 10weeks gestation o >1 miscarriage beyond 10weeks gestation o >1 premature birth due to pre-eclampsia, eclampsia or placental insufficiency placental insufficiency can be due to HTN/ T2DM in ACS, placental insufficiency leads to intra-uterine growth restriction Laboratory criteria ELISA to detect anti-cardiolipin antibodies at medium or high titres, at least twice in more than a 12 weeks period o illness etc can induce transient APS Abs production in normal people Prolonged coagulation in dilute Russell’s viper venom time demonstrates lupus anticoagulant only when o normal plasma addition does not correct the prolongation o addition of phospholipids (dilution of antibody) does correct the prolongation 4. although most patients prevent with VTE, APS patients clot in unusual places Common clinical findings: vascular o VTE prevalence is roughly 30% o recurrence rate of untreated patients is 10%; this carries a higher mortality rate o cerebral thrombosis is most common arterial thrombosis event o digital necrosis and gangrene may also be seen cardiac – valvular heart disease neuro – TIA/stroke, vascular dementia skin – livedo reticularis (rash that appears reticular) renal – vasculopathies chronic reanl ischaemia rare clinical findings Thrombocytopenia (splenic sequestration following Abs binding to Plt PL) pulmonary HTN peripheral thrombosis catastrophic APS 5. treatment of APS in obstetric medicine Lupus anticoagulant patients with high titre anti-cardiolipin bodies have greatest thrombotic potential and are at much higher risk of obstetric complications APS is also consistenly associated with intra-uterine fetal ?disease, pre-eclampsia development and the HELLP syndrome (haemolysis, eleveated liver enzymes, low platelets) heparin and low dose aspirin are being used as prophylaxis to prevent (recurrent) miscarriages steroids should only be used in treatment of coexisting AI disease, not to treat APS (side effects). 1.33 – WARFARIN & HEPARIN; USE AND MONITORING 1. Warfarin & heparin have very different mechanisms of action warfarin prevents recycling of vitamin K and hence prevents gamma carboxylation of vitamin K dependent factors so that they can no longer bind PL via their gla domains. o hence vitamin K (or FFP and PCC in urgent situations) can reverse it o resistance arises due to compliance (false resistance), vitamin K diet, cytochrome p450 induction/polymorphisms heparin is a polysaccharide of repeating Nacetylgalactosamine and n-acetylglucosamine o enhancement of antithrombin = inhibition of all SPs, mainly thrombin and 10a o release of TFPI from GAGs on endothelial cell surfaces o iactivation of thrombin via heparin cofactor2 o interactions with fibrinogen/TAFI? 2. Warfarin & heparin both have side affects apart from haemorrhage warfarin o skin necrosis (sever protein c deficiency, commonly manifests in adipose tissue) o Chondrodysplasia punctata in utero (teratogenic in 1st trimester; failure of epiphysis fusion) o Purple toe syndrome (disruption of atheromatous plaques leading to cholesterol emboli lodging distally) heparin o bleeding (protamine is the antidote) o heparin induced thrombocytopenia o hyperkalaemia, osteoporosis, alopecia 3. different tests are use to monitor warfarin/heparin warfarin; INR o Target 2-3 for patients afte first VTE, AF, caridomyaaothy and vavular heart disease o target 3-4.5 for recurrent VTE, valvular heart disease and some thrombophilias heparin – APTT o aim for APTT ratio of 2.0 o LMWH gives a more predictable response than UFH 1.34 – NEW ANTICOAGULANT AGENTS; DESIGN & PRACTICE 1. New oral anticoagulants are deisgned to act at specific targets in coagulation potential targets in anticoagulanbts o TFPI/PC/APC analogues o f9, f10a, thrombin, tafi inhibitors o rThrombomodulin requirements of new agents o efficacy – proven in arterial/venous thrombosis o safety – wide therapeutic window, low bleeding risk, predictable response, antidote presence o convenience – oral, fixed dosage, few interactions, rapid on-&offset of action, no need for monitoring Feature rapid onset rapid offset predictable response lmited interactions antidote cost oral administration warfarin + + + UFH + + + + - LMWH + ? + + + - 2. Some examples of new agents in clinical practice synthetic pentasaccharides – can be used in VTE & HIT; o fondaparinux vte prevention but requires parenteral (SC) admin excreted by kidney so cant be used in renal failure not reversible by protamine o idraparinux longer half life than fondsparinux factor 10a inhibitors – few functions outside coagulation o natural options – tick anticoagulant protein and antistasin o rivaroxaban licensed for orthopaedic vte prophylaxis, stroke prophylaxis in AF no antidote thrombin inhibitors o dabigatran licensed for orthopaedic vte prophylaxis, stroke prophylaxis in AF protein C analogues o drotrecogin-a is rAPC – used in sepsis that causes multiple organ failure but very expensive 1.35 - ENDOTHELIAL DYSFUNCTION 1. The pathogenesis of endothelial dysfunction is closely linked to low/turbulent shear stress Mechanical injury (shear stress) is one of four broad causes of endothelial dysfunction Inflammation (infectious or immune-mediated) Apoptosis & necrosis Oxidative stress o Rapid reoxygenation following hypoxia generates reactive radicals MECHAINCAL INJURY o Particulary low or turbulent blood flow o Blood pressure leads to circumferential stretch too Normal Shear stress is important for the healthy endothelium Shear stress is higher in arteries than veins (upto 15-30x greater) Shear stress is normally required for: o NO production o Pro-coagulant molecule production o Growth factor & adhesion molecule expression Shear stress affects endothelium by activating signalling cascades via mechanosensors eg integrins, stress-activated cation channels, junctional proteins o Early effects = IP3, DAG = Ca influx = protein kinase activation o Later effects = TF/gene regulation; both pro-and anti-thrombotic genes are affected as well as some kinases and genes regulating the cytoskeleton o Late effects = cell alignment and migration with blood flow Failure of normal shear-stress endothelium interaction is implicated in pro-thrombotic disease At arterial branching points, shear stress is low or turbulent - this makes endothelial cells: o Cause vascular remodelling: display a cobblestone morphology o Cause vasoconstriction o Cause inflammation and thrombosis Similarly, dysfunctional endothelium that cannot adapt properly to shear stress will appear this way Stretch leads to junctional loss and monocyte adherence (role of HTN in atherosclerosis) 2. Endothelial oxidation of LDL is a key process in atheroma formation Recap of atherosclerosis Excessive inflammatory-fibroproliferation by the endothelium in response to vascular insult o Step 1 - fatty streak formation & adhesion of monocytes (reversible) o Step 2 - intermediate lesion with layers of macrophages & SMCs in the wall o Step 3 - fibrotic plaque covering a necrotic core (irreversible) o Step 4 - plaque cap ruptures, exposing the thrombus to blood flow Four things can happen to a thrombus after a plaque ruptures Completely/partially resolves Progresses and grows because of failure of normal anticoagulant/fibrinolytic mechanisms to cope. This can lead to vessel occlusion. Incorporation into vessel wall following fibroblast/ SMC migration Fragmentation and embolization Endothelial oxidation of LDL has the following functions Adhesive glycoprotein expression chemokine production to attract monocytes & lymphocytes pro-proliferative growth factor/ cytokine production contributes to fibrous plaque formation The dysfunctional endothelium also prevents senescense/repair, loses anti-thrombotic function and may express receptors for viruses, particularly Kaposi sarcoma and herpes viruses. Treatment = statins, anticoagulants, vasodilators 3. The problem in pulmonary HTN is increased vasoconstrictor production by the endothelium The Dysfunctional endothelium begins to cause vaso-active imbalance in pulmonary HTN Increased vasoconstrictors (endothelin, angiotensin) Decreased vasorelaxants (prostacyclin, NO) Reduced expression of voltage gated K channels [reduced response to prostacyclin] Pro-proliferative and pro-fibrotic cytokine productions (VEGF, PDGF) Increased cell permeability and inflammatory cell migration Vascular changes in pulmonary HTN SMC proliferation = intimal thickening/luminal narrowing Fibroblast proliferation = fibrosis, ECM deposition o Vasculature adopts Plexiform lesion appearance due to disorganised angiogensis Vasoconstriction o Some vasoconstrictors have dual effects as growth factors and hence play a part in proliferation too Thrombosis o Pulmonary HTN patients show higher levels of TF, fibrinopeptides, PAI1, vWF A few patients with pulmonary HTN develop chronic thromboembolic pulmonary HTN the problem here is embolised DVTs interactions occur between fibrin/thrombin from the embolus and the pulmonary endothelium the endothelium begins to produce more vasoconstrictors and down regulated thrombomodulin (pro-coagulant) in the context of concomitant hypoxia/inflammation, the net result is vessel occlusion and remodelling Management = inhaled NO, IV prostacyclin/prostacyclin analogues, anticoagulants, antiinflammatories, calcium channels blockers and phosphodiesterease inhibitors (no 1 effective treatment) 4. Endothelial-and platelet derived microparticles are prothrombitc and play roles in arterial disease and cancer Microparticles are often released following apoptosis or activation of platelets/endothelial cells. Release secondary to cell activation is due to cytoskeletal disruption MP release is induced by all four broad causes of endothelial dysfunction MPs show extracellular proteins of the parent cell, particularly TF and PPDserine, as well as intracellular signalling molecules eg DNA fragments/ micro RNA Chronic thromboembolic pulmonary HTN patients show increased microparticles in plasma - as well as pro thrombotic, they wre pro-angiogenic and pro-inflammatory in this disease Endothelial MPs are implicated in arterial disease, sepsis and cancer o Tumour MPs can prime distant sites for metastasis in cancer o MPs may be initially protective in sepsis 1.36 - COAGULATION, INFLAMMATION & SEPSIS 1. Coagulation and inflammation are closely intertwined Inflammation influences coagulation in 4 main ways thanks to the dysfunctional endothelium Increase in TF release (from tissues & monocytes) Down regulation of anticoagulant molecules (TM, EPCR, APC, TFPI, AT) Increased vWF production to stimulate platelet adhesion Decreased fibrinolytic capacity (increased PAI1 and downregulated tPA) 2. Further recap on the role of the endothelium in pathogenesis of atherosclerosis The starting point is induction of VCAM expression on endothelial cells, influenced by oxidised LDL Monocyte binding on VCAM leads to microparticle release In normal people, this step is required for monocytes to become activated to macrophages and mop up LDL - keeping the endothelium in balance In hypercholesterolaemia - excessive monocyte uptake leads to the formation of foam cells and release of TF microparticles by activated monocytes TF microparticles express PSGL and bind to activated platelets where they are decrypted to allow binding of 7a and initation of further coagulation o The net result is a pro-inflammatory, pro coagulant state T-cell binding on VCAM is key in activating monocytes Th1 and Th2 cells usually do this and release cytokines to activate uptaken monocytes into macrophages Excessive t-cell uptake gives excessive monocyte activation o The net result is a pro-inflammatory, pro-coagulant state Atherosclerosis demonstrates the pro-coagulant, pro-inflammatory cycle associated with dysfunctional endothelium The dysfunctional endothelium loses CSM proteins (including TFPI, EPCR, TM) due to activation of ‘sheddase’ enzymes It also increases transcription and release of vWF There is upregulation of PAI1, and downregulation of tPA dysfunctional endothelium Adhesion molecules are upregulated Cell-cell contacts are broken and the layer becomes ‘leaky’ o This leads to inappropriate turbulence over the atheroma haemostatic plug formation o This contributes further to extravasation persistence of proinflammatory and procoagulant processes Atherosclerosis Management of atherosclerosis Statins are lipid lowering and hence prevent endothelial dysfunction Anti-inflammatory agents may work with statins to prevent plaque progression/rupture Anti-platelet drugs prevent formation of occlusive thrombi post plaque rupture accumulation of foam cells, LDL, Ca lumen occlusion increased vessel wall mass 3. The same inflammation/coagulation cycle is implicated in sepsis infection SIRS sepsis severe sepsis septic shock death The disease continuum in infection can progress very quickly Criteria for SIRS requires >2 of the following: o Temperature >38oC or <36oC o Heart rate >90 beats/min o Respiratory rate >20/min o White blood cell count >12,000/mm3 or <4,000/mm3 or >10% immature neutrophils Sepsis terms SIRS which is due to infection (not trauma, burns etc) Severe sepsis is sepsis with atleast one organ failure Septic shock (which can be fatal) is severe sepsis with hypotension that is resistant to fluid resuscitation Thrombin may be implicated in sepsis pathogenesis Normally, WBC activation, pro-inflammatory cytokine production & coagulation are effective in combatting the pathogen and limiting its spread However, in sustained infection, these three processes, couple with excessive endothelial activation - lead to the same pro-inflammatory, pro-coagulation cycle seen in atherosclerosis The result is production of thrombin, which cleaves PAR-1 receptors on endothelial cells and platelets to: o Cause cellular contraction o Upregulate adhesion molecule production In sepsis the release of TF microparticles from monocytes is about 800x more than normal o Promote vascular permeatbility by upregulating S1P3 In sepsis this can contribute to dilutional coagulopathy o Promote NfKB 4. Neutrophils may play an important role in pathogensis of sepsis Functions of neutrophils in innate immunity against sepsis Phagocytosis Reactive oxygen species generation Enzyme release from granule Production of neutrophil extracellular traps (NETs) NETs can cause endothelial dysfunction NETs are webs of neutrophil DNA and associated histones, elastases, myeloperoxidases, that trap microbes within the vascular wall following uptake of neutrophils from bloodstream NET release is stimulated by pro-inflammatory cytokine release from activated endothelial cells/platelets Excessive cytokine production in sepsis causes neutrophil to release NETS whilst in the circulation to the following effects: o Trapping RBCs o Activation of platelets o Activation of contact system of coagulation In addition, histone H4 is cytotoxic and contributes to endothelial dysfunction Novel targets in sepsis Anti-histone H4, DNAase (cleaves nets) & APC (cleaves PAR1 but has opposing effects to thrombin) 1.37 – GENE THERAPY IN HAEMOPHILIA 1. The principle of gene therapy lies with introduction of a vector Gene therapy is deliberate transfer of genetic material into cells for therapeutic purposes there are two main methods: Correction of genetic deficiency by replacing a defective gene introducing a new gene that adds a new function eg increased sensitivity/resistance to a tertiary agent o the latter method is what gene therapy is moving towards gene therapy uses viruses as vectors disassembly of the viral genome incolves removal of infective (proliferatrive) parts what is left is the plasmid and accessory genes o the gene to be added is then inserted virus replication occurs inside eukaryotic cells copies of the recombinant gene are extracted when viruses are released from cells Retroviral vectors integrate into DNA, rAAV vectors do not 2. retroviral vectors have been used in disease but may have malignant side effects Retroviral vector use in Severe combined Immunodecificy XI the problem in SCID is defiecieny of gammaC chain of IL2 = T&B cell deficiency o most children die within 12 months if unteated bone marrow transplant used to be the treatment in SCID, but this had a high mortality gene therapy uses CD34+ HSCs, which are cultures, have the deficient factor added and transplanted back into patient o Most patients trialled have good T cell recovery with partial B & NK cell recovery o 5 year survival approaches 95% the problem is that the gene is an oncogene – increased incidence of t cell lymphoblastic leukaemia Chimeric antigen receptors are used in melanoma/CLL the principle here is extracting the host t cells that recognise the malignancy and redesigning their antigen receptor to recognise other molecules eg o CD19 (BCR) o CD137 (costimulatory molecule on T cells) o CD3-zeta (signal tranducer) the modified t-cells are cloned and reinfused o unfortunately the response rate is only 22% but this is better than the previous treatment the solution is to keep making the antigen receptor more specific 3. rAAV vectors are of use in haemophilia B rAAV vectors are more attractive than retroviral ones They are non-pathogenic and only become pathogenic in the presence of a helper adenovirus they have decreased immunogenicity they have more stable responses in the long term there is increased flexibility in administration regimens BUT o o once the cell with the vector inside dies – the vector is lost (because it doesn’t integrate with DNA) rAAV vectors can onlu hold small genes <5kb The advantages of using gene therapy in haemophilia B: it is a single gene defect, and rAAV therapy would would to 24/7 endogenous F9 production following a single gene transfer (avoids the 2-3 injections a week) the therapeutic goal is modest o the goal is to get from <1% to >1% F9 – this reduces morbidity and mortality signinifcantly the response to treatment is easily measurable via ELISA Current therapy involves prophylactic/recombinant F9 administration requires frequent injections given via central venous access very expensive (>110k/pt/yr) risk of bleeding is not completely eliminated o all groups (severe, moderate, mild disease) still have reduced life expectancy 80-90% of the world’s haemophiliacs do not have access to this treatment Nathwani et al are trialling AAV8 vectors in haemophilia B AAV8 avoids the immune response o it has low human-prexisting immunity, unlike the previously studied AAV2 it is more potent than AAV2 o addition of ‘self complimentary’ AAV8 makes the molecule ‘fold in’ on itself and makes rate of transcription faster it is highly specific for the liver o addition of a liver specific codon means only heaptocytes can recognize it – synthesis of F9 by hepatocytes is very efficient it can be administered peripherally (because of the codon) o this avoids the need for hepatic-artery injections (which were needed for AAV2), which are dangerous BUT – It takes a long time to make, is very expensive, and will be difficult to get worldwide the trial was made less risky by enforcing use of contraception ( to prevent germline transmission of vector), exclusing use of patients with F9 inhibitors/ previous immunity (inflammation), and using a low dose vector there seemed to be t-cell mediated IgM responses @20days and IgG responses at 50days to AAV8’s capsid in hepatocytes (demonstrated by deranged LFTs and high IFNgamma levels). patients on high dose AAV8 with short term steroids seem to be cured of haemorrhage and the need for prophylactic/eoisodic F9 treatment – WIN!! 4. gene therapy may have further use in haemophilia A and other diseases Difficulties in gene therapy for haemophilia A F8 gene is much bigger than F9 and exceeds AAV capacity F8 undergoes a lot of pos-translational modification so getting a hold of ‘wild’ F8 is difficult o the solution being tried is codon optimisation (taking out codons that are less important) of the F8 gene to make it small enough to fit into rAAV o seems to work in mice gene therapy may also be used in other coagulation disorders, lysosomal storage diseases, haematological and solid malignancies.