Bleeding Diathesis and prothrombotic tendencies in newly
advertisement

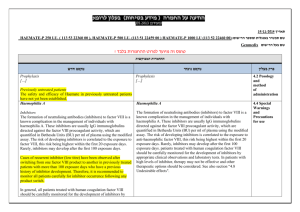
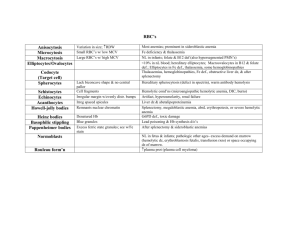
International Myeloma Working Group Abstract Bleeding Diathesis and prothrombotic tendencies in newly diagnosed systemic light chain Amyloidosis patients: important clinical implications in management Shameem Mahmood1, Anne Riddle2, Sajitha Sachchithanantham1, Thirusha Lane1, Darren Foard1, Taryn Youngstein1,Rabya Sayed1, Ketna Patel1, Marianna Fontanna1, Mark Coyne1, , Candida Quarta1, Carol J Whelan1, Helen J Lachmann1, Julian D Gillmore1, Philip N Hawkins1, Keith Gomez2, Ashutosh D Wechalekar1 1Division of Medicine, Royal Free Hospital Campus, National Amyloidosis Centre, University College of London Medical School, London, United Kingdom 2Haemophilia Department, Royal Free Hospital, Rowland Street, London, United Kingdom Background. Systemic light chain (AL) amyloidosis is known to be associated with increased bleeding diathesis, including the pathognomonic peri-orbital bruising. Little data exists as to the interplay of different coagulation factors, and prothrombotic risk in these patients, where thromboprophylaxis is an inherent part of our day to day practice. Aim. We sought to report the bleeding risks, coagulation factors and prognostic implications of any findings. Methods. We conducted a prospective study on 100 patients with suspected light chain amyloidosis, with 74 being systemic AL. Each patient had a detailed baseline assessment of organ involvement as per standard protocol, and completed a Royal Free Hospital v4 adapted bleeding questionnaire. Assays for vWF:Ag, Protein S, Protein C, Anti-thrombin III, fibrinogen, ADAMTS13, and all clotting factors were performed. Results. Among the 74 patients with systemic AL, 29 (39%) male and 32 (43%) with cardiac involvement, Mayo stage 3 in 29 (39%). 22 patients reported bleeding symptoms by the bleeding questionnaire, cutaneous (n=17), oral (n=7), epistaxis (n=5), haemarthrosis (n=1), muscle haematoma (n=1) and following surgery (n=2). Prolongation of the PT, APTT and TT occurred in 13 (17.6%), 13 (17.6%) and 35 (47.3%) patients respectively. Elevated fibrinogen levels were found in 42 (56.8%), FVIII 67 (90.5%) and vWF:Ag 67 (90.5%). Nephrotic Syndrome was present in 39 patients; an albumin less than 25g/L, significantly correlating with elevated vWF:Ag, FVIII, FV and fibrinogen, and reduced levels of protein S and anti-thrombin. Kaplan Meier estimates showed that a vWF:Ag (p=0.039) and FVIII (p=0.01) threshold greater than 280IU carried a significant survival disadvantage. By multivariate analysis, NT-proBNP, dFLC >180mg/L and FVIII >280IU/dL were factors independently impacting survival. Discussion/Conclusion. Newly diagnosed systemic AL patients are at risk of increased pro-thrombotic and bleeding diathesis. Our data shows that low levels of anti-thrombin activity and proteinuria were associated with albumin levels less than 25g/L, and an elevated FVIII and vWF:Ag levels greater than 280IU/L carried a significant survival disadvantage. The reasons are unclear, but may arise from endothelial damage and thromboembolic consequences. Thromboprophylaxis is an important consideration in all patients not having bleeding complications, irrespective of the chemotherapy therapy.