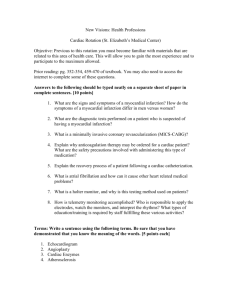
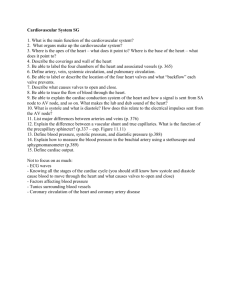
Cardiovascular System
advertisement

Cardiovascular Case Study Case Study Mr. Alex Borg is a 70 year old retired black male, who presented to the emergency department at 1000 on Saturday September 23rd via ambulance. He was accompanied by his wife. His primary complaints were of chest pain and shortness of breath. This was the Mr. Borg’s third visit to the emergency department in the last 2 weeks, with the same symptoms. On arrival, his chest pain was rated 9/10, and did not subside with rest. Vitals Upon Arrival • T – 35.9 oC • P – 118 bpm • R – 30 rpm • BP – 168/88 mm/Hg • SpO2 – 88% on RA Oxygen was applied by nasal prongs at 4L/min which brought his oxygen saturation levels up to 92%. Further clinical assessments were performed in order to confirm suspected diagnosis and treatment. The patient’s lungs were auscultated for decreased air entry and exit, but were clear throughout. Heart sounds were auscultated and a third sound, S3, was heard. Blood was drawn and sent to the lab for cardiac workup and routine chemistry. Peripheral edema was noted with +1 pitting around the ankles. Telemetry monitoring and a 12 lead ECG was performed. ECG results were obtained and showed the following rhythm. Medications administered: All other systems had no significant findings. An IV was started in the R forearm, N/S TKVO. • Nitrospray spray q 5 minutes x3 doses under the tongue beginning at 1005 • Aspirin 650mg PO given at 1005 • Shortly after medications were administered, Mr. Borg’s chest pain decreased to 5/10. • Mr. Borg was admitted to 4W Medical floor for observation. At that point a patient history was obtained with the following significant factors: – – – – – His mother died from a heart attack at age 53. His father had hypertension. He smokes 1 pack of cigarettes a day He consumes 4 or more alcoholic drinks a day He is obese • Wt. 109kg and ht. 5’9” – He has Type II Diabetes Mellitus Doctors Orders Upon Admission • Vitals q4h • Keep SpO2 >92% with 3L oxygen • Cardiac diet • AAT • IV TKVO NS 30mL/h • Daily in & outs • Telemetry • CXR • Repeat cardiac profile in 12 hours. • Daily CBC, BUN, Cr, Lytes • EC ASA 325mg po daily • Metoprolol 100mg po daily • Norvasc 2.5mg po daily • Nitrospray spray prn Diagnosis? Coronary Artery Disease with Anginal Episode What are coronary arteries? Coronary Arteries Cont’ Cholesterol • High density lipoprotein (HDL) – A protein bound lipid that transports cholesterol to the liver for excretion in the bile. – Composed of a higher proportion of lipids than the LDLss. – Exerts a beneficial effect on the arterial wall. • Low density lipoprotein (LDL) – Protein bound lipids that transport cholesterol to tissues in the body. – Composed of a lower proportion of protein than the HDLs. – It exerts a harmful effect of the arterial wall. Coronary Artery Disease (CAD) • LDLs travel through the blood stream and adhere to the walls of the coronary arteries. • Over time, a fibrous layer composed of platelets and other clotting factors envelope the fatty deposits and form a plaque. Coronary Artery Disease (CAD) • Eventually the plaque buildup becomes so large that the coronary arteries become occluded and blood is unable to pass through. The lack of blood decreases the amount of oxygen that is being delivered to the myocardial cells and myocardial tissue become ischemic. • An occlusion can happen 2 ways: – – The vessel becomes totally occluded and blood is unable to pass through at all. A piece of the plaque breaks off the vessel wall, called a thrombus, and occludes a smaller coronary artery. How CAD Causes Ischemia Coronary Artery Disease Risk Factors Modifiable • • • • • • • Dyslipidemia Hypertension Smoking Diabetes Type II Obesity Sedentary Lifestyle Alcoholism Non-Modifiable • • • • • Advanced age Males under 60 Race Genetics Diabetes Type I Diabetes • Diabetic dyslipoproteinemia includes: – increased LDL – increased triglycerides – deceased HDL • Glycation of LDL protein decreases uptake by the liver, increases hepatic synthesis of LDL, and increases LDL oxidation. • Smoking and diabetes also increase LDL oxidation. • Oxidized LDL is toxic to endothelial cells and causes smooth muscle proliferation and abnormal vasoconstriction. Hypertension • Mr. Borg is currently in a hypertensive state. He has never been diagnosed with hypertension but may have unknowingly had it for years. Hypertension causes hypertrophy of the myocardial cells which increases the myocardial need for coronary flow. Smoking • Mr. Borg has been a smoker for 40 years. He smokes approximately 1 pack a day. Nicotine in the cigarettes stimulates the release of catecholamines which increases heart rate and vascular constriction. This causes blood pressure to rise and the cardiac workload and need for oxygen to increase. Obesity • Mr. Borg is an obese man (112 kg). He has lived with obesity for many years. HDL (good cholesterol) levels decrease with obesity. Obesity also causes the heart to increase in size, and therefore increases the workload of the heart. This makes it more difficult to pump blood to the body. Alcohol • Mr. Borg has been ingesting 4 or more alcoholic drinks each day for the past 35 years. • Alcohol ingestion increases body weight, LDL levels, and blood pressure which are all other leading causes of CAD. Clinical Manifestations • Chest pain from myocardial ischemia (angina) – Feels like heaviness or pressure – May radiate to the neck, jaw, left arm, shoulder, back, or right arm • Pallor • Diaphoresis • Dyspnea Angina • When a blood vessel becomes occluded for a long period of time, blood flow is limited and myocardial tissue becomes ischemic. • Length of occlusion time is approx. 10-20 minutes. • The thrombus then breaks apart or vasodilation occurs and myocardial perfusion returns before significant tissue necrosis occurs. Nursing Interventions • Improving respiratory function – Monitor vital signs – Bedrest or sitting until pain subsides – Oxygen if SpO2 levels are low. • Reducing anxiety – Develop a trusting relationship – Provide privacy – Reassure patient • Improving cardiac flow – Elevate head of the bed – Monitor fluid volume status – Monitor peripheral pulses Treatment and Evaluation • 3rd heart sound, S3 was heard on auscultation – This indicates left ventricle failure • ECG and telemetry • Laboratory tests Telemetry • The process of continuous electrocardiographic monitoring by the transmission of radiowaves from a batteryoperated transmitter worn by the patient. • Anagram: – L: Smoke (black) over fire (red) – M: White on the right – R: Bear (Brown, on bottom) in the bush (green, on top) Nitrates - Nitrospray • Act on the blood vessels in venous circulation and the coronary arteries • Cause generalized vascular and coronary vasodilation which causes: – Increased blood flow through the coronary arteries into the myocardial cells. – Decreased cardiac preload and afterload – Decreased myocardial oxygen demand Side Effects: • Headaches from vasodilation • Hypotension • Dizziness and weakness • Faintness *Be careful when using with other vasodilators, Viagra and alcohol because together they can enhance the effects of hypotension. Beta-Adrenergic Blockers – Metoprolol • Act on the B1 receptor sites and decrease the effects of the SNS by blocking the release of catecholamines (epi & norepi) causing: – Decreased heart rate – Decreased blood pressure – Decreased myocardial oxygen demand – Decreased anginal pain Side Effects • Decreased pulse • Decreased blood pressure • Bronchospasm • Behavioural repsonses Calcium Channel Blocker - Norvasc • Calcium activates the myocardial cells to contract, increasing cardiac workload and oxygen demand. • When these channels are blocked the heart rate slows and the demand for oxygen is decreased. Side Effects • Headache • Hypotension • Dizziness • Flushing of the skin • Reflex tachycardia • Liver and kidney changes Anti-Coagulants - Aspirin • Aspirin prevents platelet activation and is used to inhibit clot formation. • Aspirin reduces the incidence of MI and death in patients with CAD. • Aspirin does not dissolve clots that are already present, but it works prophylactically to prevent clots from forming or enlarging. • Aspirin will also help to reduce the pain a patient is experiencing because it is also a non-opioid analgesic. Side Effects • GI bleeding • Increased bleeding time • Anemia from bleeding • Anaphylaxis • Heartburn, N & V, abdominal pain • Hepatotoxicity While on the floor for the past 2 days, Mr. Borg has been stable with no complaints of chest pain or shortness of breath. Lab reports and CXR came back with no significant findings. Mr. Borg is ready to be discharged tomorrow if no complications occur. • At 1235, Monday September 25th, Mr. Borg’s wife approaches the nursing station in a frantic state. • She states “My husband doesn’t feel very well. He says he feels like he is dying.” Signs and Symptoms What do we see? • Mr. Borg is sitting at the side of his bed, clutching his chest. • He is diaphoretic and cyanotic around his lips and nail beds. • He has obvious dyspnea because he is gasping for his breath • He seems quite anxious and restless • Upon palpation, his skin is cool and clammy. Vitals • T – 37.9 • P – 180 bpm • R – 30 rpm • BP – 120/70 • SpO2 – 90% on 3L/min Assessments and Interventions • Oxygen is increased to 5L/min • Heart auscultated – a third and fourth heart sound are heard, S3 and S4 • Lung ausculation – decreased air entry and exit, chest is clear. • Elevate the head of the bed to 45 degrees, semi-fowlers position Medications • Nitrospray spray sl q5min x3 • After nitrospray has been administered, Mr. Borg’s chest pain is not relieved • His ECG shows the following: ECG ST elevation Altered Q waves Inverted T waves • Altered Q waves – When a thrombus becomes permanently lodged in the coronary artery the infarct (tissue necrosis) spreads from the endocardium through to the epicardium. This results in altered Q waves. • ST Elevation – Myocardial injury also causes ST segment changes. The injured myocardial cells depolarized normally, but repolarize more rapidly then normal cells, causing the ST segment to rise at least 1mm above the isoelectric line. • Inverted T Waves – Myocardial injury causes the T wave to become enlarged and symmetric. As the area of injury becomes ischemic, myocardial repolarization is altered and delayed, causing the T wave to invert. Diagnosis? Acute Myocardial Infarction Myocardial Infarction • Plaque progression, disruption, and subsequent clot formation is the same for myocardial infarction as it is for other acute coronary syndromes, such as angina and coronary artery disease. – The same process occurs, but happens along a different point of the continuum. • In an acute MI, the thrombus is lodged for a prolonged period of time, depriving the cells of oxygen and causing cellular injury. The longer the deprivation of oxygen, there is more tissue necrosis that occurs. Cardiac Tissue Surrounding the Infarct • Myocardial stunning – Temporary loss of contractile functioning • Hibernating myocardium – Tissue that is persistently ischemic and undergoes metabolic adaptation • Myocardial remodeling – Causes myocyte hypertrophy and loss of contractile function Functional Changes Post MI 1. Decreased cardiac contractility with abnormal wall motion 2. Altered left ventricular compliance 3. Decreased stroke volume 4. Decreased ejection fraction 5. Increased left ventricular end diastolic pressure 6. SA node malfunction 7. Dysrhythmias and heart failure often follow MI “Time is Muscle!” • Within 8 seconds oxygen reserves of the myocardial cells are used up, glycogen stores are decreased, and anaerobic metabolism begins. This can put the patient into a state metabolic acidosis. • After 8 – 10 seconds of decreased blood flow the affected myocardium becomes cyanotic and cooler. • After 30 – 60 seconds of hypoxia, ECG changes are visible. • Even if cells are metabolically altered and dysfunctional, they can be saved if blood flow returns within 20 minutes. • Within an hour, tissue necrosis results in the release of certain intracellular enzymes through the damaged cell membranes. These enzymes are evident on the laboratory results. Laboratory Findings Creatinine Kinase (CK-MB) • This is a cardiac specific enzyme found mainly in cardiac cells and, therefore, rises only when there is damage to these cells. • It is the most specific index for the diagnosis of an MI • Levels start to increase within a few hours and peak within 24 hours of an acute MI • Normal values: – 5 – 100 IU/L • Patient value – 152 IU/L • This level is elevated, clearly indicating Mr. Borg has had an MI Laboratory Findings Myoglobin (Myo) • Heme protein that is found in cardiac and skeletal muscle that helps to transport oxygen. • Levels begin to increase within 1 – 3 hours, and peak within 12 hours from the onset of symptoms. • If these values are negative it is a good indicator that the patient has not had an acute MI • If the first test is negative, repeat the test in 3 hours. If the second test is negative it is confirmed that the patient did not have an MI • Normal Values – <100 ng/mL • Patient Value – 154 ng/mL Laboratory Findings Troponins • Cardiac and skeletal muscle is controlled by intracellular calcium concentrations. • When calcium levels rise, the muscles contract, and when the levels fall the muscles relax. • Long filament that calcium binds to. • There are 3 types of trops: – Trop T – Trop I – Trop C • Trop levels are normally quite low so even slight elevations are indicative of heart damage. • Levels of TropT will begin to elevate within 4 hours of myocardial damage and are normally elevated for 1 – 2 weeks postdamage. • Normal Values – <0.1 ng/mL • Patient Values – 0.15 ng/mL Laboratory Findings Serum Glucose Electrolytes • Arterial occlusion causes the myocardial cells to release catecholamines. • Catecholamines mediate the release glycogen, glucose, and stored fat from body cells. • These levels are increased on lab values. • Oxygen deprivation is accompanied by electrolyte disturbances • Normal values • Normal Values – 3.9 – 6.1 • Patient Values – 7.8 – – – – Loss of K Loss of Ca Loss of Mg These electrolytes are released into the blood stream and are evident on lab results. – Na: 125 - 145 – K: 3.5 – 5.0 – Mg: 0.74 – 1.23 • Patient Values – Na: 152 – K: 5.3 – Mg: 1.36 Laboratory Findings White Blood Cells • WBC levels increase with tissue necrosis and inflammation of the heart. • Specifically the neutrophils will have the greatest increase. Normal Findings (Neutrophils) – 0.54 – 0.75 Patient Value – 0.97 Interventions Medications • Anti-Platelet/Anti-Coagulant – Aspirin 650mg PO • ACE Inhibitor – Altace 5mg PO • Beta - Adrenergic Blocker – Metoprolol 100mg IV • Calcium Channel Blocker – Norvasc 2.5mg PO • Analgesic – Morphine • Streptokinase or rPA– as per protocol Streptokinase or rPA • What is it? – Sterile, purified preparation of the bacteria protein group C (beta)-hemolytic streptococci. • What does it do? – Acts with plasminogen to produce an “activator complex” that converts plasminogen to plasmin. – Plasmin degrades fibrin clots, fibrinogen , and other plasma proteins. rPA • Goal of the therapy: – The goal of thrombolytic therapy is to dissolve and lyse the thrombus in the coronary artery. – This allows blood to reperfuse through the coronary arteries, minimizing the size of the infarction and preserving ventricular function. rPA • Why is it needed? – Lysis of intracoronary thrombi – Improvement of ventricular function – Reduction of mortality associated with MI – Reduction of the size of the infarct – Reduction of CHF related to MI • Who can’t get thrombolytic therapy? – Active internal bleeding – Recent CVA – Uncontrolled hypertension • Adverse reaction – – – – Bleeding Arrhythmias Hypotension Cholesterol embolism rPA • What are the contraindications? – Recent major surgery – Recent gastrointestinal bleeding – Recent trauma needing CPR – Hypertension >180/>110mmHg – Age >75 – Pregnancy – Bleeding conditions Streptokinase Route Dosage Intravenous infusion 1, 500, 000 IU within 60 minutes Nursing Interventions • Ineffective cardiopulmonary tissue perfusion related to reduced coronary blood flow – The patient’s description of chest discomfort and other symptoms – Obtain a 12 lead ECG during the symptomatic event – Administer oxygen – Administer medication therapy – Ensure physical rest and ensure a restful environment • Potential ineffective air exchange related to fluid overload – Assess for abnormal heart sounds, and abnormal breath sounds – Teach patient to adhere to diet and activity perscription • Potential ineffective peripheral tissue perfusion related to decreased cardiac output – Observe for hypotension, tachycardia, activity intolerance, reduced urine output, cool, moist, cyanotic extremities. • Anxiety related to fear of death, change is health status. – Assess patients level of anxiety – Assess need for spiritual counseling – Allow patient to express anxiety and fear – Allow for flexible visiting hours – Encourage active participation in cardiac rehab – Teach stress reduction techniques. ICU • Mr. Borg is transferred to ICU following his MI and is placed under close monitoring • His condition deteriorates… Mr. Borg’s heart rhythm changes and he suddenly goes into SVT (supraventricular tachycardia) with a rate of 186 beats per minute (bpm). The physician orders adenosine (Adenocard) 6 mg IV. After no change in his heart rate or rhythm, the doctor orders an additional dose of adenosine of 12 mg. This bolus of adenosine administered IV push converts him briefly to normal sinus rhythm but then Mr. Borg’s rhythm changes back to SVT. Mr. Borg reports increased chest pain and shortness of breath. He is cyanotic with no palpable blood pressure. A Diltiazem drip is ordered and initiated. Blood gases are drawn as well. SVT • Supra = above • Ventricle is contracting too soon. There is not enough blood in the ventricle = dec. card output also the heart needs more oxygen to accommodate the increased HR. • The use of extra fibres in and around the AV node • The impulse travels from the SA to the AV and down into the ventricles but then back up via these extra fibres causing more contractions then is necessary. Drugs • Adenosine: – Antiarrythmic – Slows AV conduction • Diltiazem: – Ca channel blocker – Inhibits movement of Ca across membrane of heart muscle cells resulting in depression of impulse, slowing HR – Also dilates coronary arteries which dec. heart work In ICU, Mr. Borg’s hypotension and tachycardia persisted and a low-dose dopamine drip is initiated at 2 ug/kg/min. Mr. Borg becomes more hypotensive, tachycardic, and hypoxic. He is then intubated and placed on a ventilator with 100% oxygen. Furosemide (Lasix) 80 mg and Procanamide (Pronestyl) 500 mg IV bolus are administered. What diagnosis would you give poor Mr. Borg? Cardiogenic Shock Cardiogenic Shock • 80% of those who develop, will die. • What is it? – impaired muscle action – blood is inadequately pumped through the heart • This results in back-up of blood. • Cardiogenic shock occurs when 40% or more of myocardium is damaged (usually left ventricular). So What’s the Problem? • Right sided heart interference: • When the shock is due to right-sided heart failure, back-up will be evidenced as: – jugular venous distention – increased CVP So What’s the Problem Cont’? • Left sided heart interference: • When the shock is due to left-sided failure, blood backs up into the pulmonary circulation resulting in: – pulmonary edema – crackles in the lungs Cardiogenic Shock Cont’ • Causes: – Mechanical – Obstructive Mechanical Causes • MI – systolic dysfunction: inability of heart to pump blood forward • Valvular insufficiency due to disease or trauma (e.g. stenosis, regurgitation) • Cardiac dysrhythmias • These events cause the following which lead to cardiogenic shock: – decreased myocardial contraction – diminished cardiac output Obstructive Causes • Pulmonary emboli – travels through venous system – lodges in right side of heart in the pulmonary artery • Pericardial tamonade: – accumulation of blood in the pericardial space compresses the myocardium and interferes with the myocardium’s ability to expand – inability of heart to fill during diastole • Tension pneumothorax – significant amount of air in the pericardial space compresses heart and great vessels Cardiogenic Shock Cont’ • What do you think this patient will look like? • Clinical Manifestation: – systolic blood pressure significantly below client’s normal blood pressure – diaphoresis – tachycardic – tachypneic – signs of peripheral hypoperfusion (cyanosis, pallor, decreased capillary refill time, cold clammy skin) Clinical Manifestations Cont’ – decreased renal perfusion will result in sodium and water retention and therefore decreased urinary output – signs of decreased cerebral perfusion (restlessness, delirium, anxiety) So What Do You Want To Do For This Patient? • Overall goal? – to restore blood flow to the myocardium Nursing Interventions • Assess: – chest pain – vital signs – 12 lead ECG – monitor response to medications given – be calm and provide care efficiently to reassure patient/reduce anxiety – limit visitors Nursing Care Plan For Mr. Borg Assess Chest pain: Location Duration Quality Intensity Presence Radiation Precipitation Alleviation Scale 1-10 Diagnosis Plan/Goal Intervene Altered pain level related to discomfort due to myocardial infarction as evidenced by patient describing pain 3-10 and holding chest Evaluate Patient will be Administration Patient free of chest of verbalized that pain within 15 nitroglycerine, pain had to 20 minutes lasix, subsided from after adenosine a 8/10 to a administration 3/10 within 15 of drug therapy minutes of medication So What Do You Want To Do For This Patient? • Some laboratory values: – Cardiac Enzymes – Chest X-ray – ECG – Echocardiogram – IV, vitals, foley, meds (including something for pain; usually Morphine) but why must we be careful with how much Morphine we give Mr. Borg??? So What Do You Want To Do For This Patient? • Angioplasty with stenting • Until these can be done, the heart must be supported to optimize stroke volume and cardiac output by... Management of Cardiogenic Shock • Fluid challenge – 300ml of NS or Ringer’s to rule out hypovolemia (unless CHF or pulmonary edema) • Insert CVP catheter to monitor: • cardiac output, pulmonary artery pressure, pulmonary capillary wedge pressure • Administer inotropics (e.g. dopamine) • Administer vasodilators (e.g. nitro, calcium channel blockers, morphine) Management of Cardiogenic Shock Cont’ • Administer Diuretics (lasix) • Beta blockers (propranolol) • Intra-aortic balloon pump or external counterpulsation device Prevention of Cardiogenic Shock • Primary: – teach patients the importance of diet and exercise to minimize risk factors • Secondary: – provide oxygen – administer inotropics and vasodilators • Tertiary: – provide intra-aortic balloon pump – administer inotropics and vasodilators • Mr. Borg’s heart eventually improves a little. His heart rate is 140 bpm and the systolic BP is around 100 mm Hg while he is on 9 ug/kg/min of dopamine. A repeat ECG reveals that the distal two thirds of the left ventricle is akinetic. Mr. Borg is scheduled to have a right and left heart catheterization at 13:00 today. The results of the cardiac catheterization reveal 100% occlusion of the left coronary artery and severe diffuse disease of the left anterior descending coronary artery. The physicians have determined that he is a poor surgical candidate and plan to treat him medically. Over the next several days, Mr. Borg’s blood pressure stabilizes and he is weaned off the dopamine. The Furosemide is changed to an oral dose and the potassium is reduced to 10 mEq po tid. Mr. Borg is also digitalized and will be maintained on Digoxin 0.25 mg qd. His resting heart rate has been approximately 70 bpm. Mr. Borg is also extubated and placed on a no added salt, low fat diet. He is to begin a cardiac rehabilitation program. The physician is planning to discharge him tomorrow following a recovery treadmill test. Dopamine • To raise blood pressure by increasing peripheral resistance • Acts on norepinephrine and dilates vessels in kidneys to maintain perfusion (can be detrimental to the kidneys if used for long periods of time). Digoxin • Better blood flow in the microcirculation • To treat CHF, increase the force of contractility • Always check apical pulse for 1 minute Why was Mr. Borg intubated? Lasix • Loop diuretic • Inhibits the resorption of Na and Cl from proximal and distal loops of henle • Fluid may settle in the lungs due to back up from heart • May promote the loss of K+ Benazepril (Ace inhibitors = pril, Beta blockers = lol) • Blocks angiotensin I to angiotensin II which vasoconstricts leading to decreased BP Misc. • Rhonchi = dry rattle • Rales = crackle (non-musical) • Thiamine = Vitamin B1 – Breakdown carbs for use Cardiac Rehab • When the patient is free of symptoms cardiac rehab is initiated. • What is it? – Targets risk reduction by • Education • Individual and group support • Physical activity Cardiac Rehab • Goal? – For a patient with an MI to extend and improve quality of life. – Limit the effects and progression of plaque build-up – Return patient to pre-MI lifestyle – Prevent another cardiac episode • How will it happen? – – – – Encouraging activity and physical conditioning Education Counseling Behavioural interventions Cardiac Rehab • Phases of rehab: – Phase 1: diagnosis of MI • Low level activities and initial patient and family education • Ex: when to call 911, medications, activity-rest balance, follow-up appointments. – Phase 2: After discharge • Supervised, ECG monitored, exercise training • Counseling re: lifestyle changes – Phase 3: maintaining cardiovascular stability • Self directed • Build on the accomplishments of the previous phases What lifestyle changes can he make? When did the patient change from a stable state to an unstable state? • How can you imagine he feels going home knowing that he’s a ticking time bomb? • What impact does that have on his family and state of mind?