Postpartum Hemorrhage
advertisement

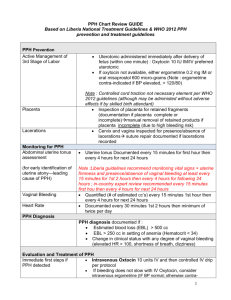
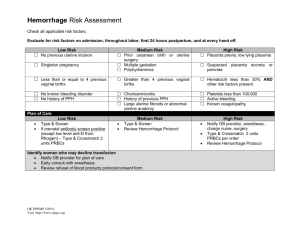
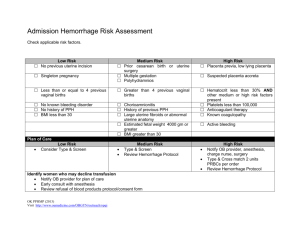
Postpartum Hemorrhage (PPH) Family Medicine Specialist CME University of Health Sciences Clinical Case 25 year-old G7P2 female presents for delivery, which occurs very rapidly after arriving at the District Hospital. Her baby was delivered without difficulty but then the placenta was retained and she began to hemorrhage. What is your definition of a postpartum hemorrhage? What are the risk factors this patient has for a postpartum hemorrhage? What are you going to do to manage this patient? Objectives • Define postpartum hemorrhage (PPH) • Discuss the risk factors and possible causes for PPH • Describe the preventative measures to take to prevent a PPH • Discuss the management of PPH • Explain the risks to maternal morbidity and mortality of PPH Definitions • Primary/immediate PPH – Excessive bleeding during the 24 hours after a delivery – Most often due to uterine atony • Secondary/late PPH – Excessive bleeding between 24 hours and up to 6 weeks after delivery – Most often due to retain products of conception, infection or both What is excessive bleeding or a PPH? • Vaginal delivery – >500 cc of blood loss • Cesarean section – >1000 cc of blood loss • Clinically – Any blood loss that causes the patient to be hemodynamically unstable Hypovolemia Clinical Presentation Mild (<20% of blood volume) • • • • Moderate (20–40% of blood volume) •Heart rate - >110 bpm Heart rate - mild tachycardia •Tachycardia - >30 rpm Skin – mottled, cool •BP – Normal in supine extremities due to position/significant increased systemic vascular resistance postural hypotension and prolonged •Skin - marked pallor; capillary refilling conjuntiva, palms and Urinary output mucous decreased Neurologic status – •Neurologic status – may report dizziness increasingly anxious but usually remains normal Severe (>40% of blood volume) • Heart rate marked tachycardia • BP – declines/unstable even in supine position • oliguria or anuria • Neurologic status – agitation, confusion, possible loss of consciousness Estimating blood loss • Usually underestimated • Ongoing trickling can cause significant blood loss • Underestimation can lead to delayed or inadequate treatment • If patient is anemic, then the ability to compensate for blood loss may not be possible and patient cannot tolerate any blood loss PPH Etiology • Tone – uterine atony • Tissue – retained placenta • Trauma – vaginal/cervical lacerations, rupture, inversion of uterus • Thrombin - coagulopathy Tone: Risk Factors Etiologic process Clinical risk factors Overdistended uterus Polyhydramnios Multiple gestation Macrosomia Uterine muscle exhaustion Rapid labour Prolonged labour High parity Intraamniotic infection Fever Prolonged rupture of membranes (PROM) Tone – Risk Factors (2) Etiologic process Clinical risk factors Functional or anatomic distortion of the uterus Fibroid uterus Placenta previa or abruptio Uterine anomalies Uterine-relaxing medications Halogenated anesthetics nitroglycerin, magnesium sulphate Tissue – Risk Factors Retained Placental tissue Etiologic process Retained products, abnormal placentation, retained cotyledon or succinuriate lobe Clinical risk factors Incomplete delivery of placenta Previous uterine surgery High Parity Abnormal placenta on ultrasound Retained blood clots Atonic uterus Trauma (Genital Tract) – Risk Factors Etiologic process Clinical risk factors Tears (lacerations) of the cervix, vagina, or perineum Ruptured vulvar varicosities Precipitous delivery Operative delivery Mistimed or inappropriate use of episiotomy Extensions, lacerations at cesarean section Malposition Deep engagement Uterine rupture Previous uterine surgery Uterine inversion High parity Fundal placenta Thrombin (Abnormalities of Coagulation) – Risk Factors Etiologic process Clinical risk factors Pre-existing states History of hereditary coagulopathies History of liver disease Therapeutic anticoagulation History of thrombotic disease Thrombin (Abnormalities of Coagulation) – Risk Factors (2) Etiologic process States acquired in pregnancy • idiopathic thrombocytopenic purpura • thrombocytopenia with preeclampsia • disseminated intravascular coagulation • preeclampsia • dead fetus in utero • severe infection/sepsis • placental abruption • amniotic fluid embolus Clinical risk factors bruising elevated blood pressure fetal demise fever elevated white blood cells antepartum hemorrhage sudden collapse Prevention of PPH – Active Management of the Third Stage of Labor • prophylactic administration of oxytocin with delivery of anterior shoulder or immediately after delivery – 10 U IM OR 5 U IV bolus • clamp and cut cord after pulsating has stopped • palpate the uterine fundus and confirm the uterus is contracted • perform controlled cord traction with suprapubic counter traction with next strong contraction • perform uterine massage after delivery of the placenta, as appropriate • examine placenta for completeness Controlled cord Traction Uterotonics - Oxytocin • stimulates smooth muscle tissue of the upper segment of the uterus causing it to contract rhythmically, constricting blood vessels, and decreasing blood • safe and effective first choice for prevention and treatment • acts almost immediately for IV injections, and within 3 to 5 minutes for IM injections • should be stored in a cool, dry place • uncommon side effects: nausea, vomiting, and headache Uterotonics – Ergot Alkaloids “Ergometrine” • causes the smooth muscle of both the upper and lower uterus to contract tetanically • takes 5 to 7 minutes to take effect when given intramuscularly • effects last approximately 2 to 4 hours • should be stored in a refrigerator between 2°C – 8°C and away from light • adverse effects include nausea and vomiting Uterotonics – Prostaglandins “Misoprostol” • causes vasoconstriction and enhances contractibility of the uterine muscles • administered orally or sublingually (rapid action), or rectally (acts fir greater period of time) for prevention or treatment of PPH • relatively inexpensive, easy to store, stable at room temperature • side effects: shivering and fever are generally mild Management of Postpartum Hemorrhage • Prevention is the key! 1. Identify and manage risk factors identified for potential PPH 2. Active management of the third stage of labor Management of Postpartum Hemorrhage 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Active management of the Third Stage of Labor REMEMBER the ABCs Call for HELP Estimate blood loss. Ask the woman to urinate or catheterize Put the baby to the breast Give Oxygen Assess the uterus using external or internal bimanual massage Give uterotonic - Oxytocin, Misoprostol, ergotamine Observe the woman, and consider transport if unstable or bleeding continues Management of PPH A B C = airway = breathing = circulation External Bimanual Uterine Massage Internal Bimanual Uterine Massage Examine the placenta for completeness Examination of maternal side Examination of fetal side Manual removal of placenta 1. 3. 2. 4. Management of Postpartum Hemorrhage 11.Examine the genitals for trauma and repair as required ie. vulva, vagina, cervix 12. If bleeding continues may require uterine tamponade or aortic compression 13.Ensure no uterine inversion or rupture 14.Manage possible coagulopathy with blood transfusion (if possible) 15.Consider transfer to facility for surgical management of PPH Aortic Compression Uterine Tamponade Management of secondary PPH Associated with: – retained placental fragments or membranes – infection – shedding of dead tissue following an obstructed labour – breakdown of a uterine wound after a cesarean section or ruptured uterus Management of secondary PPH (2) • • • • assess the woman’s condition carefully control blood loss treat for shock, if necessary administer antibiotics prophylactically for infection • provide anti-tetanus prophylaxis, if necessary • if there is no improvement with the above treatments, refer the woman promptly for further assessment and treatment Continued care of woman Once the bleeding is controlled, and the woman is stable, careful monitoring over the next 24–48 hours is required, including: • monitoring uterine tone • monitoring vital signs • estimating ongoing blood loss • ensuring adequate fluid intake • monitoring blood transfusions • monitoring urinary output • ensuring the continuous presence of a skilled attendant, who maintains good documentation Before discharge from hospital • check hemoglobin, and provide supplements as required • examine for hookworm infestation, malaria, HIV/AIDS or other co-existing conditions, provide treatment as required • provide the mother and her family with information about her experience of PPH • ensure that lactation has been established, and that a well baby care plan is in place Conclusion • Assess patient for PPH risk factors and manage accordingly • Prevention is the key: Active management of the third stage of labor • Management of bleeding is essential for saving a woman’s life • Refer to center as required for advanced care