My Substance Abuse Outline
advertisement

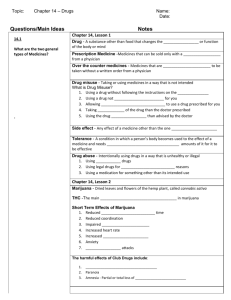
Substance Abuse Substance Abuse o The actual prevalence of substance abuse is difficult to determine o Detrimental effects of substance abuse include: Workplace injuries Homicide Motor vehicle accidents and fatalities Domestic abuse Child abuse and neglect o Affects males and females of all ages, cultures, and socioeconomic groups o Commonly coexists with (and complicates the treatment) of other psychiatric disorders Dual Diagnosis o Increasing numbers of babies are being born to substance-addicted mothers o Many people with emotional disorders or mental illness use drugs to self medicate o Many people abuse a combination of substances o Substances of abuse may be any chemical used therapeutically or recreationally o Commonly leads to physical dependence, psychological dependence, or both Etiology o Biologic factors Genetic vulnerability Neurochemical influences o Psychological factors Familial dynamics Coping Styles o Social and environmental factors Cultural Considerations o Wine is an integral part of Jewish religious rites o Some Native Americans tribes use peyote in religious ceremonies o Certain ethnic groups have genetic traits that either predispose them or protect them from developing alcoholism o Alcohol abuse plays a part in the 5 leading causes of death for Native Americans Diagnostic Classes o Alcohol o Amphetamines o Caffeine o Cannabis o Cocaine o Hallucinogens o Inhalants o Nicotine o Opioids o PCP o Sedatives, hypnotics, or anxiolytics Definitions o Substance abuse – using a drug in a way that is inconsistent with medical or social norms and it is done despite negative consequences o Substance dependence – tolerance, withdrawal, and unsuccessful attempts to try to stop using that drug. The word dependence means it’s a physiological need to use that drug. We use the drug to prevent withdrawal symptoms o Intoxication – the use of a substance that results in a maladaptive behavior o Withdrawal – a set of symptoms you can get when you are not getting the substance that your body is addicted to. Can range from HA to seizures o Detoxification – the process of safely withdrawing from that substance. Many people can’t detox by themselves, on their own. Onset/Clinical Course o Typically begins with the first episode of intoxication between 15 and 17 years of age o More severe difficulties begin in the middle 20s-30s Alcohol-related breakup of a significant relationship An arrest for public intoxication or driving while intoxicated Evidence of alcohol withdrawal Early alcohol-related health problems Significant interference with functioning at work or school o Blackout drinking in which the person continues to function but has no conscious awareness of their behavior at the time nor any later memory of the behavior o As the person continues to drink, they often develop a tolerance for alcohol; that is, they need more alcohol to produce the same effect o After continued heavy drinking, the person experiences a tolerance break, which means that very small amounts of alcohol will intoxicate the person o During the later course of alcoholism, when the person’s functioning definitely is affected, periods of abstinence or temporarily controlled drinking occur Alcohol o Central nervous system depressant o Overdose can result in vomiting, unconsciousness, and respiratory depression o Symptoms of withdrawal usually begin 4 to 12 hours after cessation or marked reduction of alcohol intake o Alcohol withdrawal usually peaks on the second day and is over in about 5 days o Very important to ask when their last drink was. You need to know when the withdrawal symptoms will start Alcohol Withdrawal o Withdrawal symptoms include: Coarse hand tremors, sweating, elevated pulse, elevated blood pressure, insomnia, anxiety, and nausea or vomiting Severe or untreated withdrawal may progress to transient hallucinations, seizures, or delirium – called delirium tremens (DTs) o Withdrawal symptoms monitored using an assessment tool Pharmacologic Treatment o Safe withdrawal from alcohol involves: Benzodiazepines to suppress withdrawal symptoms (Ativan, Librium, Valium) Vitamin B1 (thiamine) to prevent or to treat Wernicke’s syndrome and Korsakoff’s syndrome Thiamine is necessary for metabolism, effects nervous system, circulatory system, GI system. Vitamin B12 (cyanocobalamin) or folic acid for nutritional deficiencies Wernicke-Korsakoff Syndrome o These usually aren’t reversible… o Wernicke’s encephalopathy An inflammatory, hemorrhagic, degenerative, condition of the brain; characterized by lesions in several parts of the brain Double vision, involuntary rapid movements of eyes, paralysis of eyes, lack of muscular coordination, decreased mental function, peripheral neuropathy Caused by thiamine deficiency o Korsakoff’s syndrome (psychosis) A form of amnesia characterized by a loss of short-term memory and an ability to learn new skills; usually disoriented, may present with delirium, hallucinations, and confabulates to conceal the condition Can often be traced to a degenerative change in the thalamus as a result of a deficiency of B complex vitamins – especially thiamine and B12 Medical Complications of Alcoholism o Gastritis o Cirrhosis o Pancreatitis o Diabetes o Malnutrition o Esophageal varices o Peripheral neuropathy Sedatives, Hypnotics, and Anxiolytics o Central nervous system depressants Barbiturates, nonbarbiturate hypnotics, and anxiolytics o Benzodiazepines alone, when taken orally in overdose Romazicon given for overdose o Barbiturates, in contrast, can be lethal when taken in overdose; they can cause coma, respiratory arrest, cardiac failure, and death o Withdrawal symptoms occur in 6 to 8 hours or up to 1 week, depending on the half-life of the drug o Withdrawal syndrome is characterized by symptoms opposite of the acute effects of the drug: Autonomic hyperactivity (increased pulse, blood pressure, respirations, & temperature), hand tremor, insomnia, anxiety, nausea, and psychomotor agitation Seizures and hallucinations occur rarely in benzodiazepine withdrawal o Detoxification is managed by tapering To prevent seizures Stimulants: Amphetamines, Cocaine, Methamphetamine, etc. o Central nervous system stimulants o Overdoses can result in seizures and coma o Withdrawal occurs within hours to several days o Withdrawal syndrome: Dysphoria accompanied by fatigue, vivid and unpleasant dreams, insomnia or hypersomnia, increased appetite, psychomotor retardation or agitation, and depressive symptoms including suicidal ideation for several days o Stimulant withdrawal is not treated pharmacologically Psychological withdrawal is more severe than physiologic withdrawal Looks a lot like paranoid schizophrenia Formication – the feeling like there are bugs or whatever crawling under your skin. Also called “coke bugs” Cannabis (Marijuana) o Used for its psychoactive effects o Excessive use of cannabis may produce delirium or cannabis-induced psychotic disorder; overdoses do not occur o Withdrawal symptoms: Insomnia, muscle aches, sweating, anxiety, and tremors o Effects are treated symptomatically Opioids (narcotics) o Central nervous system depressants Demerol, morphine, heroine, oxycontin, methadone o Overdose can lead to coma, respiratory depression, pupillary constriction, unconsciousness, and death o Withdrawal: Short-acting drugs begin in 6 to 24 hours, peak in 2 to 3 days, and gradually subside in 5 to 7 days Longer-acting drugs begin in 2 to 4 days, subsiding in 2 weeks o Withdrawal symptoms: Withdrawal does not require pharmacologic intervention Administration of Narcan is the treatment of choice for overdose Methadone can be used as a replacement for heroin, serving to reduce cravings These have the least complicated withdrawal symptoms Hallucinogens o Distort reality and produce symptoms similar to psychosis including hallucinations (usually visual) and depersonalization Shrooms, LSD, mescaline, ecstasy Synesthia – blending of all the senses o Toxic reactions to hallucinogens (except PCP) are primarily psychological; overdoses as such do not occur; PCP toxicity can include seizures, hypertension, hyperthermia, and respiratory depression o Hallucinogens can produce flashbacks which may persist from a few months to 5 years “Bad trip” o Treatment is supportive: Isolation from external stimuli; physical restraints; for PCP, medications to control seizures and blood pressure; cooling devices; mechanical ventilation Inhalants o Inhaled for their effects o Overdose: Anoxia, respiratory depression, vagal stimulation, dysrhythmias Death may occur from bronchospasm, cardiac arrest, suffocation, or aspiration of the compound or vomitus People who abuse inhalants may suffer from persistent dementia or inhalant-induced disorders such as psychosis, anxiety, or mood disorders even if the inhalant abuse ceases o Withdrawal symptoms: none o Treatment: Support respiratory and cardiac functioning until the substance is removed from the body May present with mouth ulcers, confusion, ataxia Substance Abuse Treatment o Treatment based on concept that alcoholism/drug addiction are medical illnesses: chronic, progressive, and characterized by remissions and relapses o Settings Emergency department/medical or chemical dependency unit Outpatient/extended treatment Halfway houses o Programs AA/NA Individual and group counseling Pharmacologic Treatment o Has 2 main purposes: To permit safe withdrawal from alcohol, sedative/hypnotics, and benzodiazepines Prevent relapse o Relapse Prevention Antabuse – alcohol and studies being done for cocaine addiction Campral – new one for alcohol Methadone – used for heroine ReVia – opioid antagonist sometimes used to treat overdose Catapres – lessen effects of withdrawal Zofran – using in young males that are at high risk for alcohol dependence, also treatment for meth addiction, they’re doing studies to see these effects o Off-Label Uses Nursing Process o Info o o o o Antabuse – use for cocaine addiction Provigil – can become addictive itself Inderal – alcohol withdrawal Topamax – alcohol withdrawal The nurse may encounter patients with substance problems in various settings unrelated to mental health Seeking treatment of medical problems related to alcohol use Withdrawal symptoms may develop while in the hospital for surgery or an unrelated condition Be alert to the possibility of substance use in these situations and be prepared to make appropriate referrals Assessment History: chaotic family life, family history, crisis that precipitated treatment General appearance/motor behavior: depends on physical health; likely to be fatigued, anxious Mood/affect: may be tearful (expressing guilt and remorse), angry, sullen, quiet, unwilling to talk Thought process/content: minimize substance use, blame others, rationalize behavior, say can quit on their own Sensorium/intellectual processes: alert and oriented; intellectual abilities intact (unless neurologic deficits from long-term alcohol or inhalants) Judgment/insight: poor judgment while intoxicated and due to cravings for substance; insight limited Self-concept: low self-esteem, feels inadequate coping with life Roles/relationships: strained relationships and problems with role fulfillment due to substance use Physiologic considerations: may have trouble eating, sleeping; HIV risk if IV drug user Data analysis Nursing diagnoses common to physical health needs: Diarrhea Risk for injury Risk for infection Activity intolerance Self-care deficits Excess fluid volume Imbalanced nutrition: less than body requirements Nursing diagnoses common to psychosocial health needs: Ineffective denial Ineffective coping Ineffective role performance Ineffective family process Outcomes The patient will: Abstain from alcohol/drugs Express feelings openly and directly Accept responsibility for own behavior Practice non chemical alternatives to deal with stress or difficult situations Establish an effective aftercare plan Interventions Adequate pharmacological treatment Monitoring of vital signs Control nausea and vomiting Assess fluid and electrolyte balance Assess nutritional status Provide safe environment Assess for suicide potential Encourage participation in groups Do not reinforce feelings of worthlessness Help to see relapse as opportunity for learning Be firm and consistent –manipulation Set limits – demanding Enforce rules, help strengthen impulse control –acting out Place responsibility on patient – dependency Help patient make realistic self-appraisals and expectations – superficiality o Evaluation Is the patient abstaining from substances? Is the patient more stable in their role performance? Does the patient have improved interpersonal relationships? Is the patient experiencing increased satisfaction with quality of life? Elder Considerations o Estimates are that 30% to 60% of elders in treatment began drinking abusively after age 60 o Risk factors for late-onset substance abuse in elders: Chronic illness that causes pain; long-term use of prescription medication (sedative-hypnotics, anxiolytics); life stress; loss; social isolation; grief; depression; an abundance of discretionary time and money o Elders may experience physical problems associated with substance abuse more quickly Mental Health Promotion o Public awareness and educational advertising o Early identification of older adults with alcoholism o The College Drinking Prevention Program Substance Abuse in Health Professionals o Higher rates of dependence on controlled substances o Ethical and legal responsibility to report suspicious behavior o Texas Peer Assistance Program for Nurses (TPAPN) Texas Peer Assistance Program for Nurses Available for LVNs and RNs of Texas whose practice has been impaired due to the effects of psychiatric or substance abuse disorders Operates under state legislation, Chapter 467, Texas Health and Safety Code & NPA of Texas A project of the Texas Nurses Foundation TPAPN’s Mission Offer nurses life-renewing opportunities for recovery from substance use and psychiatric disorders Integrate nurses back into the profession, thus Protect the public, and Promote professional accountability TPAPN Serves in Two Complementary Ways As a voluntary, confidential & non-punitive alternative to BON investigation emphasizing rehabilitation & monitoring of nurses’ practice/recovery; and As a voluntary & non-confidential option under BON licensure discipline emphasizing rehabilitation & monitoring of nurses’ practice/recovery TPAPN Serves to… Keep good nurses with bad diseases who are motivated to find and maintain recovery while helping them to return to safe nursing practice – most often improved nursing practice. TPAPN serves… RNs and LVNs of Texas with at least one of the following diagnoses: o Substance Use Disorders (SUDS) Substance abuse Substance dependency (Alcoholism, prescription drug abuse or dependence, illicit drug abuse or dependence like cocaine, marijuana, crystal meth, opioids, etc.) Psychiatric Disorders o Anxiety disorders o Bipolar disorder o Major depression o Schizophrenia o Schizoaffective disorder Note: 8% of all TPAPN participants are psychiatric only How Does TPAPN Work? Holds nurses accountable for working a recovery program and obtaining appropriate support Must demonstrate good recovery for a minimum of 2 yrs (3 yrs of APN) Must demonstrate safe nursing practice by working as a nurse for at least 1 year of their participation Nurses should not have to lose jobs or licenses without first being offered the opportunity for education, treatment, and recovery for chronic, progressive, and potentially fatal diseases However, nurses whose psychiatric illness or substance use prevents them from practicing nursing safely must be referred to the BON Substance Abuse o Classic Signs Changes in behaviors & practice usually seen before physical changes are seen Co-workers observe pattern/change over time- deterioration Work is often the last thing “to go” High level of functioning before “hitting bottom” May justify use (abuse) through RX meds Increasingly isolated over time Denial! At work, but not “on the job” o Other Warning Signs Incorrect drug counts Excessive controlled substances listed as wasted or contaminated Reports by patients of ineffective pain relief from medications especially if relief had been adequate previously Damaged or torn packaging on controlled substances Unexplained absences from the unit Trips to the bathroom after contact with controlled substances Consistent early arrivals at or late departures from work for no apparent reason Psychiatric Impairment o Signs Chronic, depressed mood, lack of focus, crying… Difficulty completing tasks Increased absenteeism Mood swings – cyclical in nature Hyperactivity, grandiosity, pressured speech… Attention & memory deficits Anxiety that impairs practice, memory, etc. Rage or disruptive behaviors Bizarre (as in psychotic) behaviors Why Nurses are at risk o Genetic predisposition: individual (brain) susceptibility to substances of abuse o Environmental & Socio-cultural influences Family of origin (environment) e.g., development of adult children of alcoholic (enabling) personalities Cultural values, e.g., Western culture/medicine: Expectation for immediate gratification, pain relief. Our stressful habits & poor self-care are to be remedied by better pills… Unique Work Stressors, combined with access to controlled substances o Myth of Immunity: “I’m a nurse, not some uneducated loser on the street!” o Myth of Perfectionism: “I can do it all – and I have to do it all perfectly!” o Low self-esteem & poor self-care: Nurses end up meeting everyone else’s needs but their own! o Enabling by co-workers & administration: We may assume all is “OK” or fear confronting nurse until its too late Requirements of Participation o Qualified assessment psychiatrist o Appropriate treatment o Ongoing self-help group support o Random drug testing o Payment of participation &/or Board Order Fees o Released to RTW – by Treatment Provider & TPAPN o Demonstrate minimum 12 months safe practice o Minimum 2 year participation with compliance o Usually 1 relapse allowed before BON o 2 full participations typically permitted Self-Awareness Issues o Examine own beliefs and/or family behavior about alcohol and drugs o Recognize that substance abuse is a chronic illness with relapses and remissions o Nurse must be objective and reasonably optimistic