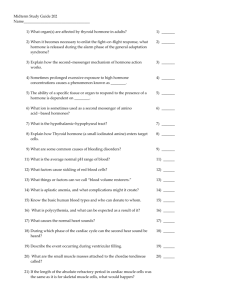
Medications Affecting the Endocrine System by Linda Self
advertisement

Endocrine glands Hormones—chemical messengers Water-soluble, protein derived hormones have short duration of action Lipid-soluble steroid and thyroid hormones have longer mechanism of action Endocrine and nervous systems interconnected Circadian cycles-ACTH, cortisol and GH Anterior pituitary hormones-GH, corticotropin, TSH, FSH, LH, prolactin Posterior pituitary hormones-ADH (vasopressin) and oxytocin Adrenal cortex hormones—cortisol and aldosterone Thyroid hormones—T3 (triiodothyronine) and T4 (thyroxine) Parathyroid hormone—PTH Ovarian hormones—estrogens and progesterone Testicular hormone—testosterone Placental hormones-chorionic gonadotropin, estrogen, progesterone, human placental lactogen Cholecystokinin Erythropoietin WBCs which produce cytokines Prostaglandins and leukotrienes Sometimes neoplasms Three mechanisms Inactivated by liver and kidney enzymes Sometimes conjugated by the liver and excreted in bile or urine Inactivated at receptor sites by enzymes Hypofunction-Type 1 diabetes, Addison’s Hyperfunction—Cushing’s, Grave’s, Gigantism Hypothalamus releases inhibitory and releasing hormones Corticotropin releasing hormone—released during sleep. Increased by vasopressin and decreased by somatostatin Growth-hormone releasing hormone— affected by dopamine, norepinephrine, epinephrine, GABA, acetylcholine and serotonin. Is blocked by somatostatin Somatostatin decreases the release of growth hormone, CCK, vasoactive intestinal peptide, TRH, others TRH causes release of TSH GRH (gonadotropin releasing hormone) causes release of FSH and LH Prolactin-releasing factor active during lactation Prolactin inhibitory factor active at times other than lactation Two act directly on target organs—growth hormone and prolactin Five act indirectly by stimulating target organs to produce hormones: Corticotropin –ACTH TSH FSH Luteinizing hormone—gonadotropin, maturation and rupture of ovarian follicle; produces corpus luteum; in men, affects Leydig’s cells and testosterone Melanocyte stimulating hormone Antidiuretic hormone—vasopressin, affects renal tubules to regulate water balance Oxytocin—uterine contractions and movement of milk from breast glands to nipples Equivalent to GnRH Zoladex (goserelin) Vantas (histrelin) Lupron (leuprolide) Synarel (nafarelin) Initially stimulate LH and FSH with chronic administration, inhibits stimulation Results in equivalent to castration in males and menopause in women Cannot be given orally Octreotide- Sandostatin; pharmacologically similar to somatostatin Use for acromegaly—reduces GH and insulin like growth factor Useful in vasoactive intestinal peptide tumors AIDS Cortrosyn (cosyntropin)—synthetic ACTH is used to test for adrenal insufficiency; IV or IM Humatrope (growth hormone)-for growth failure, Turner’s, renal failure growth retardation. Monitor ephiphyses. Chorex (HCG)-luteinizing hormone. In men to evaluate ability of Leydig’s (testosterone); Tx hypogonadism in pituitary problems and in cryptorchidism Ovidrel (HCG alpha) used w/ menotropins to induce ovulation Pergonal (menotropins)-contains FSH and LH; obtained from urine of menopausal women Somavert (pegvisomant)—GH receptor antagonist. Follistim (follitropin beta)—drug preparation of FSH used sequentially with HCG DDAVP (desmopressin) and Pitressin (vasopressin)—ADH; used in neurogenic DI, hemostasis in Von Willebrand’s Pitocin (oxytocin)-induction of labor, control postpartum bleeding Does not increase muscle mass or strength greater than seen with exercise alone Not indicated for anti-aging formula Adverse effects include—acromegaly, diabetes, hypertension, increased risk of cardiovascular disease, tumor growth and cancer Glucocorticoids or steroids Adrenal cortical secretion Corticotropin releasing hormone>>corticotropin>>>>cortisol With stress, increase in norepi, epi and cortisol; negative feedback system overruled Prototype is hydrocortisone Mineralocortocoid activity is intermediae in hydrocortisone, prednisolone and low in newer agents Increased glucose production Decreased cellular use of glucose 2ndary to decreased effect of insulin Increased breakdown of protein into amino acids Decreased rate of protein formation Increased breakdown of adipose tissue Decreaed inflammatory response by decreasing production of inflammatory chemicals, decreases numbers of antibodies, #s of lymphocytes Modifies vascular smooth muscle tone increasing pressor effects of catecholamines Stimulates renal glucocorticoid and mineralocorticoid receptors Can cause muscle atrophy Decrease bone formation, growth and increase bone breakdown Opens airways Stabilize mast cells Decrease viscosity of gastric mucous Class of steroids affecting fluid and electrolyte balance Conserve sodium and eliminate potassium Controlled by kidney function/Reninangiotensin system Inadequate secretion causes hyperkalemia, hyponatremia and ECF deficit Excessive secretion causes hypokalemia, hypernatremia and ECF excess Male = androgens Female = estrogens and progesterone Are secreted by both sexes Secondary sexual characteristics in men Affect libido and hair growth in women; excessive amounts can cause masculizing effects in women Addison’s Disease Secondary adrenocortical insufficiency Cushing’s disease Hyperaldosteronism Inhibits arachidonic acid metabolism thus affecting prostaglandins and leukotrienes Stabilizes biologic membranes also affecting prostaglandins and leukotrienes Inhibits production of interleukin 1, TNF and other cytokines Impairs phagocytosis—cells can’t move to injured site Impairs functioning of lymphocytes Inhibit growth of tissues thus delay wound healing Allergic or hypersensitivity disorders Collagen disorders-lupus, scleroderma and periarteritis Dermatologic Endocrine disorders Inflammatory bowel disorders Neoplastic disease—suppress lymphocytes Neurologic disorders-cerebral edema, myasthenia gravis Asthma and COPD Arthritis—if three or fewer joint, can give joint injections; no more than three per year Chemotherapy induced emesis—strong antiemetic effect, mechanism unknown. Usually give dose with serotonin antagonist and Reglan. Systemic fungal infections Hypersensitivity Those at risk for infections Diabetes mellitus (be cautious) Peptic ulcer disease Heart failure Renal insufficiency (can accumulate and cause s/s of hypercorticism) Beconase-beclamethasone nasally Nasonex (mometasone) Celestone-(betamethasone) orally Decadron (dexamethasone) po or IM Hydrocortisone—IV, IM, rectally Solu-Medrol (methylprednisolone)—po, IM, IV Kenalog(triamcinolone)—IM or topical Florinef (fludrocortisone)*****mineralocorticoid Daily administration of 15-20mg of hydrocortisone or its equivalent for 2 weeks suppresses the HPA axis MUST taper down Thyroid produces three hormones: thyroxine, triidothyronine and calcitonin T3 more potent but with a shorter duration of action Production of thyroid hormones is dependent on iodine and tyrosine (needed to form thyroglobulin) Control rate of cellular metabolism, linear growth, brain function, dentition, bone development and neural development Inhibition of pituitary release of TSH Increassesd fat metabolism Increased carbohydrate metabolism Increased heart rate, force of contraction and cardiac output Increase rate of cellular metabolism and oxygen consumption Common causes include: Hashimoto’s thyroiditis, secondary to treatment for hyperthyroidism Treatment with amiodarone, lithium or iodine preparations Congenital—cretinism Myxedema –can progress to coma Bruising Decreased cardiac output Decreased heart rate Cardiomegaly ASHD Apathy, lethargy Forgetfulness Drowsiness Cold intolerance Constipation Fatigue Puffiness Increased susceptibility to infections Increased sensitivity to narcotics, barbiturates, anesthetics Excessive production of thyroid hormone Associated with Graves Disease, nodular goiter, thyroiditis, overtreatment with thyroid drugs, pituitary adenoma or thyroid cancer Subclinical=reduced TSH but normal T3/T4 Can result in osteoporosis Thyroid storm aka thyrotoxicosis Have been reported cases of iodine-induced hyperthyroidism Tachycardia Increased cardiac output Increased BP Dysrhythmias Heart failure Nervousness, restlessness, insomnia Heat intolerance Weight loss Diarrhea Weakness Tremors Amenorrhea Increased susceptibility to infection exophthalmos Prototype and drug of choice is Synthroid, Levothroid (levothyroxine) Maximum absorption if taken on empty stomach Is T4 TSH (0.5 to 4.2 microunits/L) desired level Goal is euthyroid with TSH level Most drugs given will have prolonged effect Lifelong therapy is indicated Thioamide derivatives-- Propylthiouracil and methimazole. Used before radioactive iodine therapy Results may not be apparent for 3 months or longer Thioamide preparation to achieve euthyroid state Then Iodine preparations—Lugol’s and SSKI Iodine preparations may be used to reduce size and vascularity of thyroid before surgery Can cause: goiter, hyperthyroidism, benefits are temporary Radioactive iodine cannot be used effectively for prolonged time in those who have received iodine preparations (insufficient uptake thereafter) OK TO GIVE THIOAMIDE THEN IODINE PREPARATION BUT NOT IODINE THEN THIOAMIDE Thyroid disorders change metabolism of other drugs Children w/congenital hypothyroidism, tx should be started within 6 weeks of birth Drug of choice is levothyroxine Monitor ht. and wt. If hyperthyroid, can use PTU or methimazole, discourage radioactive iodine in children s/s of thyroid disorders may mimic other disorders in older adults Thorough PE and diagnostic workup Levothyroxine is appropriate Start with small doses, may increase in small increments monthly Monitor vitals closely For hyperthyroidism, use PTU or methimazole. May use radioactive iodine. Thyrotoxicosis manage in intensive care