Fluid Therapy in the Neonatal Period
advertisement

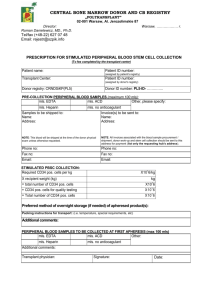
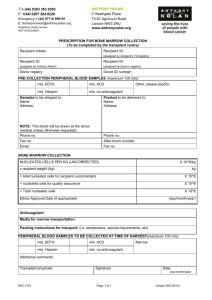
Pedram Niknafs, MD Professor of Pediatrics Director of Neonatal Services Afzalipour Medical School Kerman University of Medical Sciences Kerman, Iran Transition to Extrauterine Life • Redistribution of body water • Changes in renal function - renal blood flow and GFR - sodium balance - water handling • The kidney of a premature infant is unable to maintain positive water and sodium balance without large intakes of fluid and electrolytes. • Growth • Increased IWL • Immature renal function The Reasons for IWL in Preterm Infants • Immaturity of the cornified layer of the skin • Body surface/body mass The Relationship Between Metabolism and Maintenance Fluids Route mL/100 kcal metabolized energy • Insensible 40 - Skin 25 - Respiration 15 • Urine 80 • Stool 5 Total for Maintenance 125 Clinical Criteria to Assess Hydration • Body weight (weight loss of 5% to 15% in term and VLBW infants respectively) • Skin turgor • Edema • Fontanelle • Oral mucus membranes Laboratory Criteria to Assess Hydration • Urine volume (1-3 mL/kg/h) • Serum sodium • Urine osmolality (150-400 mOsm/L) • Urine specific gravity (1006-1013) A Practical Method to Calculate Fluid Requirements (mL/kg/d) Day 1 2 3 < 1000 100 120 140 1000-1500 80 100 120 > 1500 60 80 100 Adjustments depend on clinical and biochemical assessment of hydration state. Usually 120-150 mL/kg/d is adequate to maintain hydration during the first two weeks. Fluid Therapy in the Neonatal Period (mL/kg/d) Maintenance phototherapy Renal concentrating defect Acute renal failure Mechanical ventilation Congestive heart failure Total Depending on age and WT + 20 - 60 + urine volume - 70 + urine volume - 10 - 30 ............ Factors That Dramatically Change the Fluid Requirements • Critically ill newborn infants • Environmental stresses: - radiant warmer - phototherapy • Immature organ function • Transition to extrauterine life 1. Severe prematurity, 100-300% 2. Open warmer bed, 50-100% 3. Forced convection, 30-50% 4. Phototherapy, 30-50% 5. Hyperthermia, 30-50% 6. Tachypnea, 20-30% 1. Humidification in incubator, 50-100% 2. Plastic heat shield in incubator, 30-50% 3. Plastic blanket under radiant warmer, 30-50% 4. Tracheal intubation with humidification, 20-30% • Urine output <0.5 mL/kg/h • Serum sodium 150 mEq/L • Body weight loss approaches 15% of birthweight • Baby is appearing dehydrated (color, perfusion, turgor, anterior fontanelle) • • • • Urine output >4 mL/kg/h Serum sodium <130 mEq/L Body gain in the first 3 days of life Body is edematous with otherwise adequate hemodynamics (color, perfusion, heart rate, and blood pressure) •Na: 2 mEq/kg/day •K: 2 mEq/kg/day •Cl: 4 mEq/kg/day • Initial Therapy • Maintenance with restriction • Liberalization of fluids Stabilization • Establish IV access • Treat shock • Prevent hypoglycemia Maintenance with Restriction • Least volume to prevent dehydration Liberalization • Rehydration • Advance nutrition for growth Complications of Excessive Fluid Intake • • • • Bronchopulmonary dysplasia Patent ductus arteriosus Necrotizing enterocolitis Intraventricular hemorrhage BPD PDA NEC IVH Calculation of Na Deficit Serum Na Concentration (mEq/L) Calculation of Total Solute Deficit (mOsm/kg) Solute Deficit (mOsm/kg) Na Deficit (mEq/kg) Isotonic (10%) 140 (0.7 x 280) – (0.6 x 280) 28 14 Hypertonic (10%) 153 (0.7 x 280) – (0.6 x 306) 12 6 Hypotonic (10%) 127 (0.7 x 280) – (0.6 x 254) 44 22 Type of Dehydration Avery's: Neonatology, 6th edition, 2005: 793 Total solute deficit is assumed to be half Na. Although the serum (and ECW) has lost this amount of Na, only half this amount has been lost in the environment; the other half has been lost into the cells in exchange for K, which in turn has been lost from the body. In practice, therefore, only half the amount listed as “Na deficit” should be replaced as Na, and the other half should be given as K. Avery's: Neonatology, 6th edition, 2005: 793 Hypernatremia: Therapy • Increase free water administration to reduce serum Na no faster than 1 mEq/kg/h. • Hypernatremia does not necessarily imply excess total body Na. For example, in the VLBW infants, hypernatremia in the first 24 hours of life is almost always due to free water deficits. Cloherty JP, et al: Manual of neonatal care, 2012: 275 Physician’s Order FLUIDS mls/kg/day …………… mls/day …………… mls/hour …………… Physician’s Order ARTERIAL LINE: 500 mls D5W/Normal saline Additives: 500 units Heparin Rate of infusion: 1 ml/hour Physician’s Order IV 1: D5W/D10W/Protein solutions Additives to ……………. mls KCl ………. % ………. mls (K= 2 mEq/kg/d) NaCl ………. % ………. mls (Na= 3 mEq/kg/d) Ca gluconate 10% ………. mls Rate of infusion …………… mls/hour Physician’s Order IV 2: Type: Intralipid 20% …… mls Additives to ………….. mls Rate of infusion ………….. mls/hour Physician’s Order IV 3: Type: Additives to …………… mls ……………………………………… ……………………………………… Rate of infusion ……………. mls/h Physician’s Order ORAL FLUID INTAKE: EBM 4 mls 2/24 by 2 mls every 2nd feed IV accordingly