Disordered Eating
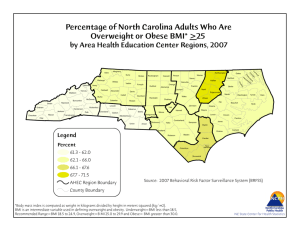
advertisement

Jack Sprat and His Wife: Disordered Eating and the Continuum From Anorexia Through Obesity Stephen Sondike, MD Medical Director, Disordered Eating Center Of Charleston (DECC) Section Head, Adolescent Medicine Charleston Area Medical Center Associate Professor of Pediatrics West Virginia University School of Medicine Jack Sprat could eat no fat. His wife could eat no lean. And so between them both, you see, They licked the platter clean Anorexia Nervosa Anorexia Nervosa Female athlete Triad Anorexia Nervosa Female athlete Triad EDNOS Anorexia Nervosa Female athlete Triad EDNOS Bulimia Nervosa Anorexia Nervosa Female athlete Triad “non-purging” BN EDNOS Bulimia Nervosa Anorexia Nervosa Binge eating disorder “non-purging” BN Female athlete Triad EDNOS Bulimia Nervosa Anorexia Nervosa overweight Binge eating disorder “non-purging” BN Female athlete Triad EDNOS Bulimia Nervosa Anorexia Nervosa overweight Binge eating disorder “non-purging” BN Female athlete Triad EDNOS Bulimia Nervosa A case in point: Pt RS Anorexia Nervosa overweight Female athlete Triad Binge eating disorder EDNOS “non-purging” BN Bulimia Nervosa Age 11: 160 lbs (pt report) Anorexia Nervosa overweight Female athlete Triad Binge eating disorder EDNOS “non-purging” BN Bulimia Nervosa Age 13: (3/3/09) Wt: 39.8 kg Anorexia Nervosa overweight Female athlete Triad Binge eating disorder EDNOS “non-purging” BN Bulimia Nervosa Anorexia Nervosa overweight Female athlete Triad Binge eating disorder “non-purging” BN Bulimia Nervosa EDNOS 6/17/09 : wt 51 kg Mom reports pt caught exercising and vomiting in bathroom Anorexia Nervosa overweight Female athlete Triad Binge eating disorder “non-purging” BN EDNOS Bulimia Nervosa 8/18/09 : wt 56.6 kg “binging and purging constantly” Anorexia Nervosa overweight 10/15/09 : Female athlete Triad wt 70.7 kg Binge eating No purging. Eating powdered disorder EDNOS scandishakes from the sink Bulimia Nervosa 10/21/10 : wt 99.7kg Anorexia Nervosa overweight Female athlete Triad Binge eating disorder EDNOS “non-purging” BN Bulimia Nervosa 7/7/11:hospital admission for abdominal pain. Wt 72.5 kg Anorexia Nervosa overweight Female athlete Triad Binge eating disorder EDNOS “non-purging” BN Bulimia Nervosa Crossing Over • 28 % of patients with AN (n = 108) had premorbid body weight of 115 % IBW or greater1 . • Up to 30% of obese patients may have BED2 • Overweight patients commonly use diet pills/laxatives/purging to try to lose weight (18% F, 8% M )3 • People with BN are 3 times more likely to be obese as a child4 1Crisp et. al. (1980) 2Streigal-Moore et al. (2004) 3Neumark-Sztainer et al. (2006) 4 Fairburn et al. (1997) Dieting behavior in children adolescents is common • • • • 60% of female students trying to lose wt. 29% of male students trying to lose wt. 21% of females use diet pills 7 % of females have tried vomiting Source YRBSS 2003 “Dieting” and Weight Status • Parental dieting and “fat talk” is associated with disordered eating, decreased body satisfaction and increased weight status in children • Personal history of dieting is associated with higher BMI and increased weight gain since the onset of “dieting” “Diabulimia” • Up to 50% of women with Type 1 Diabetes binge eat. • Up to 30% of women with T1DM intentionally withhold or reduce prescribed insulin to control weight • Most DM patients had lost significant weight prior to diagnosis and gain weight past baseline with treatment. • The standard treatment of T1DM are behaviors that are intrinsic to eating disorders. Obesity Trends* Among U.S. Adults BRFSS, 1985 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% Obesity Trends* Among U.S. Adults BRFSS, 1986 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% Obesity Trends* Among U.S. Adults BRFSS, 1987 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% Obesity Trends* Among U.S. Adults BRFSS, 1988 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% Obesity Trends* Among U.S. Adults BRFSS, 1989 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% Obesity Trends* Among U.S. Adults BRFSS, 1991 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1992 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1993 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1994 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1995 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1996 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% Obesity Trends* Among U.S. Adults BRFSS, 1997 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% ≥20% Obesity Trends* Among U.S. Adults BRFSS, 1998 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% ≥20% Obesity Trends* Among U.S. Adults BRFSS, 1999 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% ≥20% Obesity Trends* Among U.S. Adults BRFSS, 2000 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% ≥20% Obesity Trends* Among U.S. Adults BRFSS, 2001 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% ≥25% Obesity Trends* Among U.S. Adults BRFSS, 2002 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% ≥25% Obesity Trends* Among U.S. Adults BRFSS, 2003 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% ≥25% Obesity Trends* Among U.S. Adults BRFSS, 2004 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% ≥25% Obesity Trends* Among U.S. Adults BRFSS, 2005 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% 25%–29% ≥30% Obesity Trends* Among U.S. Adults BRFSS, 2006 (*BMI ≥30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%–14% 15%–19% 20%–24% 25%–29% ≥30% Adolescent Obesity is Increasing • NHANES III – 22-23% of American Children are above the 85th percentile for BMI. – 10.5% are above the 95th percentile for BMI. – Adolescent obesity is associated with significant morbidity and mortality in both the short and long term. NIDDM is Epidemic • Between 1982 and 1994: 10-fold increase in new diagnosis in pediatric populations1 • Type 2 Diabetes represents up to 50% of new pediatric Diabetes diagnoses • Impaired glucose tolerance in 25% of obese children and 21% of obese adolescents2 1 Pinhaus-Hamiel 2 Sinha et al, J Pediatr. 1996 May;128(5 Pt 1):608-15. et.al. NEJM 2002 Mar; 346(11):802-10 Pediatric Hypertension is Increasing • Concordant increase in SBP and BMI in middle school students between 1986 and 19961 • In children aged 8-17 over the past 15 years – 1.4 mm/hg in SBP – 3.3 mm/hg2 in DSP Sources: 1Leupker, 1999 2Muntner, JAMA, 2004 Bogalusa Heart Study • Atherosclerosis begins at an early age – Coronary artery and aortic plaques found as early as age 5 • Atherosclerotic plaques in childhood associated with traditional risk factors Metabolic Syndrome (as defined by Reaven) • Hyperinsulinemia • Obesity • Hypertension • Dyslipidemia Metabolic Syndrome in Youth • At least 3 of the following: – – – – – Abdominal obesity Low HDL Hypertriglyceridemia Hypertension Impaired Glucose Tolerance • 30% of overweight Hispanic children with FHx of NIDDM meet criteria for Metabolic syndrome.1 • 37.8% of moderately obese and 49.7% of severely obese subjects meet criteria for metabolic syndrome2 1Cruz 2 et. al. J Clin Endocrinol Metab. 2004 Jan;89(1):108-13 Weiss et al. NEJM. 2004 June ; 350 (23) 2362-2374 . Prevalence of eating disorders • Anorexia Nervosa – Females 0.5-1% – Males 5-10 % of all cases (female:male 9-1) • Binge Eating Disorder: (among college students) – Females 2.8% – Males 1.9% – (Spitzer 1993) • Bulimia Nervosa – Females 1-3% – Males 0.1-0.3 % EDNOS up to 20 % of adolescents Prevalence of Eating Disorders • Eating disorders have been steadily increasing since the 1950s • Changing demographics – – – – More males More minorities More worldwide Younger and younger • Hospitalizations for ED for children younger that 12 have increased 119% from 1999-2006 America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco 1140 Kcal 75g fat America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco America is an Obesogenic Society. . . • • • • Supersizing Marketing high sugar foods to children Unhealthy foods marketed as good for you Nintendo and X-Box, Social media – Thumb exercises • Healthy foods are more expensive • Elevators and Moving sidewalks • The 4 N’s – ‘Net – Nintendo – Nickelodeon – Nabisco . . . In a Culture which Stigmatizes Obesity • Thin is ideal, the thinner the better • Abundance of quick weight loss schemes • Overweight = negative personality traits . . . In a Culture which Stigmatizes Obesity • Thin is ideal, the thinner the better • Abundance of quick weight loss schemes • Overweight = negative personality traits . . . in a Culture which Stigmatizes Obesity • Thin is ideal, the thinner the better • Abundance of quick weight loss schemes • Overweight = negative personality traits HIPAA Evaluating Adiposity • BMI = wt (Kg)/ht (m)2 – Limited by inability to differentiate LBM from adiposity • Skinfold measurements – limited by operator dependence • Water Submersion – you can’t afford it • Air Dispacement (BodPod), TOBEC, DEXA, MRI/CT – Ditto • Bioimpedence- Dependant on hydration status • Visual test HIPAA HIPAA SAME BMI Anorexia Nervosa-Diagnostic Criteria (DSM IV) • Weight of less than 85% expected • Intense fear of becoming fat • Disturbance in the perception of ones weight • Amenorrhea in post menarchal females – Absence of 3 consecutive cycles – RESTRICTING TYPE – BINGE/PURGE TYPE Female Athlete Triad • Disordered Eating • Amenorrhea • Osteopenia – Results when caloric intake is insufficient for the increased need associated with vigorous exercise – May be of normal weight but manage like an anorexic Bulimia Nervosa-Diagnostic Criteria (DSM IV) • Recurrent episodes of Binge Eating, characterized by both of the following: – Eating, in a discreet period of time, more than most people would eat during a similar time period under similar circumstances – A sense of lack of control during such episodes • Recurrent inappropriate compensatory behaviors to prevent weight gain – ie. Laxatives, vomiting, exercise, fasting Bulimia Nervosa-Diagnostic Criteria (DSM IV) • At least twice/week for 3 months • Self-image unduly influenced by weight • The disturbance does not occur solely during episodes of AN BED - Diagnostic Criteria (DSM IV-Appendix B) • Recurrent episodes of Binge Eating, characterized by both of the following: – Eating, in a discreet period of time, more than most people would eat during a similar time period under similar circumstances – A sense of lack of control during such episodes • The binge eating is associated with three or more of the following: – – – – – Eating much more rapidly than normal Eating until uncomfortably full Eating large amounts when not hungry Eating alone due to embarrassment Feeling disgust or guilt about eating BED - Diagnostic Criteria (DSM IV- Appendix B) – Marked Distress towards Binge eating – Twice weekly for 6 months – Not associated with compensatory behavior or does not occur exclusively during AN or BN Eating Disorder not Otherwise Specified (EDNOS) • Disorders of eating that do not fit full the criteria for AN or BN • Common examples: – All criteria for AN except regular menses – All criteria for AN except wt. >85% expected – All criteria for BN except does not occur twice/week, or for 3 months – Purging without binging The DSM 5 will swallow a lot of this up in the other diagnoses (www.dsm5.org) Perpetuating factors (cont.) 24 hr energy expenditure Elevated Body Weight Physical activity energy expenditure Thermic effect of eating T-3 Sympathetic tone Parasympathetic tone Usual Body Weight (Lean or Obese) 24 hr energy expenditure Energy expenditure physical activity Thermic effect of eating T-3 Sympathetic tone Parasympathetic tone Reduced Body Weight Hormonal And Neural Control of AppetiteSerotonin • Increases satiety • Decreased in low weight AN but increased from normal in long term recovered AN • Possibly lower in BN; Binge on tryptophan? • Decreased in obese and correlated with carbohydrate cravings Hormonal And Neural Control of AppetiteNorEpi and Dopamine • Norepi is Orexigenic: Altered in low-weight AN but normal in recovery • BN- NorEpi low baseline but increased in in response to meals • Dopamine is associated with eating pleasure-Certain obese patients have an allele which is associates with reduced D2 receptors Hormonal And Neural Control of Appetite -Cholecystikinin (CCK)• induces satiety • AN low in low weight and normal in recovered (expected response) • BN inadequate rise after meals • Obese No specific effect Hormonal And Neural Control of Appetite -Cortisol • Secreted in response to stress- may increase appetite – Elevated in those with disordered eating • Higher cortisol is associated with higher ED attitudes and behaviors regardless of BMI status • Likely an adaptive response to starvation which perpetuates the behaviors. – Lawson et. Al; Eur J Endocrinol. 2011 Feb;164(2):253-61. Hormonal And Neural Control of Appetite –Peptide YY • Secreted in the intestine in response to food intake – Strong anorexic effect – Appear to be high in disordered eating and malnutrition and associated with drive for thinness – Low in obese subjects. Hormonal And Neural Control of Appetite Ghrelin – abnormally increased in BNpossibly decreased sensitivity in AN. NPY and PPY- Very potent appetite stimulators No specific differences adiponectin; agouti related protein; leptin; resistin; others-further study needed The Dichotomy • Obese = you should be unhappy about you weight • you are only successful in the program if you lose weight (you are “non-compliant” if you can’t/won’t) – Losing weight will improve your life – You may want to eliminate certain macronutrients (ie fat, carbs etc.) “Follow this diet, Mr. Figby, and I want to see twothirds of you back here for a check-up” The Dichotomy • Anorexia Nervosa = You are healthy at any size – Body weight does (or should) not reflect happiness – You should be comfortable with all types of food and dismiss “food phobias” – “It’s donut day in the AN ward” “Health at Every Size” • Accepting and respecting the natural diversity of body sizes and shapes. • Eating in a flexible manner that values pleasure and honors internal cues of hunger, satiety, and appetite. • Exercising for pleasure and the joy of physical movement rather than to lose weight. I don’t stop eating when I’m full. The meal is not over when I’m full. The meal is over when I hate myself! Dietary treatment goals • Attain skills for a lifetime of weight management – self monitoring of eating, physical activity and weight – social and emotional support • Realistic weight goal (may differ from that initially expressed by the teen or parents) Psychological Treatment • Cognitive Behavoral Therapy (CBT) – the mainstay of treatment for disordered eating – Demonstrated effectiveness in BN and BED. Emphasizes the interrelationships between thoughts, feelings, and behaviors as they relate to a situation. – Structured, collaborative, time limited approach to increasing capacity to identify, challenge, and modify problem thoughts and behaviors Family Based Therapy (Mauldsley Method) Demonstrated effective, and superior to CBT in younger patients with AN Pharmacotherapy in ED • High dose SSRI (60 mg. Fluoxetine) has been shown in studies to decrease binge-purge cycles in bulimia • No medication has been shown to be more effective than placebo for AN, but studies have only been done on those patients with very low weight. • SSRIs may be effective for treating comorbidities (OCD, major depression, PTSD) • To nourish the brain, you must nourish the body Pharmacotherapy in Obesity Approved: • Sibutramine (Meridia) • Orlistat (Xenical) Off label: • Fluoxitine (Prozac) • Topirimate (Topamax) Dangerous: • Ephedrine – Ephedrine/Caffeine (off the market) Pulling it together: • Your goal weight is whatever your weight happens to be when living a healthy lifestyle • Even if you can’t lose/gain weight you are not a bad person or a failure, you just have a problem you need to work on which is NOT YOUR FAULT • Model good, healthy behaviors • Have realistic goals Do: • Be sensitive and contemplative about addressing weight issues with kids and families • Associate excess adiposity with health risks and comfort issues rather than self worth and cosmetic issues • Practice anticipatory guidance about unhealthy weight loss behaviors • Encourage and congratulate even small behavior changes, even if they don’t bring immediate “results” Don’t • Tell an adolescent that they “need to lose 50 pounds” • Use sensitive terms like “obese” “fat” “chunky” • Criticize a patient who is not meeting a weight goal • Suggest a restriction without suggesting a substitution Disordered Eating center of Charleston • Multidisciplinary, multicampus team • Stephen B. Sondike MD, Medical Director Jessica Luzier, PhD, Clinical Director Jamie Oliver, RD, Dietician Morgantown Contacts: Pamela Murray, MD J. Scott Mizes, PhD THANKS!