36x48 Horizontal Poster - Center for Primary Care
advertisement

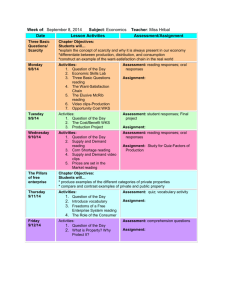
Lawrence Family Medicine Residency Transition to a Four Year Program (an ACGME Length of Training Pilot Program) Wendy Brooks Barr MD, MPH, MSCE; Whitney LeFevre, MD; Clark Van Den Berghe, MD; Joseph Gravel MD Lawrence Family Medicine Residency, Greater Lawrence Family Health Center, Lawrence, MA • Family Medicine Length of Training Pilot (FMLTP). • Developed by the ACGME Review Committee in Family Medicine (RC-FM), in conjunction with the American Board of Family Medicine (ABFM) • Goals: • To find innovative methods to prepare Family Physicians to “serve as highly effective personal physicians in a high performance health care system.” • Inform whether four years should become the standard length of training in Family Medicine • Evaluation method: Match and compare selected programs with a group of existing three-year programs • Evaluation Team: Oregon Health and Science University • Timeline:: Selected 2013, evaluation through 2019 • Selected 4 Year Residency Program: • • • • • • • • • • Mid Michigan Medical Center-Midland (Michigan) Middlesex Hospital FMR (Connecticut) John Peter Smith Hospital (Texas) Oregon Health and Science University Program (Oregon) Lawrence Family Medicine Residency (Massachusetts) University of Nevada, Reno (Nevada) National Capital Consortium (Virginia) US Naval Hospital Camp LeJeune (North Carolina) US Naval Hospital Camp Pendleton (California) US Naval Hospital Jacksonville (Florida) 1. Development of competencies in all aspects of PCMH in our NCQA Level 3 Family Medicine Center through immersion in and graduated responsibility for management of the medical home. Including: a. team-based care b. population medicine c. community health d. information mastery e. chronic disease management f. practice-based improvement g. leadership 2. Increased depth of experience in core clinical aspects of Family Medicine, particularly essential in low resource clinical environments, with development of added competencies key to the care of underserved populations. 3. Increased opportunity for residents to develop additional competencies in areas of personal interest through the expansion of areas of concentration (AOCs). 4. More meaningful and longitudinal community experiences which will serve as a foundation for substantive community involvement for residents throughout their careers. 1. Successful recruitment of high quality residents into the program as measured by: • 100% Match Rate • Increased number of US medical seniors applying to the program • Matched residents with higher achievements USMLE Step 2 scores R1 In-training Exam Scores National Medical Student Recognitions (AOA, Gold Humanism, Pisacano) 2. A high level of resident achievement in residency as measured by: • Initial ABFM Certification Exam scores • Community involvement during residency • Completion of QI and scholarly activity projects 3. A high percentage of graduates reporting: • • • • Leadership roles in CHCs Leading QI projects in their practices Working in HPSA or international sites Practicing full-spectrum family medicine Applicant Metrics By Recruitment Year 1000 900 800 700 600 500 400 300 200 100 0 Total Applicants US Grads Avg Matched Step2 R1 ITE Score 2009 (Class of 2010 (Class of 2011 (Class of 2012 (Class of 2013 (Class of 2014 (Class of '13) '14) '15) '17) '18) '19) • Changing to required 4 year curriculum has not hurt recruitment • Trend towards more total applicants and US medical school seniors • Trend toward higher R1 ITE scores and no change on Step 2 Scores of matched applicants www.postersession.com Lawrence Family Medicine Residency Transition to a Four Year Program (an ACGME Length of Training Pilot Program) Wendy Brooks Barr MD, MPH, MSCE; Whitney LeFevre, MD; Clark Van Den Berghe, MD; Joseph Gravel MD Lawrence Family Medicine Residency, Greater Lawrence Family Health Center, Lawrence, MA GOALS: Provide residents with opportunities to develop advanced competency in an area of interest. Develop resident skills in self-directed learning and promote the practice of life-long learning and skill development. R1 R2 Global Health Advanced Surgical Maternity Care Integrative Medicine Phase 1 AOCs HIV R3 R4 Adult Medicine (10 wks) Adult Medicine (4 wks) ICU (4 wks) AM NF Maternity Care MC/PD NF Pediatrics Surgery (2 wks) (6 wks) (4 wks) (4 wks) (2wks) AM NF (4 wks) Maternity Care (4 wks) MC/PD NF (2 wks) Adult Medicine AM MC MC/PD NF Pediatrics NF (2 wks) (4 wks) (6 wks) (4 wks) (2 wks) Adult Clinic FM MC/ Peds Medicine NF MC PD NF ED Chief/PCMC (2 wks) (2 wks) (2 wks) (2 wks) (4 wks) (6 wks) Peds PD Neo ED (2 wks) (2wks) ED (4 wks) Outpatient Longitudinal (14 wks) ED (2 wks) (4 wks) UMASS Sports Med (4 wks) Outpatient Longitudinal (16 wks) Outpatient Longitudinal (10 wks) Outpatient Longitudinal (20 wks) Spanish/ Spanish Intro to Vacation Elective FM (4 wks) (2wks) (4 wks) Longitudinal AOC (4wks) Longitudinal AOC (4wks) AOC (4 wks) AOC (8 wks) Elective Vacation (4 wks) (4 wks) Elective Vacation (4 wks) (4 wks) Elective Vacation (2 wks) (4 wks) (Active) Academic/Faculty Development Health Systems Leadership Sports Medicine Women’s Health Behavioral Health Phase 2 AOCs (In Progress) Addiction Medicine / Pain Management Outpatient Longitudinal Curriculum Content by Year of Training R1: Gynecology, Orthopedics/Sports Med, Geriatrics, Behavioral Health, PCMH, Outpatient Pediatrics, Community Medicine R2: Gynecology, Orthopedics/Sports Med, Surgery, Dermatology, Geriatrics, Palliative Care, PCMH, Community Medicine R3: Behavioral Health, HIV, Addiction Medicine, PCMH R4: Geriatrics, Integrative Medicine, Subspecialty Care, Dermatology, Adolescent Medicine, Outpatient Pediatrics, PCMH, Community Medicine, Innovation Area PCMH Group Visits New / Additional Training R4 “Clinic Chief” block experience; progressive leadership within clinical teams Lead at least 3 cycles of group visits in 2 clinical areas HIV Required experience with HIV-care management team Addiction Medicine Required experience in addiction medicine/chronic pain Mental Health Enhanced focus on team-based behavioral health management Underserved Longitudinal experiences; focus on Care social determinants of health during R1 “education week” Community Longitudinal involvement with Medicine defined community in Lawrence Information Mastery Enhanced didactics; skill tasks in clinical experiences Leadership Increased advocacy efforts; progressive clinical leadership Research Increased curricular time; more research methodology training Population Medicine Review community and patient data; design, implementation and evaluation of interventions based on population data Core longitudinal experiences in proven integrative modalities Hospitalist Integrative Medicine www.postersession.com