07 Anatomo-physiological peculiarities of the respiratory system
advertisement

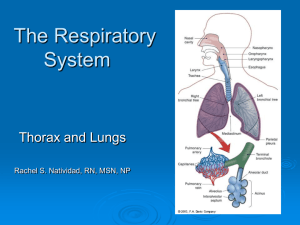
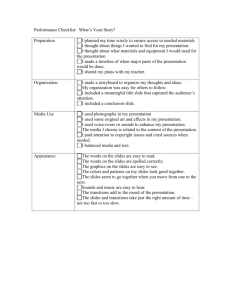
Anatomy & Physiology of the respiratory system in children prof. Pavlyshyn H.A., MD, PhD Respiratory system • The respiratory system is divided into two parts: upper and lower respiratory tract; • The border of this division is the lower edge of the cricoid cartilage. • Upper respiratory tract includes the paranasal sinuses, nasal cavity, pharynx and the Eustachian tube and other parts; • Lower respiratory tract includes the trachea, bronchi, bronchial and alveolar capillary. Anatomical characteristics Upper respiratory tract • The nose, nasal passages (airways), sinuses infancy are comperatively narrow + Mucosa is rich for vascular tissue } that makes child vulnerable to infection and oedema; → • Infection, swelling of the nasal cavity and nasal congestion contribute more narrow or blocked of nasal airways, causing difficulty in breathing and sucking. • There are not inferior (lower) nasal passages (until 4 years) and as a result rarely epistaxis in infants; • Nasolacrimal duct is short, the opening valve, hypoplasia valve may be the cause of conjunctivitis with upper respiratory tract infection • Development sinuses of infants continued after 2 years of age and finished to 12 years; the maxillary sinuses is usually present at birth; the frontal sinuses begin to develop in early infancy; Babies can suffer from sinusitis; the ethmoid, maxillary sinuses are most vulnerable to infection. Upper respiratory tract in children • Larynx is located on level the 3-4th (neck) vertebrae; •Vocal and mucous membranes are rich blood vessels and lymphatic tissue, prone to inflammation, swelling, due to babies suffering from laryngitis (viral croup), airway obstruction, inspiratory dyspnea; Anatomical characteristics Lower respiratory tract • The trachea is short; • Tracheal and bronchial passes in Trachea children is relatively small, cartilage soft, the lack of elastic tissue LRT – vulnerable, easy to cause airway narrowing and obstruction Bronchi Tubes Right bronchus more straight, like a direct extension of the trachea (causing the right lung atelectasis or emphysema); Left bronchus is the separation from the trachea; The bronchus is divided into inter-lobe bronchus, segmental bronchus, bronchioles. Bronchioles - no cartilage, smooth Bronchiole muscle imperfect development, mucosa rich in blood vessels, mucous glands hypoplasia, lack of secretion of mucus, Alveoli poor mucociliary movement; Anatomy and physiology • The ribs are cartilaginous and perpendicular relative to the vertebral column (horizontal position), reducing the movements of the rib cage. • The infant chest wall is remarkably compliant and compliance decreases with increasing age. – The orientation of the ribs is horizontal in the infant; by 10 years of age, the orientation is downward. The mecanizm of breathing • Contraction of Contraction of external diaphragm: intercostal diaphragm moves muscles > downward elevation of ribs & >increases vertical sternum dimension of • > increased frontthoracic cavity to-back dimension of thoracic cavity ↓ ↓ lowers air pressure in lungs air moves into lungs Anatomy and physiology • The intercostal muscles and accessory muscles of ventilation are immature. As a result, children are more reliant on the diaphragm for inspiration. • Increased respiratory effort causes subcostal and sternal recession, and the mechanical efficiency of the chest wall is reduced. Summary The considerable differences in respiratory physiology between infants and adults explain why infants and young children have a higher susceptibility to more severe manifestations of respiratory diseases, and why respiratory failure is common problem in neonatal and pediatric intensive care units. The appreciation of the peculiarities of pediatric respiratory physiology is not only essential for correct assessment of any ill child, but also for correct interpretation of any pulmonary function test performed in this population. An average respiratory rate at rest of the child of different age is: • newborn 40-60 per minute, • infant at 6 months 35-30 per minute, • at 1 year 30 per minute, • 5 years 25 per minute, • 10 years 20 per minute, • 12-18 years 16-20 per minute. Percussion • Resonant sounds are low pitched, hollow sounds heard over normal lung tissue. • Flat or extremely dull sounds are normally heard over solid areas such as bones. Percussion • Percuss the lung fields, alternating, from top to bottom and comparing sides • Percuss over the intercostals space. • Keep the middle finger firmly over the chest wall along intercostals space and tap chest over distal interphalangeal joint with middle finger of the opposite hand. • The movement of tapping should come from the wrist. • Tap 2-3 times in a row. Percussion Percuss the chest all around. Stand back, have the patient cross arms to shoulder. This maneuver will wing the scapula and expose the posterior thorax. Then, have the patient keep their hands over head and percuss axilla. • Then move to the front and percuss anterior chest , clavicles and supraclavicular space. Percussion • The lung is filled with air (99% of lung is air). • Percussion of it gives a resonance. This step helps identify areas of lung devoid of air. •Appreciate the dullness of the left anterior chest due to heart and right lower chest due to liver. • Note the hyper-resonance of the left lower anterior chest due to air filled stomach. • Normally, the rest of the lung fields are resonant. The pathological dullness is heard in cause of • Dull or thud like sounds are normally heard over dense areas such as the heart or liver. • Dullness replaces resonance when fluid or solid tissue replaces air-containing lung tissues, such as occurs with pneumonia, pleural effusions (hydro-, haemothorax), or tumors. • Decreased resonance is noted with pleural effusion and all other lung diseases. The hyper resonant sounds is heard in cause of Increased resonances can be noted either due to lung distention as seen in asthma, emphysema or due to Pneumothorax. • Hyper resonant sounds that are louder and lower pitched than resonant sounds are normally heard when percussing the chests of children and very thin adults. • Hyper resonant (ban-box) sounds may also be heard when percussing lungs hyperinflated with air, such as emphysema of lungs, patients with COPD, asthma, asthmatic bronchitis. • An area of hyper resonance on one side of the chest may indicate a pneumothorax. Anatomy of lobes of lungs Auscultation method of exam • Auscultate the lungs from the apices, middle and lower lung fields posteriorly, laterally and anteriorly. • Alternate and compare sides. • Listen to at least one complete respiratory cycle at each site. • First listen with quiet respiration. If breath sounds are inaudible, then have him take deep breaths. • First describe the breath sounds and then the adventitious sounds. Auscultation method of exam • Note the intensity of breath sounds and make a comparison with the opposite side. • Assess length of inspiration and expiration. Listen for the pause between inspiration, expiration. • Compare the intensity of breath sounds between upper and lower chest in upright position. • Note the presence or absence of adventitious sounds. Begin by auscultation the apices of the lungs, moving from side to side and comparing as you approach the bases. If you hear a suspicious breath sound, listen to a few other nearby locations and try to delineate its extent and character. • To assess the posterior chest, ask the patient to keep both arms crossed in front of his/her chest, if possible. • It is important that you always compare what you hear with the opposite side. Normal breath sounds • tracheal, bronchial, broncho-vesicular and vesicular sounds. Breath sounds are described by: • duration (how long the sound lasts), • intensity (how loud the sound is), • pitch (how high or low the sound is), and • timing (when the sound occurs in the respiratory cycle). Breath sounds can be divided into the following categories: Normal Abnormal Adventitious tracheal absent/decreased crackles (rales) vesicular bronchial wheeze bronchial rhonchi bronchovesicular stridor pleural rub mediastinal crunch (Hamman's sign) Normal breath sounds • Bronchial sounds are present over the large airways in the anterior chest near the second and third intercostal spaces (trachea, right sternoclavicular joints and posterior right interscapular space); • These sounds are more tubular and hollow-sounding than vesicular sounds, but not as harsh as tracheal breath sounds. • Bronchial sounds are loud and high in pitch with a short pause between inspiration and expiration (inspiration and expiration are equal); expiratory sounds last longer than inspiratory sounds. The Bronchial Breath Sound has the following characteristics : • An I:E Ratio : 1:1 or 1:1 1/4 with a pause in between inspiration & expiration • Thoracic Geography : over the manubrium of the sternum • Sound Characteristics : high pitched, tubular, hollow sound • Indication: that an area of consolidation exists pneumonia, atelectasis, fluid infiltration The Bronchovesicular Breath Sound has the following characteristics : • An I:E Ratio : 1:1 or 1:1 1/4 with a pause in between inspiration & expiration • Thoracic Geography : They are best heard in the 1st and 2nd ICS (anterior chest) and between the scapulae (posterior chest) - over the main stem bronchi • Sound Characteristics : high pitched, tubular, hollow sound • Indication : an area of consolidation - pneumonia, atelectasis, fluid infiltration Summery Type Characteristic Intensity Pitch tracheal loud high vesicular Soft low bronchial very loud high Description harsh; not routinely auscultated over the trachea . most of the lungs over the manubrium sound close to stethoscope; gap (normal) or between insp & exp sounds consolidated areas medium . normally in 1st & 2nd ICS anteriorly and between scapulae posteriorly; other locations indicate consolidation . . Normal bronchovesicular Abnormal Medium Location absent/decreased . . heard in ARDS, asthma, ateletasis, emphysema, pleural effusion, pneumothorax bronchial . . indicates areas of consolidation The term “adventitious” breath sounds • refers to extra or additional sounds that are heard over normal breath sounds. • • • • crackles (or rales) wheezes (or rhonchi) pleural friction rubs stridor Adventitious sounds • Wheeze • Stridor • Crackles • Pleural Rub Crackles (or rales) • Crackles are discontinuous, intermittent, nonmusical, brief, "popping" sounds that originate within the airways. • are caused by fluid in the small airways or atelectasis. • Crackles may be heard on inspiration or expiration. The popping sounds produced are created when air is forced through respiratory passages that are narrowed by fluid, mucus or pus. • Crackles are often associated with inflammation or infection of the small bronchi, bronchioles and alveoli (pneumonia, atelectatic lung). • Crackles are often described as fine (high pitched, soft, very brief), coarse (low pitched, louder, less brief). • Fine crackles are soft, high-pitched, and very brief. You can simulate this sound by rolling a strand of hair between your fingers near your ear. • Coarse crackles are intermittent "bubbling" sound somewhat louder, lower in pitch, and last longer than fine crackles. Wheeze Lung Sounds • These are continuous, high pitched, hissing, whistling or sibilant sounds. • They are caused by air moving through airways narrowed by constriction or swelling of airway or partial airway obstruction (asthma, CHF, chronic bronchitis, COPD). • Wheezes are sounds that are heard continuously during inspiration or expiration, or during both inspiration and expiration. • Wheezes that are relatively high pitched and have a shrill or squeaking quality may be referred to as sibilant rhonchi. These wheezes occur when airways are narrowed, such as may occur during an acute asthmatic attack. • Wheezes that are lower-pitched sounds with a snoring or moaning quality may be referred to as sonorous rhonchi. Secretions in large airways, such as occurs with bronchitis, may produce these sounds; Pleural friction rubs • are low-pitched, grating, or creaking sounds that occur when inflamed pleural surfaces rub together during respiration. • More often heard on inspiration than expiration, the pleural friction rub is easy to confuse with a pericardial friction rub. • To determine whether the sound is a pleural friction rub or a pericardial friction rub, ask the patient to hold his breath briefly. If the rubbing sound continues, its a pericardial friction rub because the inflamed pericardial layers continue rubbing together with each heart beat - a pleural rub stops when breathing stops. Summery Type Characteristic Intensity soft (fine crackles) or crackles (rales) loud (coarse crackles) Adventitio us Pitch high (fine crackles ) or low (coarse crackles) wheeze high expiratory rhonchi low expiratory stridor . inspiratory pleural rub . insp. & exp. . not synchronized w/ respiration mediastinal crunch Description Location discontinuous, nonmusical, brief; may sometimes be more commonly heard on normally heard at ant. inspiration; assoc. w/ ARDS, asthma, lung bases after max. bronchiectasis, bronchitis, expiration or after consolidation, early CHF, interstitial prolonged lung disease recumbency continuous sounds normally heard on expiration; note if monophonic can be anywhere over (obstruction of 1 airway) or the lungs; produced polyphonic (general obstruction); when there is assoc. w/ asthma, CHF, chronic obstruction bronchitis, COPD, pulm. edema continuous musical sounds similar to wheezes; imply obstruction of larger . airways by secretions musical wheeze that suggests heard loudest over obstructed trachea or larynx; trachea in inspiration medical emergency creaking or brushing sounds; usually can be continuous or discontinuous; assoc. localized to particular w/ pleural effusion or pneumothorax place on chest wall crackles synchronized w/ heart beat; best heard w/ patient medical emerg.; assoc. w/ in left lateral pneumomediatstinum decubitus position