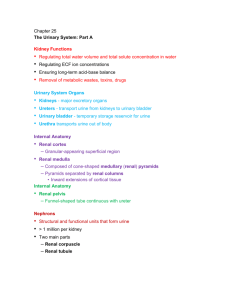
The Urinary System Chapter 18
advertisement
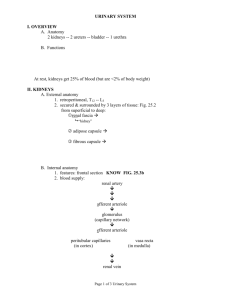
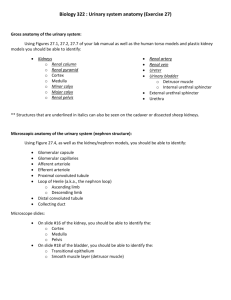
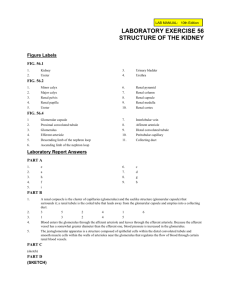
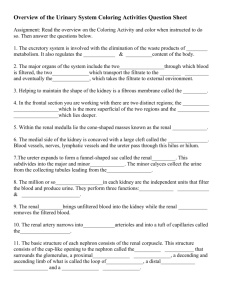
The Urinary System Chapter 26 The organs of the urinary system include: Functions of the urinary system (all done by kidneys): Regulate the volume, concentration, pH and content of blood Eliminate metabolic wastes as urine 3 processes occur within the kidneys to accomplish these goals Filtration (F) – Pressure (blood pressure) forces some fluid (plasma) and small substances from blood to renal (kidney) tubules. Results in the formation of “filtrate” in the renal tubules; approx. 180 liters filtrate/day Reabsorption (R) – Movement (by passive & active means) of most fluid & many solutes from renal tubules back into the blood; approx. 99% filtate reabsorbed Secretion (S) – Selective movement of specific substances (e.g. H+, K+) from blood to tubules blood Blood vessels (capillaries) F filtrate R Renal tubules Filtered blood S urine Gross Anatomy of the Kidneys Retroperitoneal organs Left kidney more superior than right (due to liver) Notch at medial border (hilus/hilum) for renal artery & vein, ureter Each kidney surrounded by 3 layers of CT: renal capsule – innermost layer of dense CT adipose capsule – middle layer protecting & insulating kidneys renal fascia – outer layer holding kidneys in place in abdominal cavity Internal Anatomy of the Kidneys Cortex Medulla where urine formation occurs pyramids renal papillae renal columns Pelvis - collecting basin minor calyces major calyces renal pelvis Microscopic Anatomy of the Kidneys Functional unit of the kidneys is the “Nephron” Nephron = renal corpuscle + renal tubules Most (85%) nephrons classified as “cortical nephrons” – corpuscle & most of tubule located within cortex Some (15%) classified as “juxtamedullary nephrons” – corpuscle at junction of cortex & medulla & loop of nephron extends into medulla Renal corpuscle – 1st part of the nephron; site of filtration; comprised of glomerulus – capillary network Bowman’s (glomerular) capsule – double layered capsule of epithelial tissue (inner visceral layer/outer parietal layer), surrounding glomerulus Bowman’s capsule (parietal (capsular) layer) Filtration occurs across “endothelial capsular (filtration) membrane” – junction between glomerular endothelium & podocytes; results in formation of “filtrate” in capsular space capsular space glomerulus Visceral layer of Bowman’s capsule (podocytes) Representative Nephron proximal convoluted tubule Filtrate from renal corpuscle will move into proximal convoluted tubule (PCT) loop of Henle distal convoluted tubule (DCT); and then into a collecting system of tubes (connecting tubule collecting duct papillary duct minor calyx) distal convoluted tubule reabsorption NEPHRON Secretion, some reabsorption COLLECTING SYSTEM renal corpuscle filtration collecting duct variable secretion &/or reabsorption Loop of Henle H2O solutes filtrate more reabsorption Connecting tubule papillary duct delivery of urine to minor calyx Blood supply to kidneys (Cortical radiate arteries) Efferent arteriole glomerulus Afferent arteriole Efferent arterioles branch into a second capillary network, the peritubular capillaries, which surround the renal tubules. The peritubular capillaries which surround the tubules of juxtamedullary nephrons are longer & straighter, therefore known as vasa recta Reabsorption & secretion occur between the renal tubules & peritubular capillaries Peritubular capillaries venules interlobular veins arcuate veins interlobar veins renal vein Juxtaglomerular Apparatus (JGA) Extremely important to regulate the rate of filtration that occurs at the glomerulus (glomerular filtration rate “GFR”) Macula densa To regulate glomerular BP, we have a feedback system – the juxtaglomerular apparatus (JGA) JGA = Juxtaglomerular cells juxtaglomerular cells of the afferent arteriole – recognize if renal BP is too low & then can respond macula densa cells of the distal convoluted tubule – recognize if decreased filtrate produced or too many solutes within filtrate & then can respond Histology of the kidneys Once urine is formed, it will move from the pelvis of the kidneys into the ureters retroperitoneal, muscular tubes running from kidneys to urinary bladder lined with transitional epithelium transports urine primarily by peristalsis Hollow muscular organ that temporarily stores urine prior to “micturition” Lined with mucosa of transitional epithelium with rugae Muscularis of 3 layers of smooth muscle known as “detrussor muscle” Internally have “trigone” – triangular area formed by openings of ureters & urethra Micturition reflex – stretch receptors in wall of bladder stimulate smooth muscle of detrussor muscle (involuntary); stimulation of internal urethral sphincter (involuntary) & external urethral sphincter of skeletal muscle (voluntary) Urinary bladder Histology of bladder & ureters muscularis Transitional epithelium Ureter Urinary bladder Urethra Transports urine out of body Inner urethral sphincter of smooth muscle; external urethral sphincter of skeletal muscle Anatomically different in men & women