Respiratory
advertisement

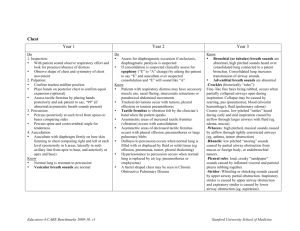
Respiratory Exam Tip; From the outset of your exam, esp general inspection, start considering the unifying diagnosis. Your findings must be coherent & make sense. (eg. If in resp distress, expect findings for the rest of exam – eg wheeze/ crackles on auscultation; if inhalers by the bed – make sure you don’t miss signs such as barrel chest or harrison’s sulcus, hyper-resonance, wheeze etc.; if chest drain in situ, don’t miss stony dullness; if IV antibiotics hanging, be vigilant about picking up ↓ air entry / crackles etc.) The patient may not have these text-book signs & may have indeed normal findings, but let the clues you gather early in the exam aid your precision for the rest of it. As best as possible, have your findings consistent with each other. O/E; 1) Inspection i) General (while washing hands & ask expose chest) C H A N D L E R Listen for sounds audible from end of bed Infant; Ask mum to expose child’s chest & abdomen Leave infant in mum’s arms Older child; expose child to waist (except adolescent girl) ii) Signs of respiratory distress; Tachypnoea Dysponea (?difficulty speaking) Recession (supraclavic, inter- & sub-costal) Tracheal tug Nasal Flaring Accessory muscles, Abdominal breathing Grunting Resp-specific Hands – clubbing, (stages? causes?), anaemia, BCG scar Pulse Head & Neck – cyanosis (under tongue) tracheal tug Coryza/secretions, Petechiae (from coughing) Defer further ENT until the end. iii) Tip; Take advantage of whatever position the child is in – eg. If infant happy clinging to mum while back exposed, examine the back first – but say you’re doing this to the examiner. You can decide to examine anteriorly first & then move to the back, or if child sitting up you can inspect front & back, palpate front & back, & so on if it suits. Again, let the examiner know what you’re doing, & take charge! Chest Resp rate; count for 10 secs & multiply x6 *abdominal breathers until 3-4 years* nb. any signs of Resp Distress Shape; Pectus carinatum / excavatum harrison’s sulcus hyperinflation (barrel chest) Symmetry & Movement; compare sides Scars Axilla – inspect ? drains / scars / swellings Spine; scoliosis (formal test later if indicated) CO2 retention; v rare Paeds Signs are; Sweaty/clammy hands Tremor/asterixis Dialated veins (bk hand) Bounding pulse ± papilloedema Scars & surgery; Thoracotomy; lobectomy Left; CoA, BT shunt Right; BT, Oesophageal Sternotomy; usually cardiac Chest drains; site; 5th i/c space mid-ax. line 2) Palpation – Neck; Lymph nodes, (best done from behind) ↑ VF; consolidation neck swellings ↓ VF; pneumothorax, tracheal deviation, th th effusion, collapse Apex beat – MCL 5 intercostal space (4 in < 3 yrs) Chest expansion [if > 4-5 years; normally 3-5 cm] Vocal fremitus [not useful < 3-4 yrs]; place one hand each side & ‘say “99”’; vibratory sensation +/- liver palpation if hyperinflation/wheeze, esp in infant! (do at the end) 3) Percussion – Not very useful < 3yrs, but know how to do it explain to the child, “play knock knock / like a drum” start at clavicle – to guage normal sound- get used to sounds side to side to compare sides include axillae ↑ resonance; hyperinfln pneumothorax ↓ resonance; collapse, consol., organs, effusion; stony dull 4) Auscultation Bell of stethoscope – warm it up first 6 positions front & back, compare sides (+ supraclavicular/apex in older child ie. 8) don’t forget axilla full inspiration & expiration at each site Comment on; Air Entry; ?equal bilateral or reduced? Breathing type; Vesicular vs. bronchial ie. Listen insp/exp phases? duration of each? gap? Any extra sounds; Creps / wheeze, +/- other; eg. pleural rub Vocal Fremitus – (not necessary if tactile vocal fremitus done) Say “99” – listen in same areas as for regular auscultation Sounds louder over areas of consolidaton REPEAT AT THE BACK NOW;(sit child forward) Inspect – scars, scoliosis Palpate – expansion, tactile vocal fremitus Percuss – (as above) – [ask child to stretch arms in front to expose under scapula] Auscultate – (as above) 5) At end; a. ENT (offer to do this, but only at end; upsetting for young children) b. PEFR (over 6 years) c. Examine sputum Breath sounds; Reduced/absent; collapse / effusion / pneumothorax / obstruction (ie. ↑ gap between lung & chest wall/ you listening, so can’t hear as much) Vesicular breathing; (normal) insp:exp 3:1, no gap, exp. fades Bronchial breathing; insp & exp same duration, no pause between, doesn’t fade (listen over your trachea) Patent bronchi but alveoli full/blocked ; ie. Consolidation / fibrosis Prolonged expiration; (often with wheeze); obstructive disease eg, asthma Wheeze (exp) = Rhonci; Asthma / bronchiolitis / viral induced / foreign body (high-pitched, due to partial obstruction of bronchioles) [can occur in inspiration (stridor) if obstruction severe] Creps/crackles; consolidation / fibrosis Fine (ie more high-pitched – indicate alveoli > bronchioles) Coarse (ie variable pitch - indicate bronchioles > alveoli) Transmitted sounds; from upper airways Exercise 1 – go over the above exam structure & select out the parts of it that are relevant to the examination of the infant. Exercise 2 – consider what pattern of clinical findings you’d expect to find in the following conditions; Auscultation Condition Consolidation Collapse Effusion Pneumothorax Obstructive dx (asthma) Chronic dx CF Foreign body Inspection Movement Mediastin al shift Percussion Vocal resonance Air Entry . extra Breathing sounds