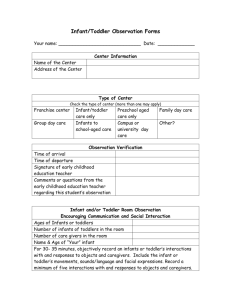
the Child
advertisement

PEDIATRIC NURSING Care of the Child and Family 1 Developmental Theorists Maslow’s Hierarchy of Needs (1954) Erik Erikson - Psychosocial Theory Jean Piaget - Cognitive Theory 2 Maslow’s Hierarchy of Needs Principles: An individual’s needs are depicted in ascending levels on the hierarchy Needs at one level must be met before one can focus on a higher level need Levels of Maslow’s Hierarchy of Needs: Physiologic/Survival Needs Safety and Security Needs Affection or Belonging Needs Self-esteem/Respect Needs Self-actualization Needs 3 TRUST VS. MISTRUST • Birth - 1 year – World/Self is good – Basic needs met • Met = happy baby • Unmet = crying, tense, clinging • Stranger Anxiety • Separation Anxiety Photo Source: Del Mar Image Library; Used with permission 5 AUTONOMY VS. SHAME & DOUBT 1 – 3 years – Sense of control – Exerts self/will – Pride in self-accomplishment • Negativism • Ritualism/Routines • Parallel play Photo Source: Del Mar Image Library; Used with permission 6 INITIATIVE VS. GUILT 3 – 6 years – “Can-do” attitude – Behavior is goal-directed and imaginative – Play is work – Be careful with criticism Photo Source: Del Mar Image Library; Used with permission 7 INDUSTRY VS. INFERIORITY 6 – 12 years – Mastery of skills – Peers in both play and work – Rules important – Competition – Predictability Photo Source: Del Mar Image Library; Used with permission 8 IDENTITY VS. ROLE CONFUSION 12 -18 years – Sense of “I” – Peers are very important – Independence from parents – Self-image Photo Source: Del Mar Image Library; Used with permission 9 Piaget’s Cognitive Theory Development of Thought Processes: 30 – 2 years: Sensorimotor 32 – 7 years: Preoperational 37 – 11 years: Concrete Operations 311 years + : Formal Operations 10 SENSORIMOTOR Birth - 2 years – Reflexive behavior leads to intentional behavior – Egocentric view of world – Cognitive parallels motor development – Object Permanence 11 PREOPERATIONAL THOUGHT 2 - 7 years – – – – – – Egocentric thinking Magical thinking Dominated by self-perception Animism No irreversibility Thoughts cause actions Photo Source: Del Mar Image Library; Used with permission 12 CONCRETE OPERATIONS 7 - 11 years – – – – – – – Systematic/logical Fact from fantasy Sense of time Problem solve Reversibility Cause & effect Humor Photo Source: Del Mar Image Library; Used with permission 13 FORMAL OPERATIONS 11 years - Adult – – – – Abstract thinking Analyze situations New ideas created Factors altering this: • Poor comprehension • Lack of education • Substance abuse Photo Source: Del Mar Image Library; Used with permission 14 Infant Physical Tasks Physical Tasks: 0 - 6 months: Fastest growth period Gains 5-7 oz (142-198 g) weekly for 6 months Grows 1 inch (2.5 cm) monthly for 6 months Head circumference is equal to or larger than chest circumference Posterior fontanel closes at 2-3 months* Obligate nose breathers* Vital signs: HR and RR faster and irregular* Motor: behavior is reflex controlled sits with or without support at 6 mo* rolls from abdomen to back Sensory: able to differentiate between light and dark hearing and touch well developed TOYS = Mirror, Music, Mobile 15 Infant Physical Tasks Physical Tasks 6 - 12 months: Gains 3-5 oz (84-140g) weekly for next 6 months * triples weight by 12 months Gains 1/2 in (1.25 cm) monthly for next 6 months Teeth begin to come in Motor: Intentional rolling over from back to abdomen* Starts crawling and pulling to a stand* Develops pincer grasp* Sits without support by 9 months* Sensory: Can fixate on and follow objects Localizes sounds 16 Infant Psychosocial Tasks Vocalizations: • • • • • Distinction in cry at 1 month Coos at 3 months Begins to imitate sound at 6 months – babbles Verbalizes all vowels at 9 months Can say 4–5 words at 12 months Socialization: • • • • Social smile at 2 months Demands attention & social interaction at 4 months Stranger anxiety & comfort habits begin at 6 months* Separation anxiety develops at 9 months* Photo Source: Del Mar Image Library; Used with permission 17 Infant Cognitive Tasks Neonates Reflexes only 1-4 months Recognizes faces Smiles and shows pleasure Discovers own body and surroundings 5-6 months Begins to imitate 7-9 months Searches for dropped objects *Object Permanence begins Responds to simple commands Responds to adult anger 10-12 months Recognizes objects by name Looks at and follows pictures in books 18 Physical Tasks: • • • • • • • Toddler Slow growth period Gains 11 lbs (5 kg) Grows 8 inches (20.3 cm) Anterior fontanel closes at 12 - 18 months* Primary dentition (20 teeth) complete by 2½ years Develops sphincter control – toilet training possible* Motor Tasks: • • • Walks alone by 12 - 18 months* Climbs and runs fairly well by 2 years Rides tricycle well by 3 years Photo Source: Del Mar Image Library; Used with permission 19 Toddler Cognitive Tasks Follows simple directions by 2 years Uses short sentences by 18 months *favorite words “no” and “mine” = Autonomy Knows own name by 12 months, refers to self Achieves object permanence Uses “magical” thinking Uses ritualistic behavior Repeats skills to master them and decrease anxiety Egocentric thinking - thoughts cause actions 20 Toddler Psychosocial Tasks Increases independence Able to help with dressing self Temper tantrums (autonomy) Beginning awareness of ownership (me and mine) Shares possessions by 3 years Vocabulary increases to over 900 words Toilet training Fears: separation anxiety, loss of control TOYS = Push-pull toys, large blocks 21 Preschooler Physical Tasks: • • • • Slow growth rate continues Weight increases 4-6 lbs (1.8–2.7 kg) a year Height increases 2½ inches (5-6.25 cm) a year Permanent teeth appear Motor Tasks: • • • • • • Walks up & down stairs Skips and hops on alternate feet Throws and catches ball, jumps rope Hand dominance appears Ties shoes and handles scissors well Builds tower of blocks Photo Source: Del Mar Image Library; Used with permission 22 Preschooler Cognitive Tasks Can only focus on one idea at a time Begins awareness of racial and sexual differences Develops an understanding of time • Learns sequence of daily events • Able to understand some time-oriented words Begins to understand the concept of causality Has 2,000 word vocabulary Is very inquisitive and curious 23 Preschooler Psychosocial Tasks Becomes independent Gender-specific behavior is evident by 5 years Egocentricity changes to awareness of others Understands sharing Aggressiveness and impatience peak at 4 years Eager to please and shows more manners by 5 years Behavior is goal-directed and imaginative Play is work* TOYS = Dolls, Dress-up, Imagination 24 Preschooler Psychosocial Tasks Fears: about body integrity (Fear & Injury) are common Magical and animistic thinking allows illogical fears to develop* Observing injuries or pain of others can precipitate fear Able to imagine an event without experiencing it Guilt and shame are common* 25 School-age Physical Tasks: Slow growth continues Weight doubles over this period Gains 2 inches (5 cm) per year At age 9, both sexes are the same size At age 12, girls are bigger than boys Very limber but susceptible to bone fractures Develops smoothness & speed in fine motor skills Energetic, developing large muscle coordination, stamina & strength Has all permanent teeth by age 12 Photo Source: Del Mar Image Library; Used with permission 26 School-Age Cognitive Tasks Period of Industry: • Likes to accomplish or produce • Interested in exploration & adventure • Develops confidence • Rules become important* Concepts of time and space develop: • Understands causality, permanence of mass & volume • Masters the concepts of conservation, reversibility, arithmetic and reading • Develops classification skills • Begins to understand cause and effect* 27 School-Age Psychosocial Tasks School occupies half of waking hours; has cognitive and social impact on child Morality develops Peer relationships start to be developed Enjoys family activities Has increased self-direction - tasks are important Has some ability to evaluate own strengths & weaknesses Enjoys organizational activities (sports, scouts, etc.)* Modesty develops as child becomes aware of own body* TOYS = Board games, computer games, learning activities 28 Adolescent Physical tasks: Period of rapid growth Puberty starts Girls: height increases 3 inches/year Boys: growth spurt around 13-yrs-old height increases 4 inches/year weight doubles between 12-18 yrs Body shape changes: Girls have fat deposits in thighs, hips & breast, pelvis broadens Boys become leaner with a broader chest Photo Source: Del Mar Image Library; Used with permission 29 Adolescent Sexual Development Girls Boys Breasts develop Facial Hair growth Menses begins Voice changes First 1 –2 years infertile Enlargement of testes at 13 yrs Nocturnal emission during sleep Reaches reproductive maturity with viable sperm at 17 yrs 30 Adolescent Cognitive Tasks Develops abstract thinking abilities Often unrealistic Sense of invincibility = risk taking behavior* Capable of scientific reasoning and formal logic Enjoys intellectual abilities Able to view problems comprehensively ACTIVITIES = Music, video games, communication with peers 31 Adolescent Psychosocial Tasks Early Adolescent: Prone to mood swings Needs limits and consistent discipline Changes in body alter self-concept Fantasy life, daydreams, crushes are normal Middle Adolescent: Separate from parents Identify own values and define self* Partakes/conforms to peer group/values* Increased sexual interest May form a “love” relationship Formal sex education begins 32 Adolescent Psychosocial Tasks Late Adolescent: Achieves greater independence* Chooses a vocation Finds an identity* Finds a mate Develops own morality Completes physical and emotional maturity Fears: Threats to body image – acne, obesity Rejection Injury or death, but have sense of “invincibility” The unknown 33 Let’s Review A 10 month-old baby was admitted to the pediatric unit. Each time the nurse enters the room the baby begins to cry. The most appropriate action by the nurse would be to: A. Complete all procedures quickly in order to decrease the amount of time the baby will cry. B. Ask another nurse to assist you with the baby’s care. C. Distract the baby. D. Encourage the parent to stay by the bedside and assist with the care. 34 Let’s Review A 6 month-old is admitted to the pediatric unit for a 3 week course of treatment. The infant’s parents cannot visit except on weekends. Which action by the nurse indicates an understanding of the emotional needs of an infant? A. Telling the parents that frequent visits are unnecessary. B. Placing the infant in a room away from other children. C. Assigning the infant to different nurses for varied contacts. D. Assigning the infant to the same nurse as much as possible. 35 Let’s Review Which child is most likely to be frightened by hospitalization? A. 4 month-old admitted with a diagnosis of bronchiolitis. B. 2 year-old admitted with a diagnosis of cystic fibrosis. C. 9 year-old admitted with a diagnosis of abdominal pain. D. 15 year-old admitted with a diagnosis of a fractured femur. 36 Infant Nutrition Birth – 6 months: Breast milk is most complete diet Iron-fortified formulas are acceptable No solid foods before 4 months* 6 - 12 months: Breast milk or formula continues* Diluted juices can be introduced Introduction of solid foods*(4-6 mo): cereal, vegetables, fruits, meats Finger foods at 9-10 months Chopped table foods at 12 months Gradual weaning from bottle/breast No honey (risk for botulism) 37 Toddler Nutrition Able to feed self – autonomy & messy! Appetite decreases- physiologic anorexia Negativism may interfere with eating Needs 16 – 20 oz. milk/day Increased need for calcium, iron, and phosphorus – risk for iron deficiency anemia Caloric requirements is 100 calories/kg/day No peanuts under 3 years of age (allergies)* Do not restrict fats less than 2 years of age* Choking is a hazard (no nuts, hot dogs, popcorn, grapes)* Photo Source: Del Mar Image Library; Used with permission 38 Preschooler Nutrition Caloric requirements is 90 calories/kg/day May demonstrate strong taste preferences • 4 years old – picky eaters • 5 years old – influenced by food habits of others Able to start social side of eating More likely to try new foods if they assist in food preparation Establish good eating habits - obesity 39 School-Age Nutrition Caloric needs diminish, only need 85 kcal/kg Foundation laid for increased growth needs Likes and dislikes are well established “Junk” food becomes a problem Busy schedules – breakfast is important Obesity continues to be a risk Nutrition education should be integrated into the school program 40 Adolescent Nutrition Nutritional requirements peak during years of maximum growth: Age 10 – 12 in girls Age 14 – 16 in boys Food intake needs to be balanced with energy expenditures Increased needs for: Calcium for skeletal growth Iron for increased muscle mass and blood cell development Zinc for development of skeletal, muscle tissue and sexual maturation Photo Source: Del Mar Image Library; Used with permission 41 Adolescent Nutrition (continued) Eating and attitudes towards food are primarily family/peer centered Skipping breakfast, increased junk food, decreased fruits, veggies, milk Boys eat foods high in calories. Girls under-eat or have inadequate nutrient intake. 42 Let’s Review The nurse recommends to parents that popcorn and peanuts are not good snacks for toddlers. The nurse’s rationale for this action is: A. B. C. D. They are low in nutritive value. They cannot be entirely digested. They can be easily aspirated. They are high in sodium. 43 Let’s Review Nutrition is an important aspect of health promotion for the infant. Priority information to give the parents concerning infant nutrition would include (check all that apply): A. Restrict the fat intake of the infant to help reduce the chances of an obese child. B. Breast or infant formula must be continued for the first year. C. Encourage the use of a pacifier for non-nutritive sucking needs. D. Introduction of solid foods should begin at 4-6 months. 44 Play is the work of Children Enhances Motor Skills Enhances Social Skills Enhances Verbal Skills Expresses Creativity Decreases Stress Helps Solve Problems 45 Appropriate Play Activities Infants - Solitary Play, stimulation of senses (music, mirror) Toddler - Parallel Play, make believe, locomotion (push-pull toys), gross & fine motor, outlet for aggression & autonomy Preschooler - Associative Play, Imaginary Playmate, dramatic & imitative, gross & fine motor School Age - Cooperative Play, rules dominate play, team games/sports, quiet games/activities, joke books Adolescent - Group activities predominate, activities involving the opposite sex in later years 46 Preparation for Procedures • Allow child to play with equipment • Demonstrate procedure on doll for young child • Use age-appropriate teaching activities • Describe expected sensations • Use simple explanations • Clarify any misconceptions • Involve parents in comforting child • Praise/reward child when finished Photo Source: Del Mar Image Library; Used with permission 47 Communicating with Children Provide a trusting environment Get down to child’s eye level Use words appropriate for age Always explain what you are doing Always be honest Allow choices when possible Allow child to show feelings/talk 48 Let’s Review The single most important factor for the nurse to recognize when communicating with a child is: A. B. C. D. The child’s chronological age. Presence or absence of the child’s parents. Developmental level of the child. Nonverbal behaviors of the child. 49 Health Promotion Childhood Immunizations Well child check-ups Nutrition Screenings throughout childhood (APGARS, newborn screenings, lead poisoning, vision/hearing, scoliosis) Health Teaching 50 Immunizations Primary prevention of many communicable diseases Vaccines safety • MMR vaccine and autism (no correlation) • Reactions (pre-medicate with Tylenol) Live attenuated vaccines (MMR, Varicella) • Weakened form of disease • Body produces immune response • Contraindicated in immunosupressed individuals Inactivated (killed virus/bacteria or synthetic) • 1st dose only “primes” system- immunity develops after 3rd 51 Injury Prevention & Safety Issues Accidents are the leading cause of death in infants and toddlers (falls, burns, poisons) Toddlers and Preschoolers – drowning School-age and adolescents – motor vehicle accidents and firearms 90% of all accidents are preventable! Safety education is the answer 52 Injury Prevention Methods of Injury Prevention • Understanding and Applying Growth and Developmental Principles • Anticipatory Guidance • Childproofing the environment • Educating caregivers and children • Legislation Precipitating Factors Potential Outcomes 53 Pediatric Poisonings Highest incidence occurs in children in 2-year-old age group and under 6 years of age Major contributing factor – improper storage, allowing children to play with “bottles” – rattling of pills, “drink” syrups, toxic portion of plants. Teach parents about proper storage Knowledge of plants in household, and keep away from infants and children who might “chew” Emergency treatment depends on agent ingested Teach parents to have poison control number available Refer to appropriate method according to substance ingested First Intervention is to call POISON CONTROL CENTER 54 Types of Poisonings Lead Poisoning Salicylate Poisoning Acetaminophen Ingestion 55 Lead Poisoning Major environmental health concern Found in older homes (built before 1978), leadcontaminated soil, water through lead pipes, lead-based paint in ceramics products, Mexican candies made in lead containers Body rapidly absorbs lead – specially in periods of rapid growth – most harmful to children under 6 years Absorbed in GI tract and accumulates in bones, brain, kidneys Low levels in blood can cause behavioral/learning problems, mid-levels anemia-like symptoms and skeletal growth interference, and high levels can be fatal from CNS edema and encephalopathy Diet high in fat, low in iron & calcium can increase lead absorption Intervention=teaching for prevention. If blood level ≥ 45, chelation therapy is needed – monitor kidney function during treatment. 56 Salicylate Poisoning Can be acute or chronic ingestion S/S = nausea, disorientation, vomiting, dehydration, hyperpyrexia, oliguria, coma, bleeding tendencies, tinnitus, seizures Nursing interventions = activated charcoal, sodium bicarbonate for metabolic acidosis, external cooling measures for hyperpyrexia, anticonvulsant and seizure precautions (think patient safety!), vitamin K for bleeding, possible hemo (NOT peritoneal) dialysis 57 Acetaminophen Poisoning Most common drug poisoning in children Acute ingestion S/S start as nausea, vomiting, pallor, sweating » hepatic involvement (jaundice, confusion, coagulation problems, RUQ pain) Treatment is activated charcoal first, then the antidote N-acetylcysteine (Mucomyst) PO every 4 hours for 17 doses after a loading dose given Always assess Level of Consciousness (LOC) before administering PO med! 58 Let’s Review Which would be the best approach for gastric emptying in a lethargic 18-month-old who ingested antihistamine tablets an hour ago? A. B. C. D. Diluting toxic substance with water or milk Administering naloxone (Narcan) Gastric lavage Administering ipecac syrup 59 Physical Assessment of Infant Assessment is NOT in the head-to-toe manner When quiet, auscultate heart, lungs, abdomen Assess heart & respiratory rates before temperature Palpate and percuss same areas Perform traumatic procedures last Elicit reflexes as body part examined Elicit Moro reflex last Encourage caretaker to hold infant during exam Distract with soft voice, offer pacifier, music or toy 60 Physical Assessment of Toddler Inspect body areas through play – “count fingers and toes” Allow toddler to handle equipment during assessment and distract with toys and bubbles Use minimal physical contact initially Perform traumatic procedures last Introduce equipment slowly Auscultate, percuss, palpate when quiet Give choices whenever possible Photo Source: Del Mar Image Library; Used with permission 61 Physical Assessment of Preschooler If cooperative, proceed with head-to-toe If uncooperative, proceed as with toddler Request self undressing and allow to wear underpants Allow child to handle equipment used in assessment Don’t forget “magical thinking” Make up “story” about steps of the procedure Give choices when possible If proceed as game, will gain cooperation Photo Source: Del Mar Image Library; Used with permission 62 Physical Assessment of School-Age Child Proceed in head-to-toe May examine genitalia last in older children Respect need for privacy – remember modesty! Explain purpose of equipment and significance Teach about body function and care of body 63 Physical Assessment of the Adolescent Ask adolescent if he/she would like parent/caretaker present during interview/assessment Provide privacy Head-to-toe assessment appropriate Incorporate questions/assessment related to genitals/sexuality in middle of exam Answer questions in a straightforward, noncondescending manner Include the adolescent in planning their care 64 Fever Causes – Often unknown, may be due to dehydration, most often viral induced Danger in infants is febrile seizures – most common between 3 months to five years. The seizure is a result of how quickly the temperature rises. Hydration (20mls/kg is formula for bolus) Antipyretics – acetaminophen or ibuprofen Cooling measures – avoid shivering • Tepid bath • Remove excess clothing and blankets • Cooling blankets/mattresses NO ICE PACKS! 65 Pediatric Differences Fluid & Electrolyte Percent Body Water compared to Total Body Weight: • Premature infants: 90% water • Infants: 75 - 80% water • Child: 64% water Higher percentage of water in extracellular fluid in infants Infants and toddlers more vulnerable to fluid and electrolyte disturbances Concentrating abilities of kidneys not fully mature until 2 years Metabolic rate is 2-3 times higher than an adult Greater body surface area per kg body weight than adults; dehydrates more quickly 66 Dehydration • Types: Isotonic – Most common; salt and water lost. Greatest threat – Hypovolemic Shock Hypotonic – Electrolyte deficit exceeds water deficitphysical signs more severe with smaller fluid losses Hypertonic – Water loss higher than electrolyte Vomiting leads to metabolic alkalosis Diarrhea leads to metabolic acidosis LAB WATCH: monitor sodium, potassium, chloride, carbon dioxide, BUN, and creatinine 67 Assessment of Dehydration • • • • • • • Skin gray, cold, mottled, poor to fair, dry or clammy Delayed capillary refill Mucous membranes/lips dry Eyes and fontanels sunken No tears present when crying Pulse and respirations rapid Irritability to lethargy depending on cause and severity, not responsive to parent and/or environment 68 Dehydration: Nursing Interventions Daily weight, I/O Assess hydration status Assess neurological status Monitor labs (electrolytes) Rehydrate with fluids both PO and IV (20 mls/kg of NS) Diet progression: Pedialyte modified Bread-RiceApple Juice-Toast (BRAT) Diet-for-age (DFA) Skin care for diaper rash Stool output (Amount, Color, Consistency, Texture ACCT) HANDWASHING! Priorities: fluid replacement & assess for S/S of69 shock Diarrhea • Often specific etiology unknown, but rotavirus is most common cause of gastroenteritis in infants and kids • Don’t forget contact precautions!! • Leading cause of illness in children younger than 5 • May result in fatality if not treated properly • History very important • Treatment aimed at correcting fluid imbalance and treating underlying cause • Metabolic acidosis = blood pH < 7.35 70 Vomiting • Often result of infections, improper feeding techniques, GI blockage (pyloric stenosis), emotional factors • Management directed toward detection, treatment of cause and prevention of complications • Metabolic alkalosis = blood pH >7.45 71 Let’s Review The most appropriate type of IV fluid to infuse in treatment of extra-cellular dehydration in children is: A. B. C. D. Isotonic solution. Hypotonic solution. Hypertonic solution. Colloid solution. 72 Let’s Review Which laboratory finding would help to identify that a child experiencing metabolic acidosis? A. B. C. D. Serum potassium of 3.8 Arterial pH of 7.32 Serum carbon dioxide of 24 Serum sodium of 136 73 Pain Assessment: Infants Assessment of pain includes the use of pain scales that usually evaluate indicators of pain such as cry, breathing patterns, facial expressions, position of extremities, and state of alertness Examples: FLACC scale, NIPS scale 74 Pain Assessment: Toddlers Toddlers may have a word that is used for pain (“owie,” “booboo,” “ouch” or “no”); be sure to use term that toddler is familiar with when assessing. Can also use FLACC scale, or Oucher scale (for older toddlers) 75 Pain Assessment: Preschoolers Think pain will magically go away May deny pain to avoid medicine/injections Able to describe location and intensity of pain FACES scale, poker chips and Oucher scale may be used Photo Source: Del Mar Image Library; Used with permission 76 Pain Assessment: Older Children Older children can describe pain with location and intensity Nonverbal cues important, may become quiet or withdrawn Can use scales like Wong’s FACES scale, poker chips, visual analog scales, and numeric rating scales 77 Let’s Review The nurse begins a full assessment on a 10 yearold patient. To ensure full cooperation from this patient it is most important for the nurse to: A. Approach the assessment as a game to play. B. Provide privacy for the patient. C. Encourage the friend visiting to stay at the bedside to observe. D. Instruct the child to assist the nurse in the assessment. 78 Let’s Review During a routine health care visit a parent asks the nurse why her 10 month-old infant is not walking as her older child did at the same age. Which response by the nurse best demonstrates an understanding of child development? A. “Babies progress at different rates. Your infant’s development is within normal limits.” B. “If she is pulling up, you can help her by holding her hand.” C. “She’s a little behind in her physical milestones.” D. “You can strengthen her leg muscles with special exercises to make her stronger.” 79 Let’s Review When assessing a toddler identify the order in which you would complete the assessment: 1. 2. 3. 4. Ear exam with otoscope Vital signs Lung assessment Abdominal assessment 80 Let’s Review When assessing pain in an infant it would be inappropriate to assess for: A. B. C. D. Facial expressions Localization of pain Crying Extremity movement 81 Genetic Disorders 7 Principles of Inheritance g Autosomal Dominant g Autosomal Recessive g Sex-linked (X-linked) Inheritance g Chromosome Alterations 7Down’s Syndrome 7Tay-Sachs Disease Nursing intervention is supporting parents and resources 82 Down’s Syndrome • Most common cause of cognitive impairment (moderate to severe) • 1 in 600 live births • Risk factor- pregnancy in women over 35 yrs old • Cause - extra chromosome 21 (faulty cell division) • Causes change in normal embryogenesis process resulting in: Cardiac defects, GI conditions, Endocrine disorders, Hematologic abnormalities, Dermatologic changes • Physical features: small head, flat facial profile, broad flat nose, small mouth, protruding tongue, low set ears, transverse palmar creases, hypotonia * Feeding is often a problem in infancy * 83 Tay-Sachs Disease Occurs predominately in children of Eastern European Jewish ancestry Fatal Disease - death usually occurs before age 4 Autosomal recessive inheritance Degenerative brain disease Caused by absence of hexosainidase A from body tissue Symptoms: progressive lethargy in previously healthy 2-6 months old infants, loss of milestones, visual acuity, seizures, hyper-reflexia, posturing, malnutrition, dysphagia Diagnosis: Classic cherry red spot on macula, enzyme measurement in serum, amniotic fluid, white cells 84 Let’s Review The infant with Down’s Syndrome is closely monitored during the first year of life for which condition? A. B. C. D. Thyroid complications Orthopedic malformations Cardiac abnormalities Dental malformations 85 Pediatric Differences Neurosensory System Size and Structure: Rapid head growth in early childhood Bones are not fused until 18-24 months Function: Autonomic Nervous System is intact - neurons are completely myelinized by 1 year Infants behavior initially reflexive, but are replaced with purposeful movement by 1 year Infants demonstrate a dominance of flexor muscles Motor development occurs constantly in head to toe progression 86 Pediatric Differences Neurosensory System Eye and Vision: Changes in development of eye and eye muscles *strabismus normal until 6 months Vision function becomes more organized Papilledema rarely occurs in infants due to expansion of fontanels with increased ICP Ear and Hearing: Hearing fully developed at birth Abnormal physical structures may indicate genetic problems 87 The Neurosensory System Disorders of the Nervous System 3 3 3 3 3 3 Hydrocephalus Spina Bifida Reyes Syndrome Seizures Cerebral Palsy (CP) Meningitis 88 Hydrocephalus • Develops as a result of an imbalance of production and absorption of CSF • The increase of CSF causes increased ventricular pressure, leading to dilation of the ventricles, pressing on skull • Signs/Symptoms of Increased ICP: • Poor feeding and vomiting • Bulging fontanel, head enlargement, separation of sutures • Lethargy, irritability, restlessness, not responsive to parents • CHILD - Headache, vomiting, diplopia, ataxia, papilledema • Seizures A child’s head with an open fontanel (under 2 years old) has the ability to expand and better compensate for the increased intracranial pressure. 89 Ventriculoperitoneal (VP) Shunts • Relief of hydrocephalus • Prevention/treatment of complications • Management of problems related to psychomotor development • Surgical intervention: ventriculoperitoneal (VP) shunt • One-way pressure valve releasing CSF into peritoneal cavity where it is reabsorbed Photo Source: Del Mar Image Library; Used with permission 90 General Nursing Interventions • Monitor Neuro Status Determine baseline Assess LOC Assess motosensory Pupil checks Vital signs, Head circ • Provide Patient Safety Seizure precautions Fall precautions Possible restraints Determine LOC ac • Decrease ICP Cluster care/ stress Quiet environment HOB 30-45 degrees Appropriate position (head midline, no hip flexion, no prone) Medications(pain meds,corticosteroids, diuretics, stool softeners, antiinfectives, anticonvulsants) 91 General Nursing Interventions • Maintain Adequate Cerebral Perfusion Maintain airway Monitor oxygenation and apply O2 PRN Monitor temperature and administer antipyretics PRN Maintain normovolemia Monitor I/O Assess perfusion • Maintain Nutritional & Fluid Needs Determine swallow ability prior to PO’s NGT feedings may be necessary Dietary consult PRN Daily weight Monitor lab results • Psychosocial Support Child Life consult Teaching 92 Spina Bifida: Occulta and Cystica (meningocele and myelomeningocele) Photo Source: Del Mar Image Library; Used with permission • Etilogy is unknown, but genetic & environmental factors considered. – Maternal intake of folic acid – Exposure of fetus to teratogenic drugs • The severity of clinical manifestations depend on the location of the lesion. – T12 - flaccid lower extremities, sensation, lack of bowel control and dribbling urine – S 3 and lower - no motor impairment • Other complications may occur. – Hydrocephalus (80-90%) – Orthopedic issues such as scoliosis, kyphosis, club foot – Urinary retention – Skin breakdown/Trauma 93 Spina Bifida Nursing Interventions • • • • • • • • Sterile dressing pre/post-op Monitor VS, S/S infection Use latex free items Avoid stress on sac - prone position only, especially pre-op; no supine until incision healed Monitor for S/S intracranial pressure (ICP) Interventions to ICP Encourage touch & talk Social service consult 94 Reye’s Syndrome • A true pediatric emergency - cerebral complications may reach an irreversible state. Vomiting & change in LOC to coma • Acute encephalopathy with fatty degeneration of the liver causing fluid & electrolyte imbalances, metabolic acidosis, hypoglycemia, dehydration, and coagulopathies. • Most frequently seen in children recovering from a viral illness during which salicylates were given. • Therapeutic management is intensive nursing care and maintaining adequate cerebral perfusion, &↓ICP. Increased ICP secondary to cerebral edema is major contributing factor to morbidity and mortality. 95 Seizures • Febrile seizures are the most common in children, caused by by a RAPID elevation in temperature, usually above 102°. • Most children do not have a second febrile seizure episode and only about 3% develop epilepsy. • Focus of care is on patient safety, cause of fever and education of parents for home care. • Remember basic CPR during seizures – airway before oxygen • Seizure precautions: Suction, oxygen, padded rails • Infants often have subtle seizures with only occular movements or some extremity movements. 96 Cerebral Palsy (CP) 1.5 - 5 in 1,000 live births Neuromuscular disorder resulting from damage or altered structure of part of the brain Caused by a variety of factors: • Prenatally - genetic, trauma, anoxia • Perinatally - fetal distress, drugs at delivery, precepitate or breech delivery with delay • Postnatally - kernicterus or head trauma 97 Cerebral Palsy (continued) Spasticity - exaggerated hyperactive reflexes Athetosis - constant involuntary, purposeless, slow writhing motions Ataxia - disturbances in equilibrium Tremor - repetitive rhythmic involuntary contractions of flexor and extensor muscles Rigidity - resistance to flexion and extension Associated Problems: Mental retardation, hearing loss, speech defect, dental & orthopedic anomalies, GI problems and visual changes 98 Cerebral Palsy: Nursing Interventions • Safety Feed in upright position Seizure precautions Ambulate with assistance if able Medication administration • Special Needs Nutritional needs include increased calories, assist with feeds, possible GT feeds. Speech, Occupational and Physical therapies 99 Bacterial Meningitis • Infectious process of CNS causing inflammation of meninges and spinal cord. • ISOLATION IS MANDATORY • Signs and symptoms include those of increased ICP plus photophobia, nuchal rigidity, joint pain, malaise, purpura rash, Kernig’s and Brudinski’s signs • Can occur at any age, but often between 1 month-5 years • Most common sequele: hearing and/or visual impairments, seizures, cognitive changes • Diagnostic confirmation is done by lumbar puncture and CSF is cloudy with increased WBCs, increased protein, and low glucose • Nursing Interventions include: appropriate IV antibiotics and meds for increased ICP as well as interventions to decrease ICP 100 Causes of Blindness Genetic Disorders: Tay-Sach’s disease Inborn errors of metabolism Perinatal: prematurity, retrolental fibroplasia Postnatal: trauma, childhood infections, Juvenile Arthritis 101 Causes of Deafness Conductive: Interference in transmission from outer ear to middle ear from chronic OM Sensorineural: Dysfunction of the inner ear Damage to cranial nerve VIII from rubella, meningitis or drugs 102 Let’s Review Which test would confirm a diagnosis of meningitis in children? A. B. C. D. Complete blood count Bone marrow biopsy Lumbar puncture Computerized Tomography (CT) scan 103 Let’s Review In performing a neurological assessment on a patient which data would be most important to obtain? A. B. C. D. Vital signs. Head circumference. Neurologic “soft signs”. Level of consciousness (LOC). 104 Let’s Review A neonate born with myelomeningocele should be maintained in which position pre-operatively? A. B. C. D. Prone. Supine. Trendelenberg. Semi-Fowler. 105 Let’s Review The nurse witnesses a pediatric patient experiencing a seizure. The primary nursing intervention would be: A. Careful observation and documentation of the seizure activity. B. Maintain patient safety. C. Minimize the patient’s anxiety. D. Avoid over stimulation and promote rest. 106 Let’s Review Which assessment finding in an infant first day post-op placement of a ventriculoperitoneal (VP) shunt is indicative of surgical complications? A. B. C. D. Hypoactive bowel sounds. Congestion in upper airways. Increasing lethargy. Incisional pain. 107 Cardiovascular System: Pediatric Variances Cardiac arrest is related to prolonged hypoxemia Heart Rate (HR) higher Cardiac Output depends on HR until heart muscle is fully developed (around 5 years of age) Innocuous (benign) murmurs Sinus arrhythmias normal in infants Congenital defects present at birth – the greater the defect, the more severe the clinical manifestations (S/S) 108 FETAL CIRCULATION Photo Source: Del Mar Image Library; Used with permission 109 Cardiovascular System: Changes from Fetal Circulation Fetal Circulation - Pattern of Altered Blood Flow Normal Circulatory Changes at Birth: Oxygenation takes place in Lungs Structural changes occur: * Ductus venosus constricts by 3-7 days becomes ligamentum venosum * Foramen ovale closes within first weeks * Ductus arteriosus functional closure at 24 hours, anatomic closure 1-3 weeks 110 Cardiovascular System: Changes from Fetal Circulation Abnormal Circulatory Patterns After Birth Abnormal openings between the pulmonary and systemic circulations can disrupt blood flow. ♥Blood will follow the path of least resistance -Left side of heart has greater pressure, so . . . ♥Blood normally shunted from left to right Obstructions to pulmonary blood flow may cause right to left shunting of blood 111 NORMAL HEART ANATOMY BLOOD FLOW Photo Source: Del Mar Image Library; Used with permission 112 The Cardiovascular System Y Care of the Child with Congestive Heart Failure Y Congenital Heart Defects Increased Pulmonary Blood Flow Decreased Pulmonary Blood Flow Obstruction to Systemic Blood Flow Y Acquired Heart Disease 113 Goals of Nursing Care with Congenital Heart Disease Y Reduce workload-Improve cardiac function Y Improve respiratory function Y Maintain nutrition to meet metabolic demands and promote growth Y Prevent infection and support/instruct parents 114 Congestive Heart Failure Review • COMPENSATORY RESPONSES – – – – – – – – – Tachycardia, especially at rest Diaphoresis Fatigue Poor Feeding Failure to Thrive (FTT) Exercise Intolerance Decreased Peripheral Perfusion Pallor and/or Cyanosis Cardiomegaly 115 CLINICAL MANIFESTATIONS-CHF • PULMONARY – – – – – – Tachypnea Dyspnea Wheezes Crackles Retractions Nasal Flaring Cough • SYSTEMIC – Edema (facial) – Sudden weight gain – Decreased Urine Output – Hepatomegaly – Splenomegaly – Jugular Vein Distention (JVD, children) – Ascites 116 CHF: Focused Review Nursing Interventions Therapeutic Management Improve cardiac function – Digitalization; Infant dose calculated 1000micrograms=1mg, ACE inhibitors Diuretics, fluid restrictions, daily weights, I/O Decrease tissue demands – Promote rest, minimize stress Increase tissue oxygenation – Oxygen Nutrition – Nipple feeds vs. gavage or GT, highercalorie feeds 117 GENERAL NURSING INTERVENTIONS • Improve Cardiac Function • Decrease Cardiac Demands – Medicate – Promote rest • Cardiac glycosides – Minimize Stress (Digoxin) – Monitor VS (temp) • Promote Fluid Loss • Reduce Respiratory Distress – Medicate – HOB elevated • Furosemide – Possible supplemental • Spironolactone oxygen • Clorothiazide • Maintain Nutrition – Fluid Restriction – Nipple vs. Gavage/GTT – Daily Weight – Higher-calorie feeds (more than 20 cals/oz) – Monitor I/O 118 Increased Pulmonary Blood Flow (Acyanotic) • Atrial Septal Defect (ASD) • Ventricular Septal Defect (VSD) • Patent Ductus Arteriosus (PDA) • CHF • Feeding intolerance • Activity intolerance • Poor growth, failure to thrive • Frequent Pulmonary Infections due to “boggy lungs” 119 Photo Source: Del Mar Image Library; Used with permission 120 Decreased Pulmonary Blood Flow (Cyanotic) • Pulmonary Stenosis • Tetralogy of Fallot • Transposition of the Great Vessels Assessment findings/Compensatory mechanisms • Oxygen desaturation • Varying degrees of cyanosis • Polycythemia 121 Decreased Pulmonary Blood Flow (Cyanotic) Photo Source: Del Mar Image Library; Used with permission 122 Obstruction to Systemic Blood flow • Aortic Stenosis • Coarctation of the Aorta • Think perfusion issues -Diminished or unequal pulses -Poor color -Delayed capillary refill time -Exercise intolerance 123 Obstruction to Systemic Blood flow Photo Source: Del Mar Image Library; Used with permission 124 Rheumatic Fever Acquired Heart Disease Inflammatory disorder involving heart, joints, connective tissue, and the CNS Peaks in school-age children Linked to environmental factors and family history Thought to be an autoimmune disorder: Commonly preceded by a Strep Throat Prognosis depends upon the degree of heart damage Rest important in recovery – priority intervention in acute stage Strep prophylaxis for 5 years or throughout adolescence 125 Hematologic System: Pediatric Variances All bone marrow in a young child is involved in the formation of blood cells. By puberty, only the sternum, ribs, pelvis, vertebrae, skill, and proximal epiphyses of femur and humerus are involved in blood cell formation. During the first 6 months of life, fetal hemoglobin is gradually replaced by adult hemoglobin. 126 The Hematologic System Disorders of Red Blood Cells Iron Deficiency Anemia Sickle Cell Anemia Disorders of Platelets/Clotting Factors Idiopathic Thrombocytopenia Purpura (ITP) Hemophilia 127 IRON DEFICIENCY ANEMIA • Most common nutritional anemia in childhood • Severe depletion of iron stores resulting in a low HGB level • Decreased O2 to tissues = fatigue, headache, pallor, increased heart rate • Occurs after depletion of iron stores in body (6-9 mo of age) • Most likely to occur during rapid physical growth and low iron intake 128 IRON DEFICIENCY ANEMIA • Often occurs as a result of increased milk intake • Lab results show low HGB, HCT, MCV, MCH, MCHC, iron, ferritin • Teach parents proper nutrition • Meat, spinach, legumes, sweet potatoes, egg yolks, seafood • Calcium inhibits iron, Vitamin C enhances iron absorption 129 Sickle Cell Disease PATHOLOGY Photo Source: Del Mar Image Library; Used with permission Normal RBC has a flexible, round shape RBC w/HbS has a normal shape until it’s O2 delivered to tissue, then sickle shape occurs Stiff, non-pliable – can’t flow freely Trapped in small vessels = causes vaso-occlusions, tissue ischemia and infarctions – painful episodes, most common area is joints Hemolysis of RBC- lifespan down to 20 days Compensatory mechanism is increased reticulocytes 130 Sickle Cell Disease ACUTE FEBRILE ILLNESS • High mortality rate <5 years old • Splenic dysfunction begins at 6 mo old • Prophylactic PCN – BID at 2-3 mo old • Monitor for Infection – Temp > 101.5 – Respiratory S/S SPLENIC SEQUESTRATION • Highly vascular • Susceptible to injury/infarction • Occurs 6 mo-3yrs • Pallor, fatigue, abd pain, splenomegaly, CV compromise • Treatment: IV fluids, PRBC’s 131 Sickle Cell Disease: Nursing Interventions GENERAL NURSING CARE • Hydration is Priority! HOME MANAGEMENT • Pain Control – Fluid Bolus & maintenance + • Fluids 1/2 • Teaching • Oxygen - to decrease sickling of • Early Identification of of cells infection • Pain Management • Immunizations – Assess frequently/appropriately • Avoid dehydration – IV Morphine q3-4 hr, PCA – Non-pharmacological methods 132 Idiopathic Thrombocytopenic Purpura (ITP) Acquired hemorrhagic disorder characterized by thrombocytopenia and purpura Cause is unknown, but is to believed to be an auto-immune response to disease-related antigens Usually follows an URI, measles, rubella, mumps, chickenpox Greatest frequency is between 2-8 years of age Platelet count is below 20,000 Therapeutic management is supportive with safety concerns. Activity is usually restricted. Acute presentation therapy can include prednisone, IV immunoglobulin, or Anti-D antibody (causes a hemolytic anemia to rid the body of the antibody-coated RBC’s) Chronic ITP will involve a splenectomy. 133 Hemophilia • Group of genetic bleeding disorders of which there is a deficiency of a clotting factor • Most common are Factor VIII (A) & Factor IX (B) • Bleed LONGER not faster • Clinical manifestations: prolonged bleeding, bruising, spontaneous hematuria • Management: replacement of missing clotting factor (recombinant factor VIII concentrate), cryoprecipitate, DDAVP • NSAIDS (aspirin, Indocin) are contraindicated, they inhibit platelet function • Regular non-contact exercise/physical therapy is encouraged 134 Hemophilia COMPLICATIONS • Bleeding into muscle tissue • Hemarthrosis can cause joint pain & destruction • Acute Treatment is rest, ice, elevation, ROM Photo Source: Del Mar Image Library; Used with permission 135 Let’s Review When assessing a child for any possible cardiac anomalies, the nurse takes the right arm blood pressure (BP) and the BP in one of the legs. She finds that the right arm BP is much greater than that found in the child’s leg. The nurse reacts to these findings in which way? A. B. C. D. Charts the findings and realizes they are normal. Suspects the child may have coarctation of the aorta. Suspects the child may have Tetralogy of Fallot. Notifies the physician and alerts the surgery team. 136 Let’s Review A 1-month-old infant is being admitted for complications related to a diagnosed ventricular septal defect (VSD). Which physician’s order should be questioned by the nurse? A. Blood pressure every 4 hours. B. Serum digoxin level. C. Diet: Enfamil 20, nipple 6 oz q2H. D. Supplemental oxygen via nasal cannula prn maintain SaO2 >92%. 137 Let’s Review A nursing intervention most pertinent for the child with hemophilia is: A. Sedentary activities to prevent bleeding episodes. B. Meticulous oral care with dental floss to prevent infection. C. Warm compresses to bleeding areas to increase absorption. D. Active range of motion exercises for joint mobility. 138 Let’s Review Which is the most appropriate information to teach a parent of a 14 month-old child with iron deficiency anemia? A. Increase the child’s daily milk intake to a minimum of 24 ounces. B. Administer oral iron supplement for the child to drink in a small cup. C. Increase the amount of dark green, leafy vegetables and eggs in the child’s diet. D. Encourage the parents to let the child choose foods he prefers. 139 Let’s Review Which strategy is appropriate when feeding the infant in congestive heart failure? A. Continue the feeding until a sufficient amount of formula is taken B. Bottle feed no longer than 30 minutes C. Feed the infant every 2 hours D. Rock and comfort the infant during feedings 140 Respiratory System Pediatric Variances The airway is smaller and more flexible. The larynx is more flexible and more susceptible to spasm. The lower airways are smaller with underdeveloped cartilage. The tongue is large. Infants < 6 months old are obligate nose breathers. Chest muscles are not well developed The diaphragm is the neonate’s major respiratory muscle. Irregular breathing pattern and brief periods of apnea (10 15 secs) are common Abdominal muscles are used for inhalation until age 5-6 yrs. Respiratory rate is higher Increased BMR raises oxygen needs 141 The Respiratory System Upper Airway Disorders Tonsillitis Croup Epiglottis Foreign Body Aspiration Lower Airway Disorders Bronchiolitis Asthma Cystic Fibrosis Photo Source: Del Mar Image Library; Used with permission 142 Tonsillitis CLINICAL MANIFESTATIONS Sore throat Mouth breathing Sleep Apnea Difficulty swallowing Fever Throat C&S/Rapid Strep IMPLEMENTATIONS Ease Respiratory Efforts Provide Comfort Warm saline gargles Pain Medication Throat lozenges Reduce Fever Promote Hydration Administer Antibiotics Provide Rest Patient Teaching Tonsillectomy may be necessary 143 Tonsillectomy Pre-operative Nursing Care Monitor Labs (CBC, PT, PTT) Age-appropriate Preparation/Teaching Surgical Consent Post-operative Nursing Care Frequent site assessment - visualize! Monitor for S/S of Complications Pain Management Diet (push fluids-no citrus juices or red, advance diet) Patient Teaching 144 Croup/Epiglottitis • Infection and swelling of larynx, trachea, epiglottis, bronchi • Often preceded by URI traveling downward • Causative agent: Viral • Characterized by hoarseness, barky cough, inspiratory stridor, and respiratory distress • Most common ages 6 mo-3 yrs • LTB form most common Photo Source: Del Mar Image Library; Used with permission 145 Acute Epiglottitis • • • • • • • • Bacterial form of croup affecting epiglottis LIFE-THREATENING EMERGENCY Wellness to complete obstruction in 2-6 hours Most common in ages 2-5 years Do not examine throat! Have functional emergency equipment at bedside - Priority! Often the child is intubated 4 D’s - Drooling, Dysphagia, Dysphonia, Distressed Inspiratory Effort • Lateral Neck X-ray shows “thumb sign” • HIB vaccine has reduced the cases dramatically 146 Croup/Epiglottitis Nursing Interventions Maintain Patent Airway Assess and Monitor Ease Respiratory Efforts Promote Hydration Reduce Fever Calm Environment Nursing Interventions Administer Meds Corticosteroids (HHN) Nebulizer treatment of Racemic Epinephrine PRN stridor Antibiotic for epiglottitis Promote Rest 147 Foreign Body Aspiration • Occurs most often in small children • Choking, coughing, wheezing, respiratory difficulty • Often it is round food, such as hot dogs, grapes, nuts, popcorn • Bronchoscopy often needed for removal • Age-appropriate preparation needed for procedure • Prevention and parent education is very important 148 Bronchiolitis/RSV • Acute viral infection of the bronchioles causing an inflammatory/obstructive process to occur • Increased amount of mucus and exudates preventing expiration of air and overinflation of lungs • Causative agent in 85% of cases is Respiratory Syncytial Virus (RSV). It is highly contagious - contact isolation must be enforced. • Nasal swab or nasal washing obtained for viral panel, including RSV • CXR shows hyperinflation and consolidation if atelectasis present • Primarily seen in children under 2 years of age • Most common in winter and early spring • Palivizumab (Synagis) 149 Bronchiolitis/RSV CLINICAL MANIFESTATIONS Nasal Congestion Cough Rhonchi, Crackles, Wheezes Increased RR & SOB Respiratory Distress Fever Poor Feeding IMPLEMENTATIONS Suction – priority Bronchodilator via HHN CPT Promote fluids Monitor VS , SaO2, lung sounds & respiratory effort Supplemental oxygen Reduce fever Promote rest HANDWASHING! 150 Asthma CLINICAL MANIFESTATIONS Tachypnea SaO2 below 95% on RA Wheezes, crackles Retractions, nasal flaring Non-productive cough Silent chest Restlessness, fatigue Orthopnea Abdominal pain CXR = hyperinflation INTERVENTIONS Monitor VS (HR, RR) Monitor SaO2 Auscultate lung sounds Monitor respiratory effort Humified oxygen Calm environment Ease respiratory efforts Promote hydration Promote rest Monitor labs/x-rays Patient teaching 151 Asthma Administer Medications Bronchodilator via HHN or MDI with spacer (Albuterol) Peak flows should always be done before and after Tx Mast cell inhibitor via HHN or MDI (Cromolyn Sodium Intal) Corticosteroid IV or PO (Solu-medrol or Decadron) Antibiotic if precipitated from a respiratory infection Home Medication Management Bronchodilator via HHN or MDI with spacer (Albuterol Proventil, Levalbuterol - Xopenex) Inhaled steroids (Beclamethasone - Vanceril) Mast cell inhibitor via HHN or MDI (Cromolyn Sodium Intal) Leukotriene modifiers PO for long-term control - Singular 152 Cystic Fibrosis 1 in 1,500-2,000 live births Dysfunction of the exocrine gland (mucus producing) Multi-system disorder Secretions are thick and cause obstruction and fibrosis of tissue. The clinical manifestations are the result of the obstructive process. Sweat has a characteristic high sodium- Sweat Chloride Test Pancreatic involvement in 85% of CF patients Disease is ultimately fatal. Average age at death: 32 years 153 Cystic Fibrosis PULMONARY MANIFESTATIONS • Initial • Wheezing • Dry, non-productive cough • Eventual & Progressive • • • • Repeated lung infections Wet & paroxysmal cough Emphysema/Atelectasis Barrel-chest - Clubbing - Cyanosis GI MANIFESTATIONS • Large, loose, frothy and foul-smelling stools • Increased appetite (early) • Loss of appetite (later) • Weight loss • FTT • Distended abdomen • Thin extremities • Deficiency of A,D, E, K • Anemia 154 Cystic Fibrosis MANAGEMENT/INTERVENTIONS – Airway Clearance - Chest physiotherapy (CPT) Priority – Drug Therapy • • • • Bronchodilators - via HHN Mucolytic Agent (Dnase-Pulmozyme) - via HHN Antibiotics - via HHN, IV, or PO Digestive enzymes Nutrition - needs are at 150% • Increased calories and protein - TPN or GT feedings at night • Additional fat soluble vitamins • Additional salt with vigorous exercise and hot weather Exercise Patient Teaching 155 Otitis Media Most common childhood illness Inflammation of middle ear Impaired eustachian tube causes decreased ventilation and drainage Acute otitis media (AOM) Infectious process by pathogen Infection can spread leading to meningitis S/S: pain, pulling on ears, fever, irritability, vomiting, diarrhea, ear drainage, full/bulging tympanic membrane Otitis media with effusion (OME) Inflammation of middle ear with fluid behind tympanic membrane-no infection Peaks spring and fall (allergies) Chronic otitis media Inflammation of middle ear > 3 mo Can lead to hearing loss/delayed speech Photo Source: Del Mar Image Library; Used with permission 156 Otitis Media RISK FACTORS Secondary smoke Formula feeding (positioning) Day care Pacifier > 6 mo old TREATMENT Antibiotics (for AOM) Myringotomy with Pressure Equalizing (PE) tubes INTERVENTIONS Teaching No bottle propping Feeding techniques Medication regimen PAIN MANAGEMENT Fever management Surgery prep if needed Photo Source: Del Mar Image Library; Used with permission 157 Let’s Review The nurse’s first action in responding to a child with tachypnea, grunting, and retractions is to: A. Place the child in an upright, semi-fowler’s position. B. Apply a pulse oximeter to determine oxygen saturation. C. Assess for further symptoms. D. Call for a stat respiratory nebulizer treatment (HHN). 158 Let’s Review A 3-year-old child is brought to the emergency room with a sore throat, anxiety, and drooling. The priority nursing action is to: A. Inspect the child’s throat for infection. B. Prepare intubation equipment and call the physician. C. Obtain a throat culture for respiratory syncytial virus (RSV). C. Obtain vital signs and auscultate lung sounds. 159 Let’s Review An assessment finding in a child with asthma requiring immediate action by the nurse is: A. B. C. D. Diminished breath sounds. Wheezing in bronchi. Crackles in lungs. Refusal to take PO fluids. 160 Let’s Review Which sign is indicative of air hunger in an infant? A. Nasal flaring. B. Periods of apnea lasting 15 seconds. C. Irregular respiratory pattern. D. Abdominal breathing. 161 Let’s Review The priority nursing intervention in caring for the infant with Respiratory Syncytial Virus (RSV) induced bronchiolitis is: A. Nasopharyngeal suctioning. B. Coughing and deep breathing exercises. C. Administration of intravenous antibiotic. D. Administration of antipyretics for fever. 162 Gastrointestinal System • Many GI issues require surgical intervention • Nursing interventions will often include general pre and post-op care • Bilious vomiting is a sign of GI obstruction and requires immediate intervention • Assess stools! • Assess hydration status Photo Source: Del Mar Image Library; Used with permission 163 Gastrointestinal System Pediatric Variances • Mechanical functions of digestion are immature at birth • Liver functions are immature throughout infancy • Production of mucosal-lining antibodies is decreased • Infants have decreased saliva • Infant’s stomach lies transversely • Peristalsis is faster in infants • Digestive processes are mature as a toddler • The child’s liver and spleen are large and vascular • Infants and children who vomit bile-colored emesis require immediate attention • Gastric acidity is low at birth 164 The Gastrointestinal System 8 Altered Connections 3 Esophageal Atresia/Tracheoesophageal Fistula 3 Cleft Lip and Palate 8 Gastrointestinal Disorders 3 3 3 8 Gastroesophageal Reflux Hirschsprung’s Disease Intussusception 3 Pyloric Stenosis 3 Imperforate Anus Acquired Gastrointestinal Disorders 3 Celiac Disease 3 Appendicitis 3 Parasitic Worms 165 ESOPHAGEAL ATRESIA & TRACHEOESOPHAGEAL FISTULA • • • • Congenital defects of esophagus EA is an incomplete formation of esophagus TEF is a fistula between the trachea and esophagus Classic 3 “C’s” - coughing,choking,cyanosis Photo Source: Del Mar Image Library; Used with permission 166 ESOPHAGEAL ATRESIA & TRACHEOESOPHAGEAL FISTULA SIGNS/SYMPTOM • Copious, frothy oral secretions • Abdominal distension from air in stomach • Look for 3 C’s • Confirmed with radiographic studies TREATMENT • Surgery: either a one- or two-stage repair • Pre-op care focuses on preventing aspiration and hydration • Post-op care focus is a patent airway, prevent incisional trauma 167 Cleft Lip/Palate May present as single defect or combined Non-union of tissue and bone of upper lip and hard/soft palate during fetal development CL-failure of nasal & maxillary processes to fuse at 5-8 weeks gestation CP-failure of palatine planes to fuse 7-12 weeks gestation Cleft interferes with normal anatomic structure of lips, nose, palate, muscles – depending on severity and placement Open communication between mouth and nose with cleft palate 168 Cleft Lip/Palate Multidisciplinary care throughout childhood and early adulthood Nutrition is a challenge in infancy ESSR method (enlarge, stimulate, swallow, rest) Risk for aspiration Respiratory distress Altered bonding is a possibility Photo Source: Del Mar Image Library; Used with permission 169 CLEFT LIP & CLEFT PALATE: Operative Care Cleft lip surgery by 4 weeks & again at 4-5 yrs Cleft palate surgery at 6-24 months of age, usually done by 1 year so speech will not be affected Protect suture lines- priority Monitor for infection Clean Cleft Lip incision Pain Management Cleft Palate starts feedings 48-hour post-op: Clear and advance to soft diet No straws, pacifiers, spouted cups Rinse mouth after feeding 170 GASTROESOPHAGEAL REFLUX Regurgitation of gastric contents back into esophagus - 50% healthy term babies affected Related to inappropriate relaxation of Lower Esophageal Sphincter (LES) making the LES pressure less than the intra abdominal pressure GER may predispose patient to aspiration and pneumonia Apnea has been associated with GER chance of GER after 12-18 mo old related to growth due to elongation of esophagus and the LES drops below the diaphragm Photo Source: Del Mar Image Library; Used with permission 171 GASTROESOPHAGEAL REFLUX SIGNS/SYMPTOMS • • • • • • • Vomiting/spitting up Gagging during feedings Irritability Arching/posturing Frequent URI’s/OM Anemia Bloody stools DIAGNOSTIC EVAL • History of feedings/PE • Upper GI/Barium swallow to eliminate anatomical problems • Upper GI endoscopy to visualize esophageal mucosa • pH probe study 172 GASTROESOPHAGEAL REFLUX: Therapeutic Management • Positioning • Prone HOB 30° • Right side • Dietary modifications • Medications • Prokinetic agents: LES pressure & gastric motility • Histamine H-2 antagonists are added if esophagitis : acid • Proton Pump Inhibitors if H-2 ineffective:acid • Mucosal Protectants • Small, frequent feedings, burp often • Possibly thicken formula • Avoid fatty, spicy foods caffeine, & citrus • Surgery: fundoplication • Teach 173 HIRSHSPRUNG’S • Aganglionic megacolon No ganglion cells at affected area usually at rectum/proximal portion of lower intestine Absence of peristalsis leads to intestinal distension, ischemia & maybe enterocolitis • Treatment Mild-mod: stool softeners & rectal irrigations Mod-severe: single or 2-step surgery Colostomy with later pull-through Photo Source: Del Mar Image Library; Used with permission 174 HIRSHSPRUNG’S SIGNS/SYMPTOMS Infants Unable to pass meconium stool within 24 hours of life Abdominal distention Bilious vomiting Refusal to feed Failure to thrive Children Chronic constipation Pellet or ribbon-like stools (foul- smelling) Vomiting/FTT NURSING INTERVENTIONS • Surgery prep: bowel cleansing, antibiotics, NPO, IVF’s, therapeutic play for surgery preparation • Infection & Skin Integrity: monitor ostomy/anus • Nutrition & Hydration: NGT, NPO then advance to Diet as tolerated, assess bowel function and abdominal status 175 INTUSSUSCEPTION • Prolapse or “telescoping” of one portion of the intestine into another • Abrupt onset • Usually occurs in 3-24 months of age • Sudden abdominal pain • Vomiting • Red, current jelly stool • Abd distention/tender • Lethargy • Can lead to septic shock Photo Source: Del Mar Image Library; Used with permission 176 INTUSSUSCEPTION DIAGNOSTIC STUDY • Barium or air enema • Abdominal ultrasound TREATMENT • Hydrostatic reduction: force exerted using water-soluble contrast and air to push the affected intestine apart • Surgical reduction if hydrostatic reduction is unsuccessful • • • • • NURSING INTERVENTIONS Monitor for infection, shock, pain Maintain hydration - assess status! Prepare child/parent for hydrostatic reduction teach, consent, NPO, NGT Monitor stools pre & post procedure If surgery: general pre & post-op care 177 PYLORIC STENOSIS Hypertrophy of pyloric sphincter, causing a narrowing/ obstruction (bands pylorus) Usually occurs between 2-8 weeks of age Infant presents with non-bilious projectile vomiting, and is “always hungry” Can lead to dehydration and hypochloremic metabolic alkalosis Weight loss Photo Source: Del Mar Image Library; Used with permission 178 PYLORIC STENOSIS DIAGNOSTIC EVAL • History/PE: “olive” palpated in epigastrum • Upper GI (string sign) • Abdominal Ultrasound TREATMENT • Surgical Intervention: Pyloromyotomy INTERVENTIONS • Pre-op: NPO, NGT to LIS, hydration, I/O, monitor electrolytes • Post-op: Start feedings in 4-6 hrs. Progressive feeding schedule begin w/5cc GW half strength formula Full strength formula 179 IMPERFERATE ANUS • Anorectal malformations • No obvious anal opening • Fistula may be present from distal rectum to perineum or GU system • Diagnostic Eval: patency of anus in newborn, passage of meconium; ultrasound is suspected • Therapeutic Management: manual dilatation for anal stenosis, surgical treatment for malformations • Nursing Implementations: pre and post-op care – IV fluids, consent, assessing surgical site for infection and monitoring for complications, possible NGT, diet progression, possible colostomy and teaching; preferred post-op condition is sidelying. 180 Celiac Disease • Malabsorption syndrome characterized by intolerance of gluten (rye, oats, wheat and barley) • Familial disease - more common in Caucasians • Thought to be an inborn error of metabolism or an immunological disorder • Reduced absorptive surfaces in small intestine which causes marked malabsorption of fats (frothy, foul-smelling stools) • Child has diarrhea, abdominal distention, failure to thrive • Treatment is lifelong low-gluten diet; corn and rice are substituted grain foods 181 APPENDICITIS • Inflammation and infection of vermiform appendix, usually related to an obstruction • Cause may be bacteria, virus, trauma • Ischemia can result from the obstruction, leading to necrosis causing perforation • S/S: periumbilical painRLQ pain (McBurney’s point), fever, vomiting, diarrhea, lethargy, irritability, WBC’s • Surgery is necessary • If ruptured, often child will receive IV antibiotics for 24 hrs prior to OR • Pre-op Care: NPO, pain management, hydration, prep & teaching, consent • Post-op Care: routine post-op care, IVF/antibiotics, NPODAT, ambulation, positioning, pain management, wound care, possible drains. 182 PINWORM (enterobiasis) Transmission: oral-fecal Persist in indoors for up to 3 weeks contaminating anything they contact (toilets, bed linens) S/S: intense perianal itch, sleeplessness, abd pain, vomiting Scotch tape test – collects eggs laid by female outside of anus. Must be obtained in am prior to bath or BM. Treatment: *mebendazole (Vermox) for over 2 years of age. Under 2 years of age treatment may be pyrvinium pamoate (Povan) which stains stool and emesis red *All family members must be treated. 183 Let’s Review Which intervention would have the highest priority for the nurse assisting in the feeding of a child post cleft palate repair? A. Permiting the child to choose the liquids desired. B. Providing diversional activities during feeding. C. Applying wrist restraints. D. Cleansing the mouth with water after each feeding. 184 Let’s Review Which food choice by a parent of a child with celiac disease indicates a need for further teaching? A. B. C. D. Oatmeal Rice Cornbread Beef 185 Let’s Review Which assessment finding would the nurse find in a child with Hirschsprung’s Disease? A. Current jelly stool B. Diarrhea C. Constipation D. Foul-smelling, fatty stool 186 Let’s Review Children with gastroenteritis often receive intravenous fluids to correct dehydration. How would you explain the need for IV fluids to a 3 year-old child? A. “The doctor wants you to get more water, and this is the best way to get it.” B. “Your stomach is sick and won’t let you drink anything. The water going through the tube will help you feel better.” C. “See how much better your roommate is feeling with his IV! You will get better, too.” D. “The water in the IV goes into your veins and replaces the water you have lost from vomiting and diarrhea.” 187 Let’s Review The nurse caring for a child with suspected appendicitis would question which physician order? A. NPO status B. Start IV fluids of D5 ½ NS at 50 mls/hour C. Complete Blood Count (CBC) D. Apply heating pad to abdomen for comfort 188 Genitourinary System Anatomy & Physiology Review • The GU system maintains homeostasis of the body (water & electrolytes) • Responsible for the excretion of waste products • Nephron is the workhorse of the kidney (filter blood at the rate of 125mL/minute)-GFR • Renin helps maintain Na & water balance (and B/P) • Kidneys produce erythropoeitin which stimulates RBC production in marrow Photo Source: Del Mar Image Library; Used with permission 189 Pediatric Variances Genitourinary System • Infants & young children excrete urine at a higher rate related to the increased BMR producing more waste • Infant kidneys have function if under stress • Infant can’t concentrate urine well until 3-6 mo • In infants, kidney & bladder are abdominal organs • Infant kidneys are less protected because of unossified ribs, less fat padding & large size • Young children have shorter urethras • Nephrons continue to develop after birth 190 The Genitourinary System Minimum urine outputs by age groups: • INFANTS & TODDLERS – 2-3 ml/kg/hr • PRESCHOOLERS & YOUNG SCHOOL-AGE – 1-2 ml/kg/hr • SCHOOL-AGE & ADOLESCENTS – 0.5-1 ml/kg/hr • TIP: Bladder capacity in ounces: AGE in years + 2 Example: a 2-year-old’s bladder can hold up to 4 ounces or 120 mls 191 The Genitourinary System d Disorders of the Genitourinary System F F F F Enuresis Nephrotic Syndrome Acute Glomerulonephritis Hemolytic Uremic Syndrome (HUS) 192 Glomerulonephritis • Group of kidney disorders that show main focus of injury is the glomerulus • It is characterized by inflammation of the glomerular capillaries • Acute disorders occur suddenly and resolve completely • Acute poststreptococcal glomerulonephritis (APSGN) is the most common type • History, presenting symptoms, and lab results establishes the diagnosis of APSGN 193 Glomerulonephritis PA THOPHYSIOLOGY Strep tococcal Infection Pro du cing A n tib od ie s Ba cte ria l A ntige ns p lu s A n tibo dies f orm Immu ne Co mplex es & t rap in Glome rulus Inflamm atory R espo nse In ju ry to Cap illa ry Wa lls Ine ffective Filtratio n Pro te in s Pas s Th rou gh De cre as ed GFR Kidn eys Enl arge w ith so dium, w a te r, w as te ED EMA AC U TE R EN AL FAILU RE Photo Source: Teresa Simbro, RN, Santa Ana College, Used with permission. 194 Glomerulonephritis ASSESSMENT • Hematuria • Proteinuria • Edema: periorbital, ankles • Urine Output • Hypertension • Fatigue • Possible fever • Abdominal discomfort • Labs: +ASO, Bicarb,K BUN, Creat, H & H INTERVENTIONS • Monitor Urine (Dipstick) • Monitor fluid overload • Assess lung sounds/Resp effort • Possible fluid & salt restriction • Monitor I/O, Daily Weights • Monitor VS • Antibiotic, diuretic & antihypertensive medications • Promote & provide rest • Provide comfort measures • Monitor labs 195 Nephrotic Syndrome • Kidney disorder characterized by proteinuria, hypoalbuminemia, and edema. • There is primary (involving kidney only) and secondary (caused by systemic disease or heavy metal poisoning) NS. Primary is the most common (MCNS). • Cause not fully understood-may have an immunologic component. • Primary age affected is 2-6 years (boys 2:1) • There is no occlusion of glomerular vessels. • Loss of immunoglobulins also occur (IgG) • Hypovolemia and the severe proteinuria put the child in a hypercoagulable state • Treatment is prednisone (2mg/kg/day) for about 4-6 weeks. Remission is obtained when the urine protein is 0-tr for 5-7 days • Albumin followed by furosemide may be given for the edema 196 Nephrotic Syndrome PATHOPHYSIOLOGY Alteration in Glomerulus Damage to Basement Membrane of glomerulus (inc reased permeabilit y) Proteinuria (Hy poalbuminemia) Fluid Shif t Intravasc ular to Interst itial HYPOVOLEMIA Dec reased Renal Blood Flow Triggers Renin Product ion Caus ing Increas ed Aldos terone Reabsorpt ion of Sodium and Water ret ention Hy perlipidemia EDEMA Photo Source: Teresa Simbro, RN, Santa Ana College, Used with permission. 197 Nephrotic Syndrome ASSESSMENT INTERVENTIONS • Proteinuria (3-4+), frothy urine • Edema (pitting):periorbital, genitals, lower extremities, abdominal • Urine Output (Hypovolemia) • Normotensive or hypotensive • Fatigue • Recent URI, Pneumonia • Abdominal Pain/Anorexia • Labs: • Monitor Urine (Dipstick) • Monitor edema/dehydration • Assess skin integrity/turn often • Possible fluid & salt restriction • Monitor I/O, Daily Weights • Monitor VS & S/S of infection • Administer medications • Promote & provide rest • Monitor labs • HANDWASHING/monitor visitors Albumin Platelets H & H Cholesterol Triglycerides 198 Hemolytic Uremic Syndrome (HUS) • It is the most common cause of acute renal failure (ARF) in children. • HUS is characterized by the triad of anemia, thrombocytopenia, and ARF. • Most children have associated GI symptoms- almost all are caused by e. coli 0157. • Treatment is supportive and based on symptoms. • No antibiotics are given; more damage can be caused. • Serum electrolytes may be outside of normal limits. • Blood transfusions and/or dialysis may be necessary. • More than 90% of the children recover with good renal function. 199 Hemolytic Uremic Syndrome (HUS) GASTROENTER ITIS e. coli #0157 Bacteria Adher es t o GI Mucosa Mult iplies Releases Toxins Damages C apillar y Walls Inf lammatory Response Occlusion of Vessels Thr ombocytopenia Collect ion of Fibrin Lipids Platelet F ragments Fr agmented RBC 's Causing Anemia (Glomer ular Vessels) Decreased GF R Photo Source: Teresa Simbro, RN, Santa Ana College, Used with permission. Acute Renal F ailur e 200 Hemolytic Uremic Syndrome (HUS) ASSESSMENT • History: emesis, bloody diarrhea, abd pain, Urine • Petechiae, bruises, purpura • Edema (possible CHF) • Hepatosplenomegaly • Altered LOC, seizure • Hypertension • Fatigue • Abdominal discomfort • Labs: Lytes may be abnormal BUN Creatinine H&H Platelets INTERVENTIONS • Monitor I/O, Daily Weights • Evaluate for signs of bleeding • Monitor fluid overload/edema • Assess for dehydration • Monitor VS with neuro checks • Seizure Precautions, HOB • Diuretic & antihypertensive medications • Provide rest/calm environment • Provide comfort measures • Monitor labs closely 201 Enuresis • Involuntary passage of urine in children whose chronological or developmental age is at least 5 years of age • Voiding occurs at least twice a week for minimum 3 months • More common in boys • Alteration in neuromuscular bladder function • Often benign and self-limiting • Organic factor could be the cause • Familial tendency • Emotional factor could be considered • Therapeutic techniques include: bladder training, night fluid restriction, drugs (imipramine, oxybutynin, DDAVP) 202 Let’s Review A clinical finding that warrants further intervention for a child with acute poststreptococcal glomerulonephritis is: A. B. C. D. Weight loss to 1 pound of pre-illness weight. Urine output of 1 ml/kg per hour. A normal blood pressure. Inspiratory crackles. 203 Let’s Review A 3 year-old is scheduled for surgery to remove a Wilms tumor from one kidney. The parents ask the nurse what treatments, if any, will be necessary after recovery from surgery. The nurse’s explanation is based on knowledge that: A. B. C. D. No additional treatments are necessary. Chemotherapy may be necessary. Chemotherapy is indicated. Kidney transplant is indicated. 204 Let’s Review Fluid balance in the child who has acute glomerulonephritis is best estimated by assessing: A. B. C. D. Intake and output Abdominal circumference Daily weights Degree of edema 205 Let’s Review In evaluating the effectiveness of nursing actions when caring for a child with nephrotic syndrome, the nurse expects to find: A. B. C. D. A recurrence of pneumonia. Weight gain. Increased edema. Decreased edema. 206 Pediatric Variances Musculoskeletal System Bone Growth: Linear growth results from skeletal development Bone circumference growth occurs as new bone tissue is formed beneath the periosteum Skeletal maturity is reached by age 17 in boys and 2 years after menarche in girls (14 yrs) Bone growth affected by Wolff’s Law - bone grows in the direction in which stress is placed on it Certain characteristics of bone affect injury and healing Children’s bones are softer and are easily fractured 207 Pediatric Variances Musculoskeletal System Muscle Growth: Responsible for a large part of increased body weight The number of muscle fibers is constant throughout life Results from increase in size of fibers and increased number of nuclei per fiber Most apparent in adolescent period 208 The Musculoskeletal System QDisorders of the Musculoskeletal System m m m m m m Developmental Dysplasia of the Hip Talipes (Clubfoot) Osteogenesis Imperfecta Scoliosis Muscular Dystrophy Juvenile Rheumatoid Arthritis 209 Developmental Dysplasia of the Hip (DDH) Variety of hip abnormalities – shallow acetabulum, subluxation or dislocation Often made in newborn period – often appears as hip joint laxity rather than dislocation Ortolani click if < 4 weeks old, older ultrasound needed to diagnose Treatment is Pavlik Harness (abducted position) for newborn to 6 months old – monitor for Avascular Necrosis 6-18 months – traction followed by spica cast Older children – operative reduction Priority nursing interventions are skin care and facilitating normal growth and development 210 Talipes (Clubfoot) Most common type is when foot is pointed downward and inward Often associated with other disorders May be due to decreased movement in utero Treatment requires surgical intervention Serial casting is begun shortly after birth and usually lasts for 8-12 weeks Priority nursing interventions are skin care and facilitating normal growth and development 211 Osteogenesis Imperfecta (OI) Inherited disorder of connective tissue and excessive fragility of bones Pathologic fractures occur easily Incidence of fractures decrease at puberty related to increased hormones making bones stronger Treatment is supportive: careful handling of extremities, braces, physical therapy, weight control diet, stress on home safety Surgical techniques for correcting deformities and for intermedullary rodding 212 Scoliosis o Abnormal curvature of the spine (lateral) o Congenital or develops later, most common during the growth spurt of early adolescence (idiopathic) o Diagnosis is made by physical exam and x-rays o Treatment for curvatures < 40 degrees is bracing o Surgical intervention is for severe curvatures – internal fixation and instrumentation (Harrington) o Postoperative care includes logrolling, neurologic assessments, pain management, skin care, assessing for paralytic ileus and possible mesenteric artery syndrome o Don’t forget the developmental needs of the adolescent 213 Muscular Dystrophy • Duchenne’s Muscular Dystrophy most common • Gradual degeneration of muscle fibers • S/S begin to show about 3 years of age – difficulties in running and climbing stairs • Changes to having difficulty moving from a sitting/supine position • Profound muscular atrophy continues, wheelchair by 12 yrs • Respiratory and cardiac muscles affected and death is usually respiratory or cardiac in nature • Diagnosis made with physical exam, muscle biopsy, EMG, serum studies: AST (SGOT), aldolase, creatine phosphokinase high first 2 years of life • Nursing care is to maintain optimal level of functioning and to help the child and family cope with the progression and limitations of the disease 214 Juvenile (Rheumatoid) Arthritis • Inflammatory disease with an unknown cause • Occurs in children < 16 years; lasts > 6 weeks • Clinical manifestations: stiffness, swelling, and loss of motion in affected joints, tender to touch • Therapeutic management includes drug therapy (NSAID’s, SAARD’s, cytoxic drugs, corticosterioids), physical and occupational therapy, exercise (swimming), moist heat for pain and stiffness, general comfort measures 215 General Nursing Interventions for Children with Musculoskeletal Dysfunctions (immobility) • • • • • • • • Maintain optimal level of functioning Promote general good health Facilitate compliance Facilitate optimal growth and development Maintain skin integrity Safety considerations at home Pain management Support child and family 216 Let’s Review An infant is being treated non-surgically for clubfoot. Which describes a major goal of care for this patient? Prevention of: A. B. C. D. Skin breakdown Calf atrophy Structural ankle deformities Thigh atrophy 217 Let’s Review The nurse is helping parents create a plan of care for their child with osteogenesis imperfecta. A realistic outcome is for this child to: A. Have a decreased number of fractures B. Demonstrate normal growth patterns C. Participate in contact sports D. Have no fractures after infancy 218 Let’s Review During acute, painful episodes of juvenile arthritis, a priority intervention is initiating: A. A weight-control diet to decrease stress on the joints. B. Proper positioning of the affected joints to prevent musculo-skeletal complications. C. Complete bedrest to decrease stress to the joints. D. High-resistance exercises to maintain muscular tone in the affected joints. 219 Pediatric Variances Endocrine System Growth Hormone: Does not effect prenatal growth Main effect on linear growth Maintains rate of body protein synthesis Thyroid-stimulating hormone (TSH): Important for growth of bones, teeth, brain Secretion decreases throughout childhood and increases at puberty Adrenocorticotrophic Hormone (ACTH): Activated in adolescent Stimulates adrenals to secrete sex hormones Influences production of gonadotropic hormone 220 The Endocrine System Disorders of the Endocrine System 8 8 8 8 Type 1 Diabetes Mellitus Congenital Hypothyroidism Growth Hormone Deficiency Precocious Puberty 221 Type 1 Diabetes Mellitus Pediatric Considerations INSULIN • Most children are well-controlled with BID dosing of fast acting (Lispro) short acting (regular) and intermediate acting (NPH, Lente) insulin. There is also Lantis, an insulin that acts a “basal.” • U-20 insulin is also available for infants • Insulin pump, pen • “Honeymoon” phase • Stress, infection, illness and growth at puberty can increase insulin needs 222 Type 1 Diabetes Mellitus Pediatric Considerations • HYPOGLYCEMIC EPISODES • In small children it is more difficult to determine and may just be a behavior change. • Treatment is the same – simple sugar – assess LOC first! • NUTRITION • Carb counting – most children’s calories should not be restricted; meal plan might change as child grows. • Some sweets may be incorporated into the diet and may help with compliance. • 3meals with 3 snacks per day 223 Type 1 Diabetes Mellitus Pediatric Considerations EXERCISE • Important for normal growth and development • Assists with daily utilization of dietary intake • Enhances insulin absorption, so may decrease amount needed • Add 15-30 grams of carbs for each 45-60 minutes of exercise • Watch for hypoglycemia with strenuous exercise 224 Type 1 Diabetes Mellitus Pediatric Considerations DEVELOPMENTAL ISSUES • Infant/Toddler • Autonomy & choices, rituals, hypoglycemia identification difficult • Preschooler • • • • Magical thinking-let them know they did not cause it Use dolls for teaching Urine testing may be done Can choose finger to use for testing • School-age • Very busy with school and activities • Likes tasks and explanations • Can do self blood testing; injections at age 8-10 years • Adolescents • Peers and body image preoccupation • High risk for non-compliance • Collaborative health care with parent involvement very important 225 Congenital Hypothyroidism • Thyroid is not producing enough thyroid hormone to meet needs of the body (resulting in↓oxygen consumption, BMR and protein synthesis) • Clinical manifestations: cool, mottled skin, bradycardia, large tongue, large fontanel, hypothermic, hypotonia, lethargy, feeding problems - THINK SLOW! • Labs: High TSH, low T4 • Decreased brain development will result with cognitive impairments • Part of newborn screening • Therapeutic management is life-long thyroid hormone replacement (levothyroxine) 226 Growth Hormone (GH) Deficiency • Deficient secretion of growth hormone • Definitive diagnosis is made with GH levels (using stimulation testing) under 10mg/ml and x-rays of hand and wrist for ossification levels • Treatment is replacement of GH (subcutaneous daily injections) until goals met • Nursing care is directed at child and family support • Remember to interact and speak to the child at her appropriate developmental level! 227 Precocious Puberty • Manifestations of sexual development in boys younger than 9 years and girls younger that 8 yrs • Causes also an early acceleration of growth with closure of growth plates • Therapeutic management is directed toward the specific cause, if known • The early secretion of sex hormones will be treated with monthly subcutaneous injections of leuteinizing hormone-releasing hormone (LHRH) • Priority interventions are directed at psychological support of child and family – encourage play with same age peers 228 Let’s Review A child weighing 25 kilograms is being treated with synthetic growth hormone. The recommended dosage range is 0.3 – 0.7 mg/kg/week. The mother informs the nurse that her child receives 1.25 mg subcutaneously at bedtime 6 times per week. The proper response from the nurse would be: A. “That dose is too high, the doctor needs to be notified.” B. “You are doing a great job, that is the correct dose for your child.” C. “The injection should be given intramuscular, not subcutaneous.” D. “That dose is too low based on your child’s new weight.” 229 Let’s Review The nurse should include which information in teaching the parents of a recently diagnosed toddler with Type 1 diabetes mellitus? A. Allow the toddler to choose which finger to use for blood glucose monitoring B. Allow the toddler to assist with the daily insulin injections C. Test the toddler’s blood glucose every time she goes out to play D. Let the toddler determine meal times 230 Let’s Review Which is the most appropriate teaching intervention for a nurse to give parents of a 6year-old with precocious puberty? A. Advise the parents to consider birth control for their child B. Inform the parents there is no treatment currently available C. Explain the importance for the child to foster relationships with peers D. Assure the parents there is no increased risk for sexual abuse. 231 Let’s Review Number in order of priority the following interventions needed while caring for a patient in diabetic ketoacidosis. _____ Hydration _____ Electrolyte replacement _____ Dietary intake _____ IV Insulin _____ Subcutaneous insulin 232 Pediatric Variances Integumentary System Evaporative water loss is greater in infants/small children Skin more susceptible to bacterial infections More prone to toxic erythema More susceptible to sweat retention and maceration 233 The Integumentary System Disorders of the Integumentary System Impetigo Roseola Diaper Rash 234 Impetigo • Superficial bacterial skin infection, often secondary from insect bite • Highly contagious • Late summer outbreak • Toddlers & preschoolers • Rash is bullous or honeycolored crusted lesions • Treatment: topical & systemic antibiotics, comfort measures, teaching, preventing comps Photo Source: Del Mar Image Library; Used with permission 235 Roseola • Transmission: contact with secretions (saliva) • Virus • 6 - 18 months • Fever »flu symptoms » rose-pink macular rash • Fades with pressure • Treatment is supportive Photo Source: Del Mar Image Library; Used with permission 236 Diaper Rash • Cause could be fungal in nature; assess mucous membranes for thrush • Cause could be due to infrequent diaper changes, an allergic reaction to the diaper product or diarrhea • Skin care includes appropriate skin barrier cream/ointment, keeping area dry • Teach parents appropriate skin care 237 Medication Administration Oral Medication Hold infant with head elevated to prevent aspiration Slowly instill liquid meds by dropper along side of the tongue Crush pills and mix with sweet-tasting liquid if permitted, but don’t add too much liquid! Allow choices for the child such as which med to take first Flush following gastrostomy or NG tube 238 Factors to consider when selecting IM sites Age Weight Muscle development Amount of subcutaneous fat Type of drug Drug’s absorption rate 239 IM and SQ Meds Select needle length according to muscle size for IM Infant - should use 1 inch needle Preemies can use 5/8 inch needle • Use Z-track for iron and tissue-toxic meds • Apply EMLA or other topical anesthetic 45-60 minutes prior to injection • May mix medication with lidocaine • Some medications may be need to be separated into 2 injections depending on amount 240 Peds IM Injection Sites Vastus lateralis for infants Ventrogluteal and dorsogluteal Don’t inject into dorsogluteal until age 3 years - muscle not well developed until child walks and sciatic occupies a larger portion of the area. Deltoid after 3 years 241 IV Meds Site may be peripheral or central Administer IV fluids cautiously Always use infusion pumps with infants and small children Inspect sites frequently (q 1-2 hours) for signs of infiltration Cool blanched skin, puffiness( infiltration) Warm and reddened skin (inflammation) 242 Nose Drops Instill in one nare at a time in infants because they are obligate nose breathers. Suction nare with bulb syringe prior to administration if nasal congestion present 243 Ear Meds Pull the ear down and back to instill eardrops in infants/toddler (↓3 years pull ↓) Pull the ear up and out to instill in older children (↑ 3 years pull ↑) Have medication at room temperature 244 Rectal Medication Insert the suppository past the anal sphincter Hold buttocks together for a few seconds after insertion to prevent expulsion of medication It is a very stressful route for children, and the school-age and adolescent have issues with modesty. 245 Inhalers and Spacers Shake the inhaler for 2-5 seconds. Position inhaler into spacer (with mask or mouthpiece). After normal exhale, place mask on face or mouthpiece in mouth – both with a good seal. Have child inhale slowly after canister is pressed down . Have child take a few breaths with a spacer and without a spacer have them hold breath for few seconds after medication released. Inhalers without spacers aren’t placed in the mouth because spacers require a seal around mouthpiece; masks with spacers can be used for infants. 246 MDI with Spacer MDI with Spacer and Mask Photo Source: Del Mar Image Library; Used with permission 247 Let’s Review The nurse would prepare which site for an intramuscular injection to a 11 month-old? A. B. C. D. Dorsogluteal Deltoid Vastus lateralis Ventrogluteal 248 Pediatric Oncology Cancer is the leading cause of death from disease in children from 1 - 14 years. Incidence: 6,000 children develop cancer per year 2,500 children die from cancer annually Boys are affected more frequently Etiologic factors: environmental agents, viruses, host factors, familial/genetic factors Leukemia is the most frequent type of childhood cancer followed by tumors of the CNS system. 249 Oncology Stressful Events “Treatment is worse than the disease.” 1. Diagnosis 2. Treatment - multimodal 3. Remission 4. Recurrence 5. Death 250 Oncology Interventions 8 Surgery 8 Radiation Therapy 8 Chemotherapy 8 Bone Marrow Transplant 251 Stages of Cancer Treatment 1. Induction 2. Consolidation 3. Maintenance 4. Observation 5. Late Effects of Treatment • Impaired growth & development • CNS damage • Psychological problems 252 Pediatric Oncology Types of Childhood Cancers D D D D D D Leukemia Brain Tumors Wilm’s Tumor Neuroblastoma Osteogenic Sarcoma Ewing’s Sarcoma 253 Leukemias Most common form of childhood cancer Peak incidence is 3 to 5 years of age Proliferation of immature WBCs (blasts) May spread to other sites (CNS, testes) Types of Leukemia: Acute lymphocytic leukemia (ALL) • 80-85% of childhood leukemia • 95% chance of remission Acute nonlymphocytic Leukemia (ANLL) • 60-80 % chance of remission Treatment is chemotherapy: prednisone, allupurinol, selected chemotherapeutic agents 254 Leukemias CLINICAL MANIFESTATIONS • • • • • • • • Purpura, Bruising Pallor Fever Unknown Origin Fatigue, Malaise Weight loss Bone pain Hepatosplenomegaly Lymphadenopathy LABS & DIAGNOSTIC TESTS ↑ WBC’s (50-100) or Very low WBC’s ↓Hgb, Hct, Platelets Blast cells in differential BONE MARROW ASPIRATION LUMBAR PUNCTURE BONE SCAN possible 255 Brain Tumors Second most prevalent type of cancer in children Males affected more often Peak age 3 - 7 years Types: Medulloblastoma Astrocytoma Brain Stem glioma Look for S/S of increased ICP and area of brain affected 256 Wilm’s Tumor Also known as Nephroblastoma Large, encapsulated tumor that develops in the renal parenchyma (do not palpate abdomen!) Peak age of occurrence: 1 - 3 years Prognosis is good if no metastases- lungs first Treatment is surgery, chemotherapy and sometimes radiation 257 Neuroblastoma Highly malignant tumor – extracranial Often develop in adrenal gland, also found in head, neck, chest, pelvis Incidence: One in 10,000 Males slightly more affected From infancy to age 4 Often diagnosed after metastasis occurs Treatment includes surgery, chemotherapy and radiation 258 Bone Tumors Osteogenic Sarcoma: Occurs most often in boys between 10-20 yrs 10-20% 5 year survival rate Primary bone tumor of mesenchymal cell Treatment:surgery (amputation or salvage) and chemo Ewing’s Sarcoma: Occurs in boys between 5 - 15 years Primary tumor arising from cells in bone marrow Treatment is radiation and chemotherapy 259 Pediatric Oncology: Nursing Interventions CHEMOTHERAPY SIDE EFFECTS • Leukopenia (Nadir) • Thrombocytopenia • Stomatitis • Nausea/Vomiting • Alopecia • Hepatotoxicity • Nephrotoxicity NURSING INTERVENTIONS • HANDWASHING! • Monitor visitors • Monitor for infection • Meticulous oral care • Antiemetics ATC • Monitor Labs • Support/Teaching 260 Pediatric Oncology: Nursing Interventions • Supportive care for radiation treatment, focusing on skin care • Surgical interventions are based on location and type of surgery • Basic pre and postoperative care • Psychosocial care for patient and family – utilize Child Life and Social Services 261 Pediatric Oncology • Teach, teach, teach! • Support the child and family • Provide resources • Be honest • Include the child in the care planning Photo Source: Del Mar Image Library; Used with permission 262 Let’s Review In caring for the child with osteosarcoma, it is important for the nurse to inform the child and family of the treatment plan. Which would be appropriate? A. B. C. D. The affected extremity will have to be amputated. The child will only need chemotherapy. Both surgery and chemotherapy are indicated. Only palliative measures are taken. 263 Let’s Review The nurse assessing a child who is undergoing chemotherapy finds the child to be suffering from mucositis. Which intervention would be the highest priority? A. Meticulous oral care. B. Obtain dietician consult. C. Place the child on a full liquid diet only. D. Medicate for pain around the clock. 264 Let’s Review The priority nursing intervention in caring for a child with acute lymphocytic leukemia (ALL) during the child’s nadir period is: A. B. C. D. Handwashing. Monitoring lab results. Administering antiemetics. Monitoring visitors. 265 Death & Dying Child’s Response to Death: Infants & Toddlers: Do not understand Viewed as a form of separation Can sense sadness in others Preschooler: Death is temporary Viewed as sleep or separation Feel guilty and blames self Dying children may regress in behavior 266 Death & Dying School-Age: Have concept of irreversibility of death Fear, pain, mutilation and abandonment Ask many questions Feel death is a punishment May personify death (bogeyman) Will ask directly if they are dying Interested in the death ceremony Comforted by having parents and loved ones with them 267 Death & Dying Adolescent: Have an accurate understanding of death Death as inevitable and irreversible May express anger at impending death May find it difficult to talk about death May wish to leave something behind to remember them by May wish to plan own funeral 268 Death & Dying Parental responses to death: Major life stress Experience grief at potential loss of child Related to circumstances regarding child’s death (denial, shock, disbelief, guilt) Confronted with major decisions regarding care May have long term disruptive effects on family Bereaved parents experience intense grief of long duration 269 Communicating with the Dying Child and Family •Use child’s own language •Don’t use euphemisms •Don’t expect an immediate response •Communicate through touch •Encourage questions and expressions of feelings •Strengthen positive memories •Listen, touch, cry 270 Impending Death Care Guidelines Do not leave child alone Do not whisper in the room Touching the child is very important Let the child and family talk and cry Let parents participate in care as much as they are emotionally capable of doing Continue to read favorite stories or play the child’s favorite music Be aware of the needs of the siblings 271 Let’s Review Which intervention would be most helpful in supporting a dying child’s family as they cope with the various decision-making periods of a lengthy terminal illness? A. Encouraging the parents to take their child home to die. B. Encouraging the parents to go through all of the KublerRoss stages of dying as quickly as possible. C. Referring the child’s family to the hospital clergy service as soon as possible. D. Using active listening to identify specific fears and concerns of the child’s family members. 272 Types of Child Abuse M Neglect: Intentional or unintentional omission of basic needs and support M Physical Abuse: Is non-accidental injury to a child by an adult M Sexual Abuse: Forced involvement of children in sexual activities by an adult M Emotional Abuse: Withholding of affection, use of cruel and degrading language towards a child by an adult 273 Child Abuse M Reports of violence against children has almost tripled since 1976. M Many of the abused children are infants. “Red Flags” Fractures in infants Spiral fractures Injuries do not match story told NURSES ARE MANDATED REPORTERS 274 Child Abuse Neglect Physical or emotional maltreatment Failure to thrive Contributing factors may be ignorance or lack of resources Physical Abuse Minor or major physical injury (bruising, burns, fractures) May cause death Munchausen by Proxy (MSP) Shaken baby syndrome (SBS) Sexual Incest, molestation, child porn, child prostitution Emotional May be suspected, but difficult to substantiate Impairs child’s self-esteem and competence 275 Child Abuse Warning Signs Incompatibility between history of event and injuries Conflicting stories from various people involved History inconsistent with developmental level of child Repeated visits to emergency rooms Inappropriate response from child and/or caregiver Nursing Interventions Assess: Physical assessment and history of event, observe and listen to caregiver’s and child’s verbal and non-verbal communication Documentation: Complete CAR form and contact Child Protective Services, hospital documentation Support family and child: Social services, resources, teaching THE CHILD’S SAFETY COMES FIRST AND IS THE PRIORITY! 276 Let’s Review In caring for a 4 year-old with a diagnosis of suspected child abuse, the most appropriate intervention for the nurse is: A. Avoid touching the child. B. Provide the child with play situations that allow for disclosure of event. C. Discourage the child from speaking about the event. D. Give the child realistic choices to feel in control. 277 Let’s Review Which pediatric patient would most necessitate further investigation by the community-based nurse? A. An adolescent who prefers to spend time with friends rather than family. B. A toddler with dark bruises located on both legs. C. An infant with numerous insect bite marks and diaper rash. D. A preschooler with dirty knees and torn pants. 278 Photo Acknowledgement: All unmarked photos and clip art contained in this module were obtained from the 2003 Microsoft Office Clip Art Gallery. 279