Case presentation - asja
advertisement

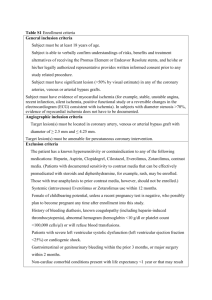
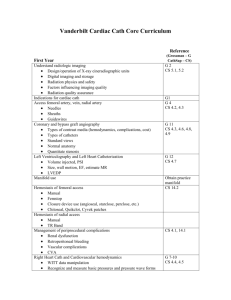
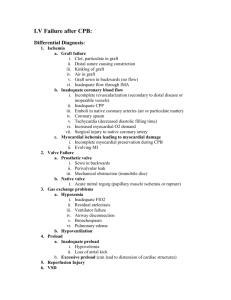
CASE PRESENTATION Dr. Amr Marzouk Assistant lecturer of anesthesia Faculty of medicine Ain shams university • A 68-year-old female, 231 lbs and 5′1″ tall, with a history of hypertension (HTN), diabetes mellitus, and large joint chronic arthritis, is scheduled for a laparoscopic cholecystectomy. • The patient is non-compliant with her treatment: atenolol and glyburide. • On the morning of the surgery, the patient’s blood pressure (BP) was 145/86 mm Hg, heart rate (HR) 88, respiratory rate (RR) 20, oxygen saturation 97% on room air, and temperature 36.8 °C. Her blood glucose was 186 mg/dL. • Physical examination revealed no abnormalities and the airway was assessed as a Mallampati class II. • After a smooth induction of general anesthesia with midazolam, fentanyl, propofol, and rocuronium, a #7.0 endotracheal tube was placed atraumatically. Anesthesia was maintained with mechanical ventilation, isoflurane, oxygen, air, fentanyl boluses, and rocuronium • About 30 minutes after the incision, the patient’s HR increased to 112 beats/minute and her BP became 184/99 mm Hg. The anesthesiologist also noticed a depression of the ST segment in the monitored V5 cardiac lead. Questions What would you do? What treatment would you give? Could this event have been prevented? Would you extubate this patient? What is your plan for the post-operative care of this patient? What would you do? Risk factors in this patient: • • • • 68 years old. Morbid obese (BMI = 45.6) wt: 104kg, height :155cm. Diabetic. Hypertensive on atenolol (pulse rate 88 b/min). Intraoperative events : • Blood pressure 184/99. • Heart rate 112b/min. • Depression of the ST segment in the monitored V5 cardiac lead. (Lead V5 is the most sensitive single lead for intraoperative myocardial ischemia). To be sure of diagnosis: Lead II is the best compliment to lead V5 because it significantly improves the sensitivity for ischemia. Reliable automated ST segment analysis has arrived and been incorporated into many monitors. 12 lead ECG Cardiac enzymes. TEE.: To see SWMA. Management • As myocardial ischemia can be a inappropriate anesthetic management so: manifestation of Evaluate the adequacy of ventilation, oxygenation, and anesthetic depth. Control of hemodynamics. Antianginal agents. Finally institution of invasive measures such as; intra- aortic balloon counter-pulsation or angioplasty. Control of Hemodynamics & Anti-anginal Agents Management of Heart Rate Takes Priority. • Increases in heart rate not only increase myocardial oxygen demand, but also decrease myocardial oxygen supply because the duration of diastole is shortened by increases in heart rate and it is during diastole that coronary blood flow occurs Control of Hemodynamics & Anti-anginal Agents • Heart rate can be controlled by addition of a small dose of narcotic such as fentanyl but may also require the use of a β blocker. • Esmolol is a cardioselective β-adrenergic antagonist. It is rapidly metabolized in blood and liver by hydrolysis and has a much shorter duration of action than other available β blockers • Next, IV nitroglycerin Is easily titrated because of its very rapid onset and short duration of action. It produces marked venodilation with limited arterial dilation. • Thus, left ventricular filling volume and pressure are usually reduced to a much greater degree than arterial blood pressure. • Obviously, this is of a substantial advantage in enhancing effective coronary perfusion pressure.In addition, nitroglycerin dilates larger coronary arteries and even the residual lumen within coronary constrictions. • Because of these facts, IV nitroglycerin is usually the first pharmacologic agent chosen for control of intraoperative myocardial ischemia after basic anesthetic management hemodynamics have been optimized. and Institution of Invasive Measures • If myocardial ischemia still persists or is accompanied by left ventricular failure, we will request the placement of an intra-aortic balloon pump, coronary angioplasty, and/or coronary thrombolysis. • An interventional cardiologist will be needed for such endeavors, but failure to treat persistent myocardial ischemia or delay in its treatment may result in unnecessary loss of myocardium, cardiac reserve, or viable cardiac function Could this event have been prevented? • Yes, this event might have been prevented by adequate preoperative preparation. ACC/AHA guidelines for the sample case a. Intermediate risk surgery b. Minor clinical risk secondary to her uncontrolled hypertension These guideline require no further cardiac work-up unless patient had symptoms of cardiac ischemia (i.e., chest pain). Perioperative Cardiac Risk Reduction Therapy What is your plan for the post-operative care of this patient? 1. Hemodynamically stable a. Resolution of patient’s ST-depression b. Extubate i. Closely monitor the patient and treat any hypertension and tachycardia. ii. Be prepared to abort the extubation if the patient develops ST-changes. c. Maintain hemodynamics. d. Send the patient to a cardiac-monitored floor. e. Cardiology consult 2. Hemodyanmically unstable a. Keep intubated. b. Coronary care unit (CCU) c. Cardiology consult ICU admission • Factors that may increase the likelihood of postoperative myocardial ischemia that we can control include tachycardia, anemia, hypothermia, shivering, hypoxemia, endotracheal suctioning, and less-than-optimal analgesia. Coronary angioplasty: • Immediate coronary angioplasty has been favorably compared with thrombolytic therapy in the treatment of acute MI, but of greater importance is that the risk of bleeding at the surgical site is believed to be less with direct angioplasty than with thrombolytic therapy. •In addition, these reperfusion procedures should not be performed routinely on an emergency basis in postoperative patients in whom MI is not related to an acute coronary occlusion. •For instance, in cases of increased myocardial demand in a patient with postoperative tachycardia or hypertension, lowering the heart rate or blood pressure is likely to be of greater benefit, and certainly less risk. MEDICAL TREATMENT: Therapy with aspirin, a beta blocker, and an ACE inhibitor, particularly for patients with low ejection fractions or anterior infarctions, may be beneficial, whether or not the patients are rapidly taken to the catheterization laboratory. Although not intended specifically for patients who have a postoperative MI, they are nonetheless appropriate for these high-risk patients