Morpho-functional peculiarities of neural system
advertisement

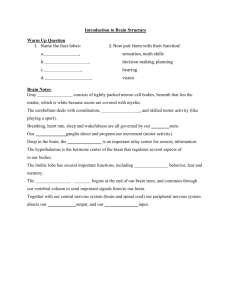
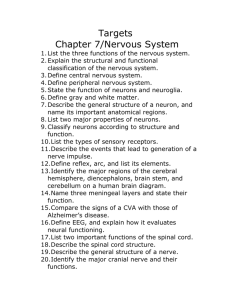
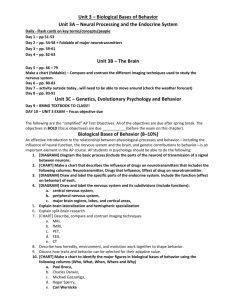
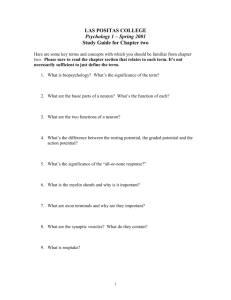
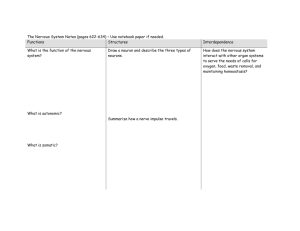
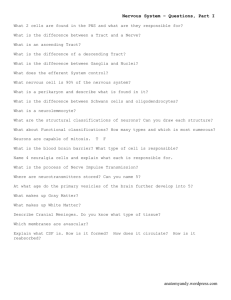
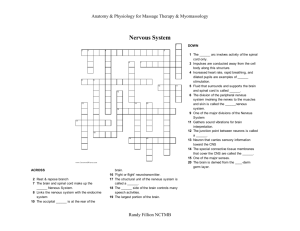
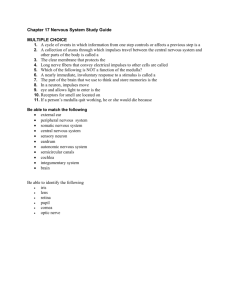
Morpho-functional peculiarities of nervous system Department of pediatrics The nervous system consist of the brain, the spinal cord, the peripheral nervous system, the autonomic nervous system sense organs (sight, heating, olfactory, taste, skin sensitivity). The main nervous system’s functions are: -psychological (intelligence) activity; -emotions -locomotion activity (function); -neural regulation of vegetation functions. - the nervous system realizes coordination of psychological and metabolic processes in different tissues, organs and systems and realizes connection between the organism and environment. The Brain During Development The nervous system develops from embryonic tissue called the ectoderm. The first sign of the nervous system developing is the neural plate that can be seen at about the 16th day of development. Over the next few days, a "trench" is formed in the neural plate - this creates a neural groove. By the 21st day of development, a neural tube is formed when the edges of the neural groove meet. The rostral (front) part of the neural tubes goes on to develop into the brain and the rest of the neural tube develops into the spinal cord. Neural crest cells become the peripheral nervous system. The nervous system is originated Forepart of medullar tube growths and gives the origin of brain bubbles during 5-6 weeks of intrauterine period. The nervous system is originated Five parts of brain – 2 hemispheria, connected by telencephalon, diencephalon, mesencephalon, metencephalon, myencephalon, are formed from back part of madullar tube. The Brain During Development Almost all the convolutions and fissures (gyre and sulcus) the brain is to possess in later life are present at birth, but they are extremely underdeveloped. The layers of the cerebral cortex are already almost completely formed at term, but differentiation of all the nerve cells occurs predominantly in the postnatal period. At the same time the spinal cord, the optic thalamus, and the corpus striatum are of a more mature structure. The cerebellum is elongated and its sulci are weakly pronounced. It is only towards the end of the first year of life that macroscopic structure of baby’s brain approaches that of an adult. Differentiation of the brain matter (nerve tissue, ganglionic cells and nerve fibers) is slower. Development of the spinal cord Critical period The most intensive fission of neural cells occurs between 6 and 18 weeks of intrauterine period. We call this period “the critical period” of CNS development due to possibility of the influence of various teratogenic factors to fetus nervous system, formation the defects of development of the nervous system is possible. Development of the brain Development Since the cortical layers of the brain of the newborn infant are little differentiated the formation of the cortical centers is also immature. An intensive development of the cerebral cortex takes place during the first three month after delivery. A most characteristic point is the absence of dendrites (arboraceous branches) in the nerve cells (neurons). Principal differentiation of the nerve cells is completed by the age of 3 years, although the final termination of the process occurs only at 8 years. The conduction routes (with the exception of the pyramidal pathways) are sufficiently developed at birth; the pyramidal routes myelinize by the time the baby is 5 or 6 month old. According the existing date the first neuron pathways to become myelinized in the cerebral hemispheres are the efferent routes, while pyramidal myelinization (the efferent pathway) occurs later. DEVELOPMENT OF MYELIN SHEATHS A significant aspect of brain development is the continued growth of myelin sheaths around the axons of the cerebral cortex. Myelin is a fatty substance which is deposited around many (though not all) axons as an insulating sheath. Its presence allows conduction of nerve impulses to occur from ten to one hundred times as rapidly as would occur along a non-myelinated axon. Since this obviously increases the efficiency of the axon system (just as increased computing speed enhances the efficiency of a computer), the development of axonal sheaths are taken as a measure of increasing maturity of the neural system involved. Myelin sheath development, or myelinization as it is called, has a rather well recognized time table in the cerebral hemispheres. Fibers serving the primary sensory (touch, vision, audition etc.) and motor areas are myelinated shortly after birth while those which are involved with more complex associative and cognitive functions myelinate later. It is generally believed that fiber systems of the prefrontal lobes (executive functions, intentions, future planning, etc.) are among the latest to myelinate, a process that may go on into young adulthood. The spinal cord is almost prepared to function at birth. Its weight at that time is 2 to 6g and subsequent gains are less intensive than those of the brain. The growth of the spinal cord runs parallel to the development of motor function – its initial weight triples by the age of 5 years; however, in distinction from brain the structure of the spinal cord approaches adult structure already in the second year of life. The only subsequent increase is in number of motor cells in the ventral (anterior) horns. By puberty the spinal cord increases four to fivefold. The intracranial nerves myelinize by the three month after birth, the peripheral nerves by three years, but growth of the myelin sheath and even of the axis cylinder continues. The autonomic nerves system functions from the moment of birth. So, the morphological features most characteristic of the nervous system in early childhood are immaturity of cerebral cortex, meager differentiation of the nerve cells, and insufficient myelinization of the nerve fibers. Clinical summary The great excitability and tendency to affective states characteristic of very young children are due to prevalent development of the subcortical centers and the decrease of inhibitory activity of the cortex at this age. Development of the sense organs Hearing – the receptive abilities of the auditory analyzers, develops in the child from the time he is two weeks old. Vision – as a reflex to object is defined from the third month of life; transient strabismus and absence of coordinated movement of the eyeballs are physiological phenomena in the newborn. The olfactory sense (smell) develops gradually in the form of reflex to odors after the age of six months, but the perception of taste appears much earlier. Clinical correlates Most defects of the spinal cord result from abnormal closure of the neural folds in the 3rd and 4th weeks of development. The resulting abnormalities are known as neural tube defects (NTDs), which also involve the meninges, vertebrae, muscles, and skin. Spina bifida refers to a splitting of the vertebral arches and may or may not involve underlying neural tissue. The incidence for severe neural tube defects is approximately 1 in 1000 but varies in different populations. refers to a defect in the vertebral arches that is covered by skin and usually does not involve underlying neural tissue. It occurs in the lumbosacral region (L4—S1) and is usually marked by a patch of hair overlying the affected region. The defect is due to a lack of fusion of the vertebral arches and is present in about 10% of otherwise — normal people. Spina bifida cystica can be diagnosed prenatally (!) by ultrasound investigation and by determination of α—fetoprotein (AFP) levels in maternal serum and amniotic fluid. The vertebra can be visualized by 12 weeks of gestation, and defects in closure of the vertebral arches can be detected. Clinical methods of examination of Central Nervous System include interrogation, observation, examination of muscular strength, tonocity, coordination, examination of physiological and pathological reflexes, diagnostic of pathological symptoms and syndromes, examination of child’s mental development, behavior disturbances. The interrogation includes information about complaints, history of the disease, anamnesis of vitae according the schema of the case history. History The history is the most important component of the evaluation of the child with neurology problem. It should carefully document in chronological order the onset of symptoms. A comprehensive review of systems also is essential. It is important to start with concise description of the chief complaint within its developmental context. A comprehensive understanding of developmental milestones is essential in order to ascertain the relative importance of the parents` observations. Following the chief complaint and history of present illness, a review of pregnancy, labor, and delivery is indicated, particularly if a congenital disorder is suspected. Maternal exposure of infections, drugs, cigarettes and alcohol during the pregnancy is important associated with the congenital myophathies and other neuromuscular disorders. The history of birth weight, length and head circumference are particularly important. History Apgar scores, need for ventilator assistance, and history of feeding difficulties should be noted. The most important component of the neurology history is the child`s developmental assessment. An abnormality in development from birth suggests an intrauterine or perinatal cause. A slowing of the rate of acquisition of skills later in infancy or childhood suggests an acquired abnormality of the nervous system. A loss of skills over time strongly suggests an underlying degenerative disease of the central nervous system. The family history is extremely helpful in the neurology evaluation of the child. The history should document the presence of neurologic disease, including epilepsy, migraine, strokes and heredofamilial disorders. It also should be determined whether the parents are related. Observation includes details of head shape, size, posture, locomotion activity, child behavior, muscle bulk, pathological symptoms. Observation of the child behavior and play provides useful information must be modified for infants and children of various ages. The examination should be conducted in a setting that is nonthreatening and enjoyable for the child. The more it seems like a game the greater will be the degree of cooperation. Evaluation of the motor function, gait, and coordination should precede the more threatening head and cranial nerve examination. Paraclinical methods of investigation Include central spinal fluid CSF examination, skull roentgenography, Computer tomography, MRI, cerebral angiography, cranial ultrasound, electroencephalography. “Light- brain” – is a sing of meningitis Focus of necrosis of brain Focus of ischemia of brain Ultrasound investigation – intracranial left-side hemorrhage Computer tomography - intracranial hemorrhage Electroencephalography Differential diagnosis of syndrome of meningism, purulent and serous meningitis Parameters of cerebrospinal fluid The normal data Newborn Color Colorless Transparency Transparent Pressure (mmH2O) 130-180 Frequency of drops from the needle(per minute) 40-60 Cytosis**(10 9/L)-all kinds of cells 0.002-0.008 Leukocytogram: Lymphocytes (%) Neutrophiles (%) Protein (g/L) 80-85 3-5 0.25-0.33 Reaction of pandy*** - Condition after lumbar puncture Head ache, vomiting when a significant quantity is withdrawn The diagnosis Syndrome of meningism Purulent meningitis Serous meningitis Кsantochromic Colorless Milky, greenish Colorless Transparent Transparent Turbid Transparent 150-180 40-60 0,002 – 0,008 80-100 28 0,33-0,35 200-250 Considerably increased 200-300 60-80 Frequency lesser then normal* 60-90 0.002-0.008 1.0-15.0 0.02-1.0 80-85 3-5 0-60 40-100 80-100 0-20 0.16-0.45 0.66-16.0 0.33-1.0 +++,+++ +,++ Insignificant improvement for a short period of time Significant relief often becomes the turning point of the disease + Significant relief often becomes the turning point of the disease The main clinical symptoms of nervous system diseases are headache, dizzines, disorder of motor function (apraxia, ataxia, hyperkinesiscramp, tremor, changes of muscular tonus, gait, paralysis, disorders of consciousness, speech, reflexes activity, sleep, cranial nerves, sensitivity and other). Syndrome of movement and reflex disorders (upset) includes paralysis and paresis. Paralysis is inability of motor activity, Paresis is partial loss of motor activity. Congenital anomaly of development inflammatory diseases, affection of neural system due to - infections, - metabolic disorders, - toxicosis. The symptoms of neurological disorders of different diseases can be apathy, somnolence, unconsciousness, excitation, convulsions, defects of speech, defects of hearing, defects of reading or writing, extremely large head in hydrocephaly the small dimensions of cranial in microcephaly paralysis of facial nerve, paralysis of peripheral nerve, disturbance of coordination, motor ataxia, increased muscular tonicity, decreased muscular tonicity, pathologic reflexes. Congenital hydrocephaly According to spreading it is possible to distinguish monoplegia, hemiplegia, paraplegia, tetraplegia. According to focus of movement neurone (effector neurone) affection it is possible to make out - central (spastic) paralysis due to affection of central neurone - and peripheral (flaccid) paralysis due to affection of peripheral neurone. Central (spastic) paralysis is characterised by increase of muscular tonus, increase of deep tender reflexes, pathologic reflexes (Babinsky’s reflex, Rossolimo’s reflex). muscles tropism is not affected, atrophy is not present. Peripheral (flaccid) paralysis is characterised muscle hypotonia, decrease or absence of reflexes, extremities grew colder, trophic disorder, decrease of bones growth are marked. Most often reasons of paralysis and paresis are pathology of perinatal period, polyomielitis, metabolopathy. Central paralysises are result of acute and chronic affections of brain as in intrauterus period, so in delivery, if brain is affected by asphyxia or trauma, hypoglycemia, hyperbilitubinemia. Convulsive syndrome (seizures) Types of convulsions are various: Clonic convulsions: tonic convulsions – with affection of extenzors, flexors, mixed type, unifocal, multifocal, hemiconvalsions, focal tonic –asymmetrial truncal or eye deviation, generalized tonic activity. myoclonic (generalized or focal); motor automatism (rhythmic rapid or random eye movements, pedaling, rotatory arm movements, purposeless movements). Causes of seizures are various: epilepsy, toxicosis infections of CNS – meningitis, meningoencephalitis, infection diseases – dysentery, pneumonia, gastroenteritis and many other. Syndromes of sensitivity disturbances. Sensitivity can be increased, is called hyperesthesia, hypersensitivity. decreased is called hypoesthesia. changed due to different diseases (meningitis, tumor of brain) is called paresthesia Meningeal syndrome occurs in all forms of acute meningitis Symptoms of meningeal syndrome include all typical brain affection symptoms and local symptoms. Most typical symptoms are fever, headache, vomiting, dizziness, muscle tonic strain, neck muscle regidity, Kernig’s, Brudzinsky’s symptoms are positive, Lesage’s symptom is positive, convulsions, sensitivity disturbances (hyperesthesia), vegetative disturbances (arrhythmia, pulse and breath dissociation), disturbances of breath rhythm, vasomotor lability, psychiatric disturbances (dullness, adynamia, hallucinations, hypomnesia). Bulging fontanella, motor unrestless, convulsions, tremor of extremitis, dullness, unconscionsness, change of CFS (protein increase, leucocities increase, increased pressure) are typical for newborn suffering from meningitis. Encephalitic syndrome includes some complexes of symptoms general symptoms of infections (fever, hemogramme changes, increased ESR), symptoms of general brain disturbances due to oedema and hyperaemia of brain, hyperproduction of liquor, disturbances of consciousness, excitement convulsions, meningeal symptoms, cells-protein dissociation in CSF. Encephalitic reaction occurs in acute infections (convulsive syndrome, delirium). Syndrome of consciousness disturbances includes excitement with euphoric, excitement with negativism, somnolence, stupor, sopor, coma (I, II, III degree). Cause of consciousness disturbances are infections, metabolic disorders, diabetes melitus. Syndrome of sleep disturbances includes superficial sleep, insomnia, sleep walking (somnambulism), sleeptolking, swing and knocking. Syndromes of CNS disturbances in newborn and infant includes syndromes of hypoexcitability, hyperexcitability, motor disturbances, muscle hypotonia, muscle dystonia, muscle hypertonia, cerebellum motor disturbances, hypertention – hydrocephalic syndrome, convulsive syndrome, syndrome vegetative-visceral disturbances, syndrome of minimal brain dysfunction. Neurosis in children includes stammering, hysteria, noctural incontinence of urine (enuresis), tics, cramp, neurasthenia. Care of children with nervous system disorder Some pathological syndromes are accompanied disorders of vital functions (breathing, cardiovascular activity) and demand intensive care. Intensive care includes: comfortable condition because neural regulation of vegetative functions is not perfect if the child is suffering from serious neurological disorders. Incubator is advisable for newborn (temperature regime, humidity, oxygen supply). Monitoring of vital functions has to be done. Fluid and electrolytes balance control. Monitoring of IV fluid therapy is advisible. Nutrition has parenteral feeding if it is necessary. Care of children with nervous system disorder