Coronary Blood Flow
advertisement

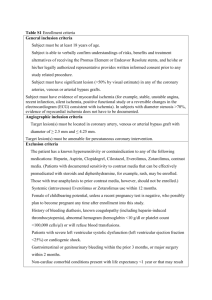
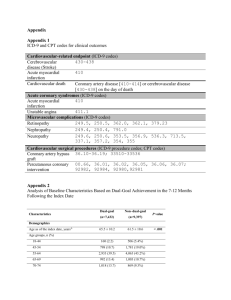
Ischemic Heart Disease and Myocardial Infarction Pathophysiology of Myocardial Ischemia Bio-Med 350 September 2004 Physiology and Pathophysiology of Coronary Blood Flow / Ischemia Basic Physiology / Determinants of MVO2 Autoregulatory Mechanisms / Coronary Flow Reserve Pathophysiology of Coronary Ischemia and Atherosclerosis Clinical Syndromes Stable Angina Acute Coronary Syndromes – Unstable Angina – Acute MI (UA, AMI) Coronary Arteries Normal Anatomy Basic Principles myocardial cells have to do only 2 things: contract and relax; both are aerobic, O2 requiring processes oxygen extraction in the coronary bed is maximal in the baseline state; therefore to increase O2 delivery, flow must increase large visible epicardial arteries are conduit vessels not responsible for resistance to flow (when normal) Basic Principles small, distal arterioles make up the major resistance to flow in the normal state atherosclerosis (an abnormal state) affects the proximal, large epicardial arteries once arteries are stenotic (narrowed) resistance to flow increases unless distal, small arterioles are able to dilate to compensate Myocardial Ischemia: Occurs when myocardial oxygen demand exceeds myocardial oxygen supply Myocardial Ischemia: Occurs when myocardial oxygen demand exceeds myocardial oxygen supply MVO2 = Myocardial Oxygen Demand MVO2 determined by: Heart Rate Contractility Wall Tension MVO2 (Myocardial Oxygen Demand) Increases directly in proportion to heart rate Increases with increased contractility Increases with increased Wall Tension: i.e. increases with increasing preload or afterload Heart Rate 10 8 MVO2 cc/min /100g 6 4 2 100 150 Heart Rate (BPM) 200 Contractility 10 Norepinephrine Control MVO2 (cc/min /100g) 5 0 Peak Developed Tension (g/cm2) Wall Tension Is related to Pressure x Radius Wall Thickness Defined as: Force per unit area generated in the LV throughout the cardiac cycle Afterload - LV systolic pressure Preload - LV end-diastolic pressure or volume Myocardial Ischemia: Occurs when myocardial oxygen demand exceeds myocardial oxygen supply Myocardial Oxygen Supply Determined by: Coronary Blood Flow & O2 Carrying Capacity ( Flow = Pressure / Resistance) Coronary perfusion pressure Coronary vascular resistance Oxygen saturation of the blood Hemoglobin content of the blood Coronary Blood Flow Proportional to perfusion pressure / resistance Coronary Perfusion pressure = Diastolic blood pressure, minus LVEDP Coronary Vascular resistance external compression intrinsic regulation Local metabolites Endothelial factors Neural factors (esp. sympathetic nervous system) Endocardium and CFR Diastole Systole Endocardium vs Epicardium Greater shortening / thickening, higher wall tension: increased MVO2 Greater compressive resistance ? Decreased Perfusion Pressure Less collateral circulation Net Result is more compensatory arteriolar vasodilatation at baseline and therefore decreased CFR Autoregulatory Resistance Major component of resistance to flow Locus at arteriolar level Adjusts flow to MVO2 Metabolic control Oxygen Adenosine , ADP NO (nitric oxide) Lactate , H+ Histamine, Bradykinin Autoregulatory Resistance Involves 3 different cells Myocardial muscle cell - produces byproducts of aerobic metabolism (lactate,adenosine, etc) Vascular endothelial cell (arteriole) - reacts to metabolic byproducts Vascular smooth muscle cell (arteriole) signaled by endothelial cell to contract (vessel constriction) or relax (vessel dilation) Autoregulation of Coronary Blood Flow Oxygen Acts as vasoconstrictor As O2 levels drop during ischemia: precapillary vasodilation and increased myocardial blood supply Adenosine Potent vasodilator Prime mediator of coronary vascular tone Binds to receptors on vascular smooth muscle, decreasing calcium entry into cell Adenosine During hypoxemia, aerobic metabolism in mitochondria is inhibited Accumulation of ADP and AMP Production of adenosine Adenosine vasodilates arterioles Increased coronary blood flow Autoregulatory Resistance 200 Adenosine Flow cc/100g /min 100 0 Control 60 80 100 115 130 Coronary Perfusion Pressure (mmHg) Autoregulators Other endothelialderived factors contribute to autoregulation Dilators include: EDRF (NO) Prostacyclin Constrictors include: Endothelin-1 Coronary Flow Reserve Arteriolar autoregulatory vasodilatory capacity in response to increased MVO2 or pharmacologic agents Expressed as a ratio of Maximum flow / Baseline flow ~ 4-5 / 1 (experimentally) ~ 2.25 - 2.5 (when measured clinically) Coronary Flow Reserve Stenosis in large epicardial (capacitance) vessel decreased perfusion pressure arterioles downstream dilate to maintain normal resting flow As stenosis progresses, arteriolar dilation becomes chronic, decreasing potential to augment flow and thus decreasing CFR Endocardial CFR < Epicardial CFR As CFR approaches 1.0 (vasodilatory capacity “maxxed out”), any further decrease in PP or increase in MVO2 ischemia Coronary Flow Reserve 5 Maximum Flow 4 Coronary 3 Blood Flow 2 Resting Flow 1 0 25 50 75 Epicardial % Diameter Stenosis 100 Endocardium and Collaterals Epicardium Endocardium Coronary Steal A Sub-epicardium B Sub-endocardium Vasodilator Rx (Ado) R2 decreases Flow increases to A R3 - no reserve Increased flow across R1 GRT P1-2 No change in P1 P2 Flow to B is dependant on P2 and Prevalence of CAD in Modern Society 70 60 Age(years) 50 % Donors 70% 40 50% 30 <25 25-40 >40 20 10 25% 0 Clevelend Clinic Cardiac Transplant Donor IVUS Data-Base Risk Factors family History cigarette smoking diabetes mellitus hypertension hyperlipidemia sedentary life-style obesity elevated homocysteine, LP-a ? Coronary lesions in Men and Women, Westernized and non-Westernized diets Relationship between fat in diet and serum cholesterol Atherosclerotic Plaque Evolution from Fatty Streak Fatty streaks present in young adults Soft atherosclerotic plaques most vulnerable to fissuring/hemorrhage Complex interaction of substrate with circulating cells (platelets, macrophages) and neurohumoral factors Plaque progression…. Fibrous cap develops when smooth muscle cells migrate to intima, producing a tough fibrous matrix which glues cells together Intra-vascular Ultrasound (IVUS) Atherosclerotic Plaque Physiologic Remodeling Coronary atherosclerosis Stable Angina - Symptoms mid-substernal chest pain squeezing, pressure-like in quality (closed fist = Levine’s sign) builds to a peak and lasts 2-20 minutes radiation to left arm, neck, jaw or back associated with shortness of breath, sweating, or nausea exacerbated by exertion, cold, meals or stress relieved by rest, NTG Symptoms and Signs: Coronary Ischemia Stable Angina - Diagnosis Exercise Treadmill Test Stable Angina - Diagnosis Thallium Stress Test Stable Angina - Treatment Risk factor modification (HMG Co-A Reductase inhibitors = Statins) Aspirin Decrease MVO2 nitrates beta-blockers calcium channel blockers ACE-inhibitors Anti-oxidants (E, C, Folate, B6)? Stable Angina - Treatment Mechanical Dilation: Angioplasty, Stent, etc. Treatment of Stable Angina STENTS Stable Angina - Treatment Coronary Artery Bypass Grafting Surgery (CABG) Schematic of an Unstable Plaque Unstable Plaque: More Detail……. Cross section of a complicated plaque Journey down a coronary… Angiogram in unstable angina: eccentric, ulcerated plaque Angiogram in unstable angina: after stent deployment Acute Coronary Syndrome Terminology Pathophysiology of all 3 is the same Unstable Angina (UA) ST depression, T Wave inversion or normal No enzyme release Non-Transmural Myocardial Infarction (NTMI or SEMI) ST depression, T Wave inversion or normal No Q waves CPK, LDH + Troponin release Transmural Myocardial Infarction (AMI) ST elevation + Q waves CPK, LDH + Troponin release Pathophysiology of the Acute Coronary Syndrome (UA,MI) Plaque vulnerability and extrinsic triggers result in plaque rupture Platelet adherence, aggregation and activation of the coagulation cascade with polymerization of fibrin Thrombosis with sub-total (UA, NTMI) or total coronary artery occlusion (AMI) Pathophysiology of Acute Coronary Syndromes Pathophysiology of Acute Coronary Syndromes “Vulnerable Plaque” Coronary Stenosis Severity Prior to Myocardial Infarction % Stenosis 68% 14% 18% >70 50-70 <50 Falk et al, Circulation 1995; 92: 657-71 Acute Coronary Syndrome Unstable Angina / Myocardial Infarction Symptoms new onset angina increase in frequency, duration or severity decrease in exertion required to provoke any prolonged episode (>10-15min) failure to abate with >2-3 S.L. NTG onset at rest or awakening from sleep Unstable Angina High Risk Features prolonged rest pain dynamic EKG changes (ST depression) age > 65 diabetes mellitus left ventricular systolic dysfunction angina associated with congestive heart failure, new murmur, arrhythmias or hypotension elevated Troponin i or t Unstable Angina / NTMI Pharmacologic Therapy ASA and Heparin beneficial for acute coronary syndromes ( UA, NTMI, AMI) Decrease MVO2 with Nitrates, Betablockers, Ca channel blockers, and Ace inhibitors consider platelet glycoprotein 2b / 3a inhibitor and / or low molecular weight heparin Anti-Platelet Therapy Three principle pathways of platelet activation with >100 agonists: ( TXA2, ADP, Thrombin ) Final common pathway for platelet activation / aggregation involves membrane GP II b / III A receptor Fibrinogen molecules cross-bridge receptor on adjacent platelets to form a scaffold for the hemostatic plug Platelet GP IIB/ IIIA Inhibitors with Acute Coronary Syndromes Odds Ratios and 95% CI for Composite Endpoint ( Death,Re- MI at 30days ) Placebo (% ) Rx ( % ) PURSUIT 15.7 14.2 PRISM 7.1 5.8 11.9 8.7 11.7 12.0 (vs Heparin) PRISM PLUS (+ Heparin) PARAGON (high dose) 0.2 Rx better 1 4 Placebo better Low Molecular Weight Heparin in Acute Coronary Syndromes Odds Ratios and 95% CI for Composite Endpoint ( Death, MI, Re-angina or Revasc at 6-14 days ) UH / Placebo (%) Rx (%) FRISC 10.3 5.4 FRIC 7.6 9.3 ESSENCE 19.8 16.6 TIMI 11b 16.6 14.2 0.2 LMWH Better 1 UH Better 4 Acute Myocardial Infarction total thrombotic occlusion of epicardial coronary artery onset of ischemic cascade prolonged ischemia altered myocardial cell structure and eventual cell death (release of enzymes - CPK, LDH, Troponin) altered structure altered function (relaxation and contraction) consequences of altered function often include exacerbation of ischemia (ischemia begets ischemia) Acute Myocardial Infarction wavefront phenomenon of ischemic evolution endocardium to epicardium If limited area of infarction homeostasis achieved If large area of infarction (>20% LV ) Congestive heart failure If larger area of infarction (>40% LV) hemodynamic collapse AMI - Wavefront Phenomenon Acute Myocardial Infarction Non-transmural / sub-endocardial Non-occlusive thrombus or spontaneous reperfusion EKG – ST depression Some enzymatic release – troponin i most sensitive Transmural total, prolonged occlusion EKG - ST elevation Rx - Thrombolytic Therapy or Cath Lab / PTCA Cardiac enzymes: overview Legend: A. Early CPK-MB isoforms after acute MI B. Cardiac troponin after acute MI C. CPK-MB after acute MI D. Cardiac troponin after unstable angina Markers of MI: Troponin I Diagnosis of MI: Role of troponin i Troponin I is highly sensitive Troponin I may be elevated after prolonged subendocardial ischemia See examples below Causes of Troponin elevation Any cause of prolonged (>15 – 20 minutes) subendocardial ischemia Prolonged angina pectoris Prolonged tachycardia in setting of CAD Congestive heart failure (elevated LVEDP causing decreased subendocardial perfusion) Hypoxia, coupled with CAD “aborted” MI (lytic therapy or spontaneous clot lysis) EKG diagnosis of MI ST segment elevation ST segment depression T wave inversion Q wave formation Consequences of Ischemia (Ischemia begets Ischemia) chest pain systolic dysfunction (loss of contraction) decrease cardiac output decrease coronary perfusion pressure diastolic dysfunction (loss of relaxation) higher pressure (PCWP) for any given volume dyspnea, decrease pO2, decrease O2 delivery increased wall tension (increased MVO2) All 3 give rise to stimulation of sympathetic nervous system with subsequent catecholamine release- increased heart rate and blood pressure (increased MVO2) Ischemic Cycle Ischemia / infarction Diastolic Dysfunction Systolic Dysfunction chest pain pulmonary congestion pO2 LV diastolic pressure cardiac output wall tension catecholamines (heart rate, BP) MVO2 Treatment of Acute Myocardial Infarction aspirin, heparin, analgesia, oxygen reperfusion therapy thrombolytic therapy (t-PA, SK, n-PA, r- PA) new combinations ( t-PA, r-PA + 2b / 3a inhib) cath lab (PTCA, stent) decrease MVO2 nitrates, beta blockers and ACE inhibitors for high PCWP - diuretics for low Cardiac Output - pressors (dopamine, levophed, dobutamine; IABP; early catheterization TIMI Flow Grades TIMI 0 Flow = no penetration of contrast beyond stenosis (100% stenosis, occlusion) TIMI 1 Flow = penetration of contrast beyond stenosis but no perfusion of distal vessel (99% stenosis, sub-total occlusion) TIMI 2 Flow = contrast reaches the entire distal vessel but either at a decreased rate of filling or clearing versus the other coronary arteries (partial perfusion) TIMI 3 Flow = contrast reaches the distal bed and clears at an equivalent rate versus the other coronary arteries (complete perfusion) GUSTO 30 Day Mortality p-values t-PA vs. t-PA + SK t-PA vs. SK (IV) t-PA vs. SK (SQ) t-PA vs. Combo SK 10 0.04 0.003 0.009 0.001 8 6 7 .2 7 .4 7 .0 6 .3 4 2 0 SK + SQ H e p a r in N: 9,796 S K + IV H epera n 10,376 A c c e l. t-P A 10,344 t-P A + S K 10,327 GUSTO 90 min Patency % of Patients TIM I 3 100 TIM I 2 81 % * 80 60 73 % 56 % 61 % 40 20 N: p < 0.001 p < 0.001 0 SK + SQ H epa rin SK + IV H epa rin A ccel. t-P A t-P A + SK 295 282 291 297 p = < 0.001 for Accelerated t-PA vs. all other arms TIMI Flow Grade Versus Mortality (GUSTO) Mortality p=0.01 12 9 % of Patients 9.7 p=0.05 9.9 6 7.9 3 4.3 0 N TIMI 0 TIMI 1 TIMI 2 TIMI 3 259 81 342 447 Coronary Steal Role of Collaterals Adenosine Rest Flow P2 collateral Flow P1 P2 collateral Assumptions Collateral resistance P1 drops with vasodil P2 bed with no vaso dilator reserve P1 Changing Paradigm – The Concept of Physiologic Remodeling