S. aureus
advertisement
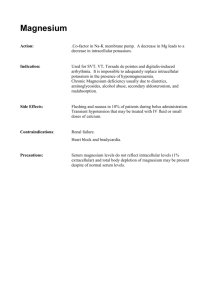
Intracellular Pathogens MIC4124 Thien-Fah Mah, PhD Department of Biochemistry, Microbiology and Immunology Dr. Mah’s path to U of O 1 35 4 1. B.Sc in Microbiology, UBC, Vancouver, BC 2. Three years of work (lab, library, teaching) and travel 3a. M.Sc. in Molecular and Medical Genetics, U of Toronto 3b. Ph. D in Molecular and Medical Genetics, U of Toronto 4. Postdoctoral training at Dartmouth Medical School, Hanover, NH 5. Assistant Professor, U of Ottawa (2005) http://www.worldmapsonline.com/classroommaps/ECNorthAmericaPhys.jpg Dr. Desjardin’s path to the Ottawa Hospital • 1985-1989: BSc with honours Biology - University of Ottawa • 1989-1996: Graduate studies - PhD in Microbiology (used to be Dept of Micro and Immuno) U of Ottawa • 1996-1998: Clinical Microbiology residency fellowship: Strong Memorial Hospital, Rochester New York • 1998-2002: Director Microbiology Laboratory Binghamton General Hospital, Binghamton New York • 2002: Board Certification examination - Diplomat American Board of Medical Microbiology and Fellow of the Canadian College of Microbiology • 2002: I'm back in Ottawa as a Clinical Microbiologist What is an intracellular pathogen? • A microbe that is capable of causing damage to its host that spends at least part of its lifecycle within a host cell or host cell vacuole – ability to replicate within the host cell – ability to persist within the host cell Why be an intracellular pathogen? • Life outside a cell is harsh – Low pH, shear stress due to circulatory system, complement, antibodies, macrophages, T cells • Bacteria can hide out and replicate inside the cell cytoplasm or inside vacuoles (phagosomes) within cells – Bacteria can invade into underlying tissue Some notable intracellular pathogens • Coxiella burnetii - Q fever (highly contagious- only a single bacterium required for infection; flu-like symptoms can progress to pneumonia and acute respiratory distress syndrome (ARDS) and death) • Legionella pneumophila* - Legionnaires disease • Listeria monocytogenes* – Listeriosis • Mycobacterium tuberculosis* – Tuberculosis • Rickettsia prowazekii – epidemic typhus (occurs after wars and natural disasters; headache, fever, chills, delirium, death) • Salmonella enterica* – gastroenteritis and typhoid fever • Shigella flexneri – shigellosis (bloody diarrhea and fever, usually resolves within a week) Entry into a cell • by phagocytosis (cell-eating) – by professional phagocytes like neutrophils, macrophages and dendritic cells • by induced uptake – by cells that are not normally phagocytic (endothelial and epithelial cells) Phagocytosis Receptor mediated, actin-driven process whereby foreign objects larger than 0.5 mm are internalized and degraded. http://www.nature.com/nri/journal/v8/n2/full/nri2240.html Phagocytosis animation http://highered.mcgraw-hill.com/sites/0072495855/student_view0/chapter2/animation__phagocytosis.html Induced uptake Knodler, LA et al 2001 Nat Rev Mol Cell Biol 2(8): 578-588 Host actin • primary host determinant of cell shape and cytoplasmic structure • Rho family of GTPases (Rho, Rac, Cdc42) is important for actin organization • bacteria manipulate the actin cytoskeleton to induce or prevent phagocytosis Actin cytoskeleton http://scienceblogs.com/transcript/2007/01/cytoskeleton.php Antiphagocytic action of Y. pestis Yop proteins Cornelis, GR 2002 Nature Rev Mol Cell Biol 3:742-52 Persistence • Two possible mechanisms allowing pathogens to persist within the host cell: – Modification of endocytic pathway • Salmonella enterica • Mycobacterium tuberculosis • Legionella pneumophila – Escape from endocytic vesicle (phagosome) • Listeria monocytogenes • Maybe M. tuberculosis? • Maybe Staphylococcus aureus? Endocytic and exocytic pathways http://www.landesbioscience.com/curie/chapter/4274/ Endocytic (phagocytic) pathway Haas, A 2007 Traffic 8:311-330 Endocytic (phagocytic) pathway Haas, A 2007 Traffic 8:311-330 Phagosomal Maturation • phagosomes mature due to sequential addition of cellular proteins delivered to them by fusion with different endosomal compartments • anything left in the phagosomes will be destroyed • bacteria need to either – escape before the phagosome environment becomes bactericidal – modify the phagosomal maturation process Bacteria inside phagosomes -membrane is derived from host plasma membrane -single or multiple bacteria per vesicle -ultimate goal: destruction of bacteria by antimicrobial compounds Haas, A 2007 Traffic 8:311-330 How phagosomes kill bacteria -nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex produces superoxide radicals from oxygen -nitric oxide synthetase produces NO radicals -vacuolar ATPase pumps protons into the phagosome in reduce pH to ~4.5 -fusion with lysosomes results in delivery of various hydrolases that digest most biological macromolecules Haas, A 2007 Traffic 8:311-330 Ways to study bacterial-phagosomal interactions • Direct microscopic observation • Characterize the vacuoles that contain bacteria using immunofluorescence colocalization – correlate the presence and absence of various host markers with the presence of the bacterium • Directly measure physiological parameters of the phagosome – pH – hydrolytic activities Colocalization of V-ATPase with bacterial DNA -Monolayer of epithelial cells infected with S. aureus at MOI 10:1 -V-ATPase labelled with antibody -DNA stained with To-Pro-3 Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 Acidification of a phagosome -measurement of pH following internalization of a bead -concanamycin A inhibits V-ATPase Rohde, K et al 2007 Immunol Rev 219:37-54 Salmonella enterica • Gram negative pathogen – gastroenteritis (self-limiting, mild) to typhoid fever (fatal) • Virulence factors mainly located on one of two Salmonella pathogenicity islands, SPI-1 or SPI-2 – encode type III secretion systems important for invasion of non-phagocytic cells and bacterial replication in phagosomes Pathogenicity Islands • Large genomic regions that are present in pathogens but absent in their non-pathogenic counterparts • % GC content quite different from surrounding DNA (suggests that DNA acquired from different organism) • Found in both gram negative and gram positive bacteria • Carry virulence genes • Carry factors that promote mobility (integrases, transposases, IS elements) SPI-1 and SPI-2 Hansen-Wester and Hensel 2001 Microbes Infect 3: 549-559 Intracellular S. enterica Step I: using SPI-1 type III secretion system -injection of effectors that mediate uptake Step II: SPI-2 effectors mediate formation of Salmonella-containing vesicles (SCVs) Knodler, LA et al 2001 Nat Rev Mol Cell Biol 2(8): 578-588 http://www.hhmi.org/biointeractiv e/disease/salmonella.html Salmonella-containing vesicle (SCV) • can persist for hours to days • formation requires genes from SPI-2 • characterized by several endosomal markers – EEA1 (early endosomal marker) – Rab5 and Rab11 (middle) – Rab 7, LAMP1, LAMP2, LAMP3, V-ATPase (late) – low pH (indicative of lysosomal fusion) – transient? Steele-Mortimer,Finlay Cell. Micro. (1999) 1(1), 33-49 Salmonella-induced filaments (Sifs) • • • • 4-6 hours after SCV formation, see salmonella-induced filaments (sifs) not sure what their function in pathogenesis is not sure what effectors do Sif formation not yet shown in vivo Rajashekar R et al 2008 Traffic Salmonella-induced filaments (Sifs) • • • • 4-6 hours after SCV formation, see salmonella-induced filaments (sifs) not sure what their function in pathogenesis is not sure what effectors do Sif formation not yet shown in vivo Rajashekar R et al 2008 Traffic Salmonella genes important for intracellular life Modulation of host cytoskeleton (SPI-1) SopB-activates Cdc42 and Rho SopE-activates Cdc42, Rac and Rho SopE2-activates Cdc42, Rac and Rho SipA-actin nucleation SipC-actin nucleation Formation and Maintenance of SCV (SPI-2) SifA-Sif formation SopD2- Sif formation SseJ- maintains SCV integrity Steele-Mortimer,Finlay Cell. Micro. (1999) 1(1), 33-49 Haraga A et al 2008 Nat Rev Microbiol 6: 53-66 Mycobacterium tuberculosis • • • • Gram positive Reservoir: humans Causes tuberculosis, spread by aerosols Enters host macrophages and subverts normal phagosome maturation • Persists in a granuloma http://www.sunysb.edu/icbdd/images/infectious2.jpg Infected macrophages and the granuloma Intracellular M. tuberculosis Granuloma Russell 2007 Nat Rev Microbiol 5:39-47 M. tuberculosis Phagosome • M. tuberculosis – Blocks rab conversion – Retains characteristics of early endosome (Rab5 and EEA-1) – Phagosome pH only reaches pH 6.5 Adapted from Via and Deretic 1997 JBC 272:13326-13331 Rab conversion block -Rab5 (early) and Rab7 (late) are GTPases involved in endosome maturation -Rab conversion occurs when Rab5 is replaced with Rab7 Deretic, V. et al 2006 Cell Microbiol 8:719-727 Rab conversion block Mycobacterial factors that cause the block: – Liparabinomannan (LAM) is a lipid (part of mycobacterial cell wall) that prevents the increase of cytosolic [Ca2+] that normally accompanies phagocytosis (and this affects the recruitment of a Rab5 effector) – Phosphatidylinositol mannoside (PIM)- mechanism unknown – SapM is a PI3P phosphatase * *PI3P is important for proper membrane trafficking through the endosomal pathway Recent observations suggest that M. tuberculosis can escape into the cytosol Direct microscopic observations suggested that M. tuberculosis was not blocking phagosomal maturation at early stages…. -M. tuberculosis in dendritic cells at 2 hours -bacteria (star) colocalize with LAMP-1 (dot)(late endosomal marker) -lysosomes fuse with M. tuberculosiscontaining phagosome Van der Wel et al 2007 Cell 129:1287-98 Evidence of escape into cytosol 4 hours 96 hours -green= bacteria -red= LAMP-1 -blue=host cell DNA -yellow=green and red merged *also counted number of bacterial cells at 4 hours and 96 hours and saw increase Van der Wel et al 2007 Cell 129:1287-98 More evidence for escape into cytosol -no phagosomal membrane surrounding M. tuberculosis at 96 hours and no association with LAMP-1 (dots) -escape into cytosol requires RD1 (regions of difference between pathogenic and non-pathogenic mycobacteria) genes (contains ESAT/type VII secretion system) Van der Wel et al 2007 Cell 129:1287-98 Non-pathogenic mycobacterium does not escape into cytosol -M. bovis (vaccine strain) (green) cocolocalizes (yellow) with LAMP-1 (red) -host cell DNA (blue) -evidence of phagosomal membrane surrounding bacteria -association with LAMP-1 (dots) Van der Wel et al 2007 Cell 129:1287-98 Listeria monocytogenes • • • • Gram positive Ubiquitous in the environment Intracellular pathogen Causes listeriosis – acquired by ingesting contaminated food – mainly affects the elderly, the very young, immunocompromised individuals and pregnant women – results in gastoentiritis, meningitis, encephalitis, septicaemia and death in 25-30% of cases http://www.rps.psu.edu/indepth/graphics/knabel2.jpg Genes required for L. monocytogenes to invade and spread L. monocytogenes avoids destruction by escaping into host cytosol http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VPN-4NNN0J0-6&_user=1067359&_rdoc=1&_fmt=&_orig=search&_ sort=d&view=c&_version=1&_urlVersion=0&_userid=1067359&md5=30ef1ede32268634f516a8778f263c32 Genes required for survival in the host • inlA and inlB (invasion-associated surface proteins internalin A and B: mediate invasion of nonphagocytic cells) • hly (listeriolysin O or LLO: pore-forming toxin) • plcA and plcB (phospholipase C enzymes: phagocytic vacuole disruption) • actA (actin polymerization) • mpl (metalloprotease required for PlcB maturation) • hpt (hexose phosphate transporter important for rapid growth in host cytosol) LLO • a primary virulence factor facilitating escape from the phagosome and cell-to-cell spread • member of pore-forming cholesteroldependent cytolysin family (C. perfringens, S. pyogenes, B. anthracis) • active at pH 5.5 (therefore active in phagosome and not in cytosol) Mechanism of cholesterol-dependent cytolysin pore formation Monomers bind cholesterol, diffuse laterally…. Tweten 2005 Infect Immun 73:6199-6209 Mechanism of cholesterol-dependent cytolysin pore formation …to form membrane prepore of sufficient size a-helical bundles in prepore are converted into amphipathic transmembrane b-hairpins… Tweten 2005 Infect Immun 73:6199-6209 Mechanism of cholesterol-dependent cytolysin pore formation …and the prepore collapses 40Å such that specific domains are inserted into the membrane The end result is the formation of a large b-barrel pore Tweten 2005 Infect Immun 73:6199-6209 ActA • identified in a screen for bacteria deficient in cell to cell spreading • required for actin-based motility • bacterial surface protein that interacts with several host proteins Actin comet tails • after a few hours of growth, host actin filaments form on surface of bacteria • polarization into a comet tail (cross-linked network of actin filaments) Cameron LA et al 2000 Nat Rev Mol Cell Biol 1:110-119 Actin-Arp2/3-ActA interaction actin profilin Arp2/3 -vasodilator-stimulated phosphoprotein (VASP) interacts with profilin (actin binding protein) -Arp2/3 is a 7 protein complex that nucleates actin Cameron LA et al 2000 Nat Rev Mol Cell Biol 1:110-119 Listeria with actin tails http://mcb.berkeley.edu/labs/portnoy/ Theriot lab movies • http://cmgm.stanford.edu/theriot/movies.htm Actin-based motility in other systems • • • • Shigella flexneri Rickettsia species Vaccinia virus Enteropathogenic E. coli (pedestal formation) Refs: Goldberg 2001 Microbiol Mol Biol Rev 65:595-626 Cameron et al 2000 Nat Rev Mol Cell Biol 1:110-119 Legionella pneumophila • Gram negative • Found as parasite of freshwater protozoa • Infects alveolar macrophages and causes severe pneumonia • Legionnaires disease – Outbreak at a war vet convention in Philadelphia 1976 (34 deaths) – isolated bacterium from cooling tower that linked to the air conditioning system of the hotel – Climate control changes implemented Legionnaires disease today • http://www.cbc.ca/news/health/story/2012/01/11/legionnai res-disease-hospitals-water-features.html Intracellular L. pneumophila • Legionella containing vacuole (LCV) – Does not fuse with late endocytic vesicles • Resists lysosomal degradation • Associates with smooth vesicles and is decorated with ribosomes • Is a replication niche • Smooth vesicles are derived from ER – Unique biomarkers for ER – Believed that this is a source of polypeptides (energy for bacterial replication) – Camouflage? L. pneumophila modulates phagocytic pathway -L. pneumophila creates intravacuolar niche for replication -normal phagocytic pathway -normal eukaryotic secretory membrane system (from endoplasmic reticulum [yellow], to golgi complex, to the plasma membrane) Isberg et al 2009 Nat Rev Micriobol 7:13-24 L. pneumophila modulates phagocytic pathway -L. pneumophila creates intravacuolar niche for replication Isberg et al 2009 Nat Rev Micriobol 7:13-24 Type IV secretion: Dot/Icm gene locus mediates intracellular survival • Genetic screen identified mutants defective in intracellular replication • Dot/Icm: defect in organelle trafficking/intracellular multiplication genes • Type IV secretion system required for delivery of proteins across the host cell membrane (phagosome membrane) Dot/Icm secretion apparatus Isberg et al 2009 Nat Rev Microbiol 7:13-24 Legionella containing vacuole (LCV) -several Dot/Icm effectors associate with the LCV and recruit host proteins (boxed) that are involved in vesicle trafficking through the secretory pathway Isberg et al 2009 Nat Rev Microbiol 7:13-24 Type IV effectors • A growing number of proteins (effectors) are substrates for the Dot/Icm associated type IV secretion system (30 +) but functions not well understood – Some proposed to promote phagocytosis – Others prevent fusion with normal endocytic vesicles – Some of eukaryotic resemblance suggesting roles in mimicry – Acquisition of eukaryotic genes? ArfI – a host trafficking protein • ArfI is a GTPase responsible for mediating vesicular transport between Golgi and ER – ArfI: inactive [GDP bound form] and active [GTP bound form] – natural cycle • Recruitment of ArfI to membranes requires GEF (guanine nucleotide exchange factor) which remove GDP to allow GTP binding Type IV effector: RalF • RalF – is a GEF (enzymatic activity) – Stimulates ArfI activation promoting its fusion to the LCV • ralF mutant is deficient in ArfI localization to the LCV Type IV effectors • Other effectors are involved – VipA and VipD block lysosomal fusion – LepA and LepB promote Legionella release dissemination – SdhA prevents apoptosis • Key to intracellular survival (cell remains a viable unit to allow replication!) – LidA binds Rab1-GTPase • Modulates vesicular pathway Staphylococcus aureus • gram-positive cocci • production of a large number of secreted toxins • humans are major reservoir (up to 40% are carriers) • major nosocomial pathogen • emergence of antibiotic resistant strains -MRSA • pathogen of Cystic Fibrosis patients Courtesy of Rob Shanks, Dartmouth Medical school Staphylococcus aureus Escapes More Efficiently from the Phagosome of a Cystic Fibrosis Bronchial Epithelial Cell Line than from Its Normal Counterpart Todd M. Jarry and Ambrose L. Cheung 2006 Infection and Immunity 74(5):2568-2577 S. aureus: intracellular pathogen? • Rationale: – Originally thought to be exclusively extracellular – Why it might not be: “although the role of S. aureus in the disease progression of CF remains unknown, the clinical observation of rapid recolonization soon after treatment suggests that S. aureus may persist inside host cells of the lung”* *Jarry and Cheung 2006 Infect Immun 74:2568-2577 Hypothesis: S. aureus is an intracellular pathogen Experimental set up • Invasion assays – Bacteria were added to host cells in tissue culture plates and allowed to incubate for specific periods of time – Extracellular bacteria were killed with addition of antibiotic (only intracellular bacteria will survive) – Host cells were lysed and bacterial cells were counted • Immunofluorescence – Bacteria were added to host cells, as above – Cells were fixed and antibodies (to LAMP-1 or LAMP-2) were added – Also utilized this technique to observe association with lysotracker Intracellular replication CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 Attachment vs. Internalization (30 min) CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 Internalization of different bacteria CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 S. aureus loses association with LAMP-1 and LAMP-2 over time CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 S. aureus loses association with LAMP-1 and LAMP-2 over time CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 S. aureus loses association with acidic vesicles over time CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 S. aureus loses association with acidic vesicles over time CFT-1 (dead) LCFSN (dead) LCFSN (live) CFT-1 (live) CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 Model for S. aureus trafficking within a CF mutant cell line CFT-1: CF tracheal cell line (DF508) LCFSN: complemented cell line (wt CFTR) Jarry, TM and Cheung, AL 2006 Infect Immun 74 (5):2568-2577 Is S. aureus an intracellular pathogen? Did they prove or disprove their hypothesis? Summary • S. enterica: SCVs (early, middle and late markers), Sifs • M. tuberculosis: Rab conversion block (early); possible escape into cytoplasm • L. monocytogenes: Escapes from phagosome, invades other cells via actin-based motility • L. pneumophila: LCV mimics host ER? • S. aureus: invades a CF cell line and escapes into the cytoplasm. Reminder: Final exam • April 21, 2012 from 9:30am-12:30pm in Desmarais (DMS) 1160 • Format: – short answer (no multiple choice) • It will cover the lectures from Feb. 15 (Bioterrorism) to April 4 (Intracellular Pathogens) • I will also assign a paper (check Blackboard on April 13, 2012) to read before the exam and you will be asked to answer questions about it. You may NOT bring the paper or any notes to the exam. • I will post a study guide on the Blackboard site on April 11, 2012. Please remember it is just a guide- anything that was addressed during the lectures is fair game Good luck on your exams!