Evaluation of passive ROM in a child with CMD
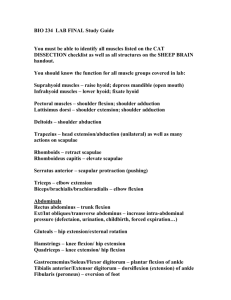
advertisement

Evaluation of passive ROM in a child with CMD Robyn Smith Dept. of Physiotherapy UFS 2012 Evaluation of passive ROM in a child with CMD It is essential to use your observational skills to determine what ROM and muscle lengths need to be assessed in a patient It is also essential that ROM and muscle lengths are assessed correctly accurately and safely It is crucial to note the available ROM in degrees or as a fraction Also clearly not the restricting factor e.g. joint, capsule, muscle, tone etc. Causes of deformities The cause of deformities in children with CMD is extensive and deformities may even result due to a combination of the following factors; Immobility Hypertonicity/ spasticity Hypotonicity Muscle weakness and imbalances Asymmetry Stereotypical (habitual) movement patterns Growth related factors e.g. difference in bone lengths Biomechanical issues Abnormal/ pathological reflex activity e.g. TLR, ATNR Neck Neck flexion One hand on occiput Other hands index finger on the chin and the middle finger under chin Make sure of the correct alignment of the cervical spine (chin tuck) Provide slight traction and provide high cervical flexion Restricted by tight neck extensors Neck extension Child in supine Index finger placed between the vertebrae lift the hand up so that cervical extension is done Repeat at the various levels of the cervical spine Restricted by tight neck flexors Side flexion Child in supine Neutral position of cervical spine Hands are placed both sides of the head/jaw Do side flexion of the neck Ensure that no rotation occurs Make sure that the child does not compensate with elevation of the shoulder on the side tested Repeat to the other side and compare ROM Restricted by tight upper fibres of m. trapezius Neck rotation Child sitting or in supine Hand are placed on sides of the head/jaw to which want to rotate to Other hand on the occiput Do rotation of the neck Make sure that the child is not compensating with lateral flexion Often restricted Restricted by tight SCM Trunk Trunk flexion Children that have increased tone in their m. pectoralis or those that make excessive use of flexion patterns of the UL and trunk are at an increased risk of developing a thoracic kyphosis Child is to be seated on a block/end of a roller. Allow the child to do trunk flexion, with the head and arm lowered between legs Your hand on the child’s arms and thoracic spine In the case of a smaller child of an extremely spastic child one can even observe flexion in side lying or picking the child up in a flexed position Restricted by shortened back extensors e.g. erector spinae and multifidus Limited by excessive extensor tone over the trunk Trunk extension In a child neutral spine extension is found Allow the child to sit over a roller Support the arms in 900 shoulder flexion Place one hand on the thoracic spinous process and press downwards towards the pelvis, the arms should naturally lift slightly If the child has severe flexor spasticity this can be tested in prone over a roller . In a smaller child the legs can be lifted off the supporting surface with one hand under the hips/pelvis and the other hand on thoracic vertebrae Restricted by shortened trunk flexors ie. Mm. abdominals, especially rectus abdominus Lateral flexion Lateral flexion ROM is greater in the lumbar spine, and less in the thoracic spine area due to the ribcage Child sitting on roller/block Neutral position spine Provide pressure on the lower ribcage in the direction of the opposite hip Whilst doing a weight shift In the case of very limited side flexion lift you can do side flexion by giving traction to the arm in ER, give counter pressure to the scapula Restricted by shortened abductors and quadratus lumborum on the opposite side Trunk rotation Rotation in the thoracic spine is approximately 90 0 and less in the lumber region 12 0 Child sitting on roller/block Neutral position spine Ensure that the pelvis is stabilised to prevent pelvic rotation to compensate Sit behind the patient Place one hand on the abdomen and the other on the thoracic spine Evaluate at the various levels of the spine: Arms side = upper trunk rotation Arm crossed at 90 0 shoulder = mid trunk rotation and Arms elevated above 90 0shoulder flexion =lumbar rotation Restricted by vertebral or muscle stiffness Scapula Scapula Child in side lying Hips and knees flexed, neural spine Assess scapula elevation, depression, protraction, retraction, and rotation Glenohumeral joint Glenohumeral joint Shoulder flexion Child in supine Observe gleno-humeral and scapula movement Avoid compensatory shoulder elevation Elbow should be in extension Restricted by tight shoulder extensors ie. Latissimus dorsi Shoulder extension Child in supine Observe glenohumeral and scapula movement Avoid compensatory shoulder elevation Elbow should be in extension Restricted by tight shoulder extensors Medial and lateral rotation Child in supine Shoulder in 450 flexion Avoid compensatory shoulder elevation Elbow should be inflexion Lateral rotation restricted a tight mm. pectoralis, teres major, subscapularis and latissimus dorsi Medial rotation restricted by a tight mm. infraspinatis and teres minor Horizontal abduction Child can be in supine or in sitting If seated ensure trunk is stable Arm is to be abducted horizontally prevent compensatory movements of shoulder elevation and protraction Restricted by a tight m.pectoralis Elbow Elbow flexion and extension in supine Stabilise the upper arm Do elbow flexion and extension If elbow extension is limited it most likely due to tight m. biceps Supination and Pronation in supine Perform supination and pronation with the elbow flexed and extended Wrist Wrist flexion, extension and deviation Stabilise the forearm Provide traction, especially in the case of a stiff wrist When assessing wrist extension make sure that you grasp close to the wrist joint, if you grasp the distal hand you run the risk of hyper-mobilising the carpal bones Wrist extension is often restricted by shortening of the long flexor muscles especially in the case of patients with increased flexor tone and fisting Hand Hand Be vary careful when assessing the ROM at the hand Do not do supination of the hand as this may damage the carpal bones and/or hyper-mobilise them In a closed or fisted hand where the long flexors are shortened or there is excessive flexor spasticity do not pull the finger out as the MCF joint is easily hyper-mobilised and the muscles overstretched, first make use of sweep taping to inhibit the flexor tone. Once you have got the hand slight open one can then work from the inside of the hand out. In case of palmar thumbing be careful not to pull the thumb out of the palm of the hand this hypermobilises the MCF joint. Provide enough stability to ensure that the correct joint and movement is being assessed. Pelvis and lower trunk Pelvis and lower trunk Child in supine with his hips flexed to 900 Physiotherapist in half kneeling supporting the legs. Ensure that the pelvis is in a neutral position Move the legs laterally to the sides using leg/arms Posterior and anterior pelvic tilt Child in supine with his hips flexed to 900 Physiotherapist in half kneeling supporting the legs. This evaluates the posterior pelvic tilt Lowe the legs to assess anterior tilt Lumbosacral rotation Child in supine with his hips flexed to 900 Physiotherapist in half kneeling supporting the legs. Do rotation to the left and right Test in controlled manner Be careful in the patient with already evident hyper-mobility of the lumbosacral joint Hip Abduction Child in supine If child has a severe lordosis bend the other leg up Do abduction of the hip Be careful avoid compensation by using ER Abduction may be restricted by severe adductor spasticity and shortening of the adductors Adduction Test the length of the TFL Supine If the left leg is being tested, lift the right hip and move it into adduction, this helps to stabilise the pelvis Now lift the left leg and move it into adduction Adduction might be restricted by tight m.gluteus medius Internal and external rotation Supine, leg bent with 900 hip and knee flexion Use the lower leg as a lever and do IR/ER hip Be care of excessive IR in cases where there already seems to be excessive ROM as this is an unstable position for the hip Can also be done in prone as above, just ensure that the rotation of the femur is neutral IR restricted by tight lateral rotators of the hip ie. mm. piriformis, quadratus femoris and obturator internus & externus ER restricted by tight gluteus minimus & medius, TFL Flexion Supine or side lying Hip flexion with knee flexion Can also test the length of m. hamstrings in supine. It is important to observe if the opposite legs pelvis/hip lifts Can be restricted by tight m. gluteus maximus Extension Side lying with the lower leg bent up in flexion 900 Ensure that the trunk is in a neutral position Stabilise at the pelvis and extend the hip Be careful of not getting lumbar extension Also guard against too much of a posterior pelvic tilt, adjust the degree of hip flexion of the lower leg Must differentiate whether m. quadriceps (with knee in flexion) or m. iliopsoas (with knee in extension) is restricting restricting Extension can be restricted by a tight m. iliopsoas or m. quadriceps over the hip Knee Knee flexion and extension Can be tested in sitting over end plinth or sitting on a block Extension can be limited by shortened m. hamstring Flexion of the knee can be limited by m. quadriceps Ankle Dorsiflexion and plantarflexion Can be tested in prone or in supine. Prone is often a more effective position to use especially in the case of severe extensor spasticity as this is a TIP Ensure that the foot is correctly aligned Grasp the heel to ensure that the DF movement actually takes place at the ankle and not the mid foot It important to test DF as well, especially in cases where the child constantly wears AFO’s DF restricted by a tight m. gastrognemius PF can be restricted by a tight m. tibialis anterior Foot Foot In supine evaluate rear foot mobility Also look at midfoot pronation and supination Also evaluate the length of the long toe flexors Look out for shortening of the plantar fascia Observe for foot abnormalities and biomechanical alignment issues References Kendall, F.P., Kendall McCreary and Provance, P.G. 1983. Muscle testing and function. 4ed. Williams & Wilkins. Baltimore Kriel, H. 2007. Cerebral Motor disturbances (lecture notes, UFS: unpublished) Smith, R. 2009. Paediatric Dictate (lecture notes, UFS: unpublished Images courtesy of Google images (2009)