Continued Use of Illicit Substances: A Retention
advertisement
Oral Substitution Treatment for Opioid
Dependence: A Training in Best Practices &
Program Design for Nepal
Day 1
March 26-28, 2006
Kathmandu, Nepal
UNDP
Richard Elovich, MPH
Columbia
University Mailman School of Public
Health Medical Sociologist
Consultant, International Harm Reduction
Development International Open Society Institute
1
This Training is Adapted From:
Medication-Assisted Treatment For Opioid
Addiction in Opioid Treatment Programs
CSAT/SAMSHA (Substance Abuse and Mental Health Services
Administration Center for Substance Abuse Treatment)
2
Best Practices in Methadone Maintenance Treatment
Office of Canada’s Drug Strategy
Addiction Treatment: A Strengths Perspective
Katherine van Wormer and Diane Rae Davis
Additional Sources: Robert Newman, MD, Alex Wodak,
MD, Melinda Campopiano, M.D, Miller and Rollnick,
Prochaska, DiClemente, and Norcross, Michael Smith,
MD, Sharon Stancliff, MD, Ernest Drucker, PhD,
Adequate
Resources
Program Development
And
Design
Accessibility
3
A
Maintenance
Orientation
Training Goals
Ideally, this training will contribute to:
4
Increased knowledge, skills and best
practices among OST practitioners and
providers;
Engagement and retention of clients/patients
in the OST program in Kathmandu
Improved treatment outcomes
Six Training Modules
5
The SocioPharmacology of Opioid
Use and Dependence
Introduction and
background of oral
substitution treatment
The pharmacology of
medications used in oral
substitution treatment
Information collection
and service provision:
‘assessment-in-action’
Pharmacotherapy and
OST
Insights from the field
Learning Together
Parallel Process
6
Learning Process: Knowledge and
Skills
Acquisition of content
Retention (store in memory)
Application (retrieve and use)
Proficiency (integrate and synthesize)
7
Expectations for Certification:
Training Contract
8
This is an 18 hour
training over a 3 day
period. Allowances have
been made for your work
schedules: Noon – 6 PM.
You must be present and
participate in all 18 hours
of the training to receive
certification. There can
be no exceptions.
Please stay focused. Be
on task because we have
a lot of material to cover
in 3 days.
Listening is a key to this
training. Listen to new ideas.
Listen to what’s coming up
inside you in relation to what’s
being presented. Try to put
your thoughts and feelings into
words instead of “shutting
down.”
Acknowledge and respect
differences. You can “agree to
disagree” on a contentious
point and move on. Participate
in role plays. Everyone has
permission to pass. Offer
feedback constructively not
personally. Try to receive
feedback as a gift.
Learning Environment
9
Try to be okay with
taking some learning
risks. Stretch past
your edge of what
you know and what
you are comfortable
with.
Confidentiality. Hold
the container. Don’t
be leaky.
Turn
off
phones
please.
No cross talk. Allow one
person to speak at a
time. Equal time over
time.
Start and end on time,
including breaks.
Be
alert to tendency to fudge
this.
Use “I” statements.
Can everybody agree to
this training contract? Is
there
anything
you
absolutely cannot live
with?
Now we are off.
I. The Socio-Pharmacology of
Opioid Use and Dependence
10
Heroin/Tidigesic/’Set’ Use= Social
Heroin/opiate use, though physiological and
experienced in the body, is socially mediated.
What does this mean?
11
Initiation– relational, social
Learning to use the drug.
Administration
The experience changes over time
Managing the experience
Contingencies
What else?
The production of getting “off” or
getting “high”.
12
Brainstorm components of the production.
List names of the social actors involved in the
production.
Identify social interactions.
Identify cognitive and learning processes.
Identify strategies of the heroin user or addict.
What is Opioid dependence?
13
14
“Drug Use is The Root of Their
Problems”
15
Substance use may be an expression of a
problem rather than its cause.
Rather than the cause of erratic or unhealthy
behavior, substance use may be an adaptive
mechanism or best solution to a range of
problems including mental illness, abusive
partner, homelessness, sexual abuse, poverty
or other difficulties (Springer, 1991)
“Bad Drug Using Women”
16
A survey of crack-using women in New York, for
example, found that nearly 1/3 had a past
history of abuse and prior hospitalization for
mental illness (Chavkin, 1993).
In another, women who were HIV+, were
homeless in the last year, and had experienced
combined physical and sexual abuse were also
those most likely to report exchanging sex for
drugs and money, using injection drugs in the
past year, and having sex in crack houses (El
Bassel et al, 2001).
“An Addict Stays the Same or
Gets Worse.”
17
Addiction is cyclic and variable in intensity.
While some addicts may follow the
pattern, made familiar by alcoholism, of
chronic, progressive illness, others may
have periods of intense drug use and
dysfunction followed by long periods of
being drug free or vice versa (Kane,
1999).
Compare cocaine bingeing and heroin
“It’s Their Choice; it’s Their Own
Fault.”
18
Ongoing substance use is rarely a simple
question of choice.
Much as with people in abusive
relationships or those with compulsive
disorders, “choice” for substance users is
shaped by perceptions of self-efficacy,
mental health status, and social
conditions.
“They stopped growing. They are not
themselves. They are addicted.”
19
How do we know they stop growing?
Who defines when people are themselves?
How do we define these terms? Societal or
cultural norms?
How does the “planet heroin” story lead us to
the disappearance of the person into the drug?
How are heroin users accounts of themselves
ignored or marginalized when we make these
assumptions based on the label addict?
“They are manipulative. They lie.”
20
Once a person is labeled a heroin addict,
what assumptions do we make about
them?
How are they treated by health providers?
Imagine yourself at your last job interview.
“Whose Fault is it Anyway?”
21
Addiction– like hypertension, asthma, or
diabetes– is chronic, relapsing condition whose
etiology frequently includes a combination of
behavioral, genetic, and environmental factors.
As with substance users, only a minority of
diabetics or hypertensives successfully abstain
from the behaviors contributive to these
conditions, yet these patients are not
stigmatized, blamed for their condition, or
denied health services (McLellelan et al, 1995)
1. How Do Drugs Work?
Drug Action: Interconnection between
neurology, the science of the nervous system,
and chemistry
Drug Effects represents broader phenomena
than drug and living tissue association.
Drug Factors, which originate outside the
laboratory, in real life practice that shapes
effects.
22
Drug Action I
23
In passing through the brain, a given drug (the
“key”) will be attracted to, and will bind to a
specific site in the brain (the lock).
The sites in the brain that control certain organs
are rich in receptors into which specific drugs
“fit” much like a key into a lock; these same sites
may lack receptors for other drugs.
Drug Action II
24
For instance, after heroin turns into
morphine in the body, morphine “fits into”
the receptors in the brain that control
breathing and heartbeat rate, and hence,
a sufficiently large dose of this drug can
shut down these two functions and cause
death by overdose.
Opiates: Duration of action
25
Methadone
Oxycontin
Heroin
Dilaudid
Codeine
Demerol
Fentanyl
24 hours
12 hours
6-8 hours
4-6 hours
3-4 hours
2-4 hours
1-2 hours
Heroin In The Brain
26
Short-term Effects Of Heroin Use
27
Soon after injection (or inhalation), heroin
crosses the blood-brain barrier.
In the brain, heroin is converted to
morphine and binds rapidly to opioid
receptors.
Abusers typically report feeling a surge of
pleasurable sensation, a "rush."
Short-term Effects Of Heroin Use
28
The intensity of the rush is a function of how
much drug is taken and how rapidly the
drug enters the brain and binds to the
natural opioid receptors.
Heroin is particularly addictive because it
enters the brain so rapidly.
Short-term Effects Of Heroin Use
With heroin, the rush is usually accompanied
by
The rush may also be accompanied by
29
A warm flushing of the skin,
Dry mouth, and
A heavy feeling in the extremities,
Nausea,
Vomiting, and
Severe itching.
Short-term Effects Of Heroin Use
30
After initial effects, drowsy for several hours.
Mental function clouded by effect on CNS.
Cardiac function slows.
Breathing severely slowed, sometimes to
the point of death.
Overdose is a particular risk on the street,
where the amount and purity of the drug
cannot be accurately known.
Short-term Effects Of Heroin Use
31
“Rush”
Depressed Respiration
Clouded Mental Functioning
Nausea and Vomiting
Suppression of pain
Spontaneous abortion
Heroin Intoxication
32
Pupil size (pinned pupils)
Voice (slower, lower in tone)
Conversations (talkative)
Being high (feeling warm, euphoric, content)
Scratching
Droopy eyes
Itchiness?
Blood spots (needle marks bleed)
Expansive mood
Nodding out (sleep-like state)
Drug Action and Drug Effects
33
It is crucial to make a distinction between
the specific pharmacological action of a
drug, which is the product of a biological
and chemical process, and drug effects.
Drug Effects
34
Drug effects is far more than the chemistry of a
drug placed in the setting of living tissue. They
represent the nonspecific factors that influence
drug effects.
Six more or less pharmacological dimensions:
(1) identity and half-life in the body; (2) dose; (3)
potency and purity; (4) drug mixing; (5) route of
administration; (6) habituation.
Five additional factors that originate outside
the laboratory setting in real life practice
35
Set
Setting
Script
Schedule (раскумарчтвся or morning shot)
Structure
Tolerance
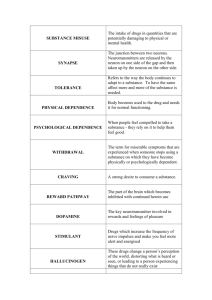
Need for increased amounts of
the drug to achieve desired effect
Markedly diminished effect with
continued use of the same
amount of the drug
Withdrawal
36
Characteristic withdrawal
syndrome
The same (or closely related) drug
is taken to relieve or avoid
withdrawal symptoms
The drug is taken in larger
amounts or over a longer period
than was intended
There is a persistent desire or
unsuccessful efforts to cut down
or control drug use
A great deal of time is spent in
activities necessary to obtain the
drug
Important social, occupational or
recreational activities are given up
or reduced
Drug use is continued despite
knowledge of having a persistent
or recurrent problem that is likely
to have been caused or
exacerbated by the drug use
What is Substance Dependence
37
As the DSM IV explains, the term “addiction” is no longer
widespread in the medical community, and has been
widely replaced by the term “drug {or substance}
dependence. They also note that the term “drug {or
substance abuse} abuse” is:
“a highly complex, value-laden and often excessively
vague term that does not lend itself completely to any
single definition.”
Furthermore, because the term has different meanings
for different groups of people– and their definition of the
term reflects their different perspectives– there is often
difficulty in drawing a line between use of substances
and abuse of substances (Brands et al., 1998, 45).
Dependence Syndrome
38
Dependence syndrome consists of the particular
behavioral, cognitive and physiological effects that may
arise through repeated substance use.
Psychological characteristics include a strong desire
to take the drug (craving), impaired control over its use,
persistent use despite harmful consequences, and the
prioritization of drug use over other activities and
obligations.
Physical dependence comprises increased tolerance
and a physical withdrawal reaction that occurs when
drug use is discontinued (WHO 1984)
The DSM-IV* Specifies Criteria
for Opioid Dependence:
“A maladaptive pattern of substance use, leading to
clinically significant impairment or distress, as
manifested by three (or more) of the following,
occurring any time in the same 12-month period:
tolerance, as defined by either of the following:
a)
b)
A need for markedly increased amounts of the substance to
achieve intoxication or desired effect
Markedly diminished effect with continued use of the same
amount of the substance.
*American Psychiatric Association’s Diagnostic and Statistical Manual
of Mental Disorder (DSM-IV)
39
The DSM-IV Specifies Criteria for
Opioid Dependence:
Withdrawal, as manifested by either of the
following:
a)
b)
40
The characteristic withdrawal syndrome for the
substance
The same (or a closely related) substance is taken
to relieve or avoid withdrawal symptoms
The substance is often taken in larger amounts
or over a longer period than was intended
There is a persistent desire or unsuccessful
efforts to cut down or control substance use
The DSM-IV Specifies Criteria for
Opioid Dependence:
41
A great deal of time is spent in activities
necessary to obtain the substance, use the
substance, or recover from its effects
Important social, occupational, or recreational
activities are given up or reduced because of
substance use
The substance use is continued despite
knowledge of having a persistent or recurrent
physical or psychological problem that is likely
to have been caused or exacerbated by the
substance
Perspectives on Drug
Dependence
42
The unfolding nature of heroin
dependence
Different types of dependencies and
patterns of practices. Drug dependence is
complex and variable but literature speaks
in absolutes
Fluid phenomenon: movable famine
Drug users are thinking, strategizing
Range of different therapies/services for
multiple and incremental outcomes
Tolerance and Habituation
43
When a person uses heroin regularly, they
develop a tolerance– they have to use more
heroin to get the same effects. The greater the
amount and frequency of their use, the faster
they become tolerant.
Some people try to “chip” or use only
occasionally, avoiding two days in a row.
Others try to “manage their habits” by using a
little less for a day or two to lower their
tolerance, allowing them to decrease the
amount needed to get high-- or well.
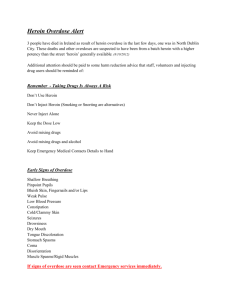
Overdose
44
Overdose is a serious health risk for
heroin users.
Heroin slows down the heart rate and
breathing; someone who overdoses may
eventually stop breathing altogether.
Mixing heroin with other drugs (valium,
alcohol, cocaine) significantly increases
risk of overdosing, especially alcohol.
Active Drug users can be
approached about overdosing:
45
Avoid mixing heroin with other drugs,
especially “benzos” (Xanax, Clonopin,
Ativan, Valium), other “downs” (Seconal,
Elavil, Placidyl) or alcohol.
Many drug users overdose after coming
out of jail because their tolerance has
fallen. Users should do a tester shot if it is
from a new source or they have not used
in a while.
Overdose are very serious but do
not have to be fatal:
46
Drug users should talk with using partners and
make a plan for dealing with ODs. If they have
thought it through, they are less likely to panic or
freeze up in the event of an actual OD.
Drug users should know about Naloxone, what
paramedics use, and can call 1 866 STOP ODS
for more information.
Drug users can learn rescue (mouth to mouth)
breathing, which is the most important thing they
can do to help someone survive an overdose.
Heroin Withdrawal (1 of 2)
47
Elevated Blood Pressure & Pulse
Insomnia (can last for days or weeks)
Restlessness
Anxiety (confusion, exaggerated startle reflex)
Irritability
Body aches
Lacrimation
Sneezing
Heroin Withdrawal (2 of 2)
48
Runny nose
Piloerection (body hair stands up)
Nausea and vomiting (can lead to dehydration)
Sweating
Diarrhea
Deep muscle twitch
Spontaneous erection or ejaculation (due to
hypersensitivity)
Pupil dilation (enlarged pupils)
Long-term Effects Of Heroin Use
49
Dependence
Infectious Diseases: HIV/AIDS, Hepatitis B & C
Collapsed veins
Bacterial Infections
Abscesses
Infection of heart lining and valves
Arthritis and other rheumatologic problems
Long-term Effects Of Heroin Use
Physical dependence develops with higher
doses of the drug.
50
The body adapts to the presence of the drug
and withdrawal symptoms occur if use is
reduced abruptly.
Withdrawal may occur within a few hours after
the last time the drug is taken.
Long-term Effects Of Heroin Use
Symptoms of withdrawal include:
51
Restlessness
Muscle and bone pain
Insomnia
Diarrhea
Vomiting
Cold flashes with goose bumps ("cold turkey")
Leg movements.
Long-term Effects Of Heroin Use
52
Major withdrawal symptoms peak 24 - 48
hours after the last dose of heroin and
subside after about a week.
Some people have shown persistent
withdrawal signs for many months.
Heroin withdrawal is never fatal to otherwise
healthy adults, but it can cause death to the
fetus of a pregnant addict.
Chronic Use: Medical
Complications
53
Scarred and/or collapsed veins
Bacterial infections of blood vessels and heart
valves
Abscesses (boils) and other soft-tissue infections
Liver or kidney disease
Lung complications (e.g., pneumonia, TB) may
result from the poor health condition of the abuser
as well as from heroin's depressing effects on
respiration.
Sources of Skin Infections
54
User’s skin and mouth (most common)
Syringe
Cooker
Dissolving water
Filter
Drugs and contaminants
Danger Signs
Fever and chills
Increased pulse
Difficulty breathing
Altered mental status/confusion
Can progress to
55
Sepsis
Necrotizing fascitis (gangrene, streptococcus)
Wound botulism or tetanus
Prevention of Infection
56
New needle for each injection or reduction
in reuse
Site rotation
Alcohol wipes or soap and water for at
least one minute
Cook heroin until it bubbles
Plan for missing the vein
Chronic Use: Medical
Complications
57
Clogging of blood vessels that lead to the
lungs, liver, kidneys, or brain (due to the
many additives in street heroin which may
not readily dissolve) resulting in infection or
even death of small patches of cells in vital
organs.
Immune reactions to these or other
contaminants can cause arthritis or other
rheumatologic problems.
Chronic Use: Medical
Complications
58
Sharing “works” or fluids can lead to some of
the most severe consequences of heroin
abuse-infections with hepatitis B and C, HIV,
and a host of other blood-borne viruses,
which drug abusers can then pass on to their
sexual partners and children.
Heroin Abuse & Pregnancy
59
Heroin abuse can cause serious
complications during pregnancy,
including miscarriage and
premature delivery.
Children born to addicted
mothers are at greater risk of
SIDS (Sudden Infant Death
Syndrome), as well.
Heroin Abuse & Pregnancy
60
Pregnant women should not be detoxified from opiates
because of the increased risk of spontaneous abortion or
premature delivery; rather, treatment with methadone is
strongly advised.
Infants born to mothers taking prescribed methadone may
show signs of physical dependence but they can be treated
easily and safely in the nursery.
Research has demonstrated also that the effects of in utero
exposure to methadone are relatively benign.
Heroin Use & Blood-borne Diseases
61
At risk for contracting HIV, hepatitis C, and other
infectious diseases through sharing and reusing
syringes and injection paraphernalia that have
been used by infected individuals.
They may also become infected with HIV and,
although less often, to hepatitis C through
unprotected sexual contact with an infected person.
Injection drug use has been a factor in an
estimated one-third of all HIV and more than half of
all hepatitis C cases in the Nation.
Heroin Use & Blood-borne Diseases
Users can change the behaviors that put them at
risk for contracting HIV, through drug abuse
treatment, prevention, and community-based
outreach programs, including harm reduction.
Users can reduce or eliminate the risk of exposure
to HIV/AIDS and other infectious diseases by
decreasing/eliminating:
62
drug use
Injection drug use
drug-related risk behaviors such as needle sharing
unsafe sexual practices
II. Introduction and background of
oral substitution treatment
63
What is Oral Substitution Therapy (OST)?
How does Methadone Work?
Rationale for and Uses of OST
What types of OST are Most Effective?
Increasing Access to OST in Nepal:
Identifying and Overcoming Barriers
Developing a Continuum of MMT Program
Delivery
Vernacular Formulations of
Substitution Therapies
64
Irregular supply, fluctuations in price and
purity mean dangers for drug users and
others
Drug users are already creating their own
forms of replacement therapy
Although we call it ‘methadone
maintenance,’ it is a form of drug
treatment
65
66
67
68
69
70
The Basic Orientation
71
THE PATIENT: like all other patients
THE CONDITION: like all other chronic medical
conditions
THE MEDICATION: like all others used in medicine
CHINA VISIT
APRIL 7-14, 2005
The Baron Edmond de Rothschild
Chemical Dependency Institute
72
73
74
75
76
77
78
79
80
81
What is Methadone?
Formulation: Oral solution, liquid
concentrate, tablet/diskette, and powder
Receptor Pharmacology: Full mu, opioid
agonist
Regulation: Proscriptive regulations fail to
leave room for treatment flexibility and
innovation (SAMSHA, U.S. Department of Health and Human
Services: Treatment Improvement Protocol 43: 22)
82
How Does Methadone Work? 1
83
Opiate agonists bind to the mu opiate
receptors on the surfaces of brain cells,
which mediate the analgesic and other
effects of opioids.
Methadone produces a range of mu
agonist effects similar to those of shortacting opioids.
How Does Methadone Work? 2
84
Therapeutically appropriate doses of this agonist
medication produce cross-tolerance for short
acting opioids such as morphine and heroin,
thereby suppressing withdrawal symptoms and
opioid craving as a short-acting opioid is
eliminated from the body. The dose needed to
produce cross-tolerance depends on the
individual patient’s level of tolerance for shortacting opioids.
How Does Methadone Work? 3
85
When given intramuscularly or orally,
methadone suppresses pain for 4 to 6
hours. Intramuscular is used only for
patients who cannot take oral methadone,
for example, patients in medicationassisted treatment for opioid dependence
who are admitted to a hospital for
emergency medical procedures.
How Does Methadone Work? 4
86
Methadone is metabolized chiefly by the
cytochrome P3A4 (CYP3A4) enzyme
system (Oda and Kharasch 2001), which
is significant when methadone is coadministered with other medication that
also operate along this metabolic pathway.
How Does Methadone Work? 5
87
After patient induction into methadone
pharmacotherapy, a steady-state
concentration (i.e., the level at which the
amount of drug entering the body equals
the amount being excreted) of methadone
usually is achieved in 5 to 7.5 days (four to
five half-lives of the drug).
How Does Methadone Work? 6
88
Methadone’s pharmacological profile
supports sustained activity at the mu
opiate receptors, which allows substantial
normalization of many physiological
disturbances resulting from the repeated
cycles of intoxication and withdrawal
associated with dependence on shortacting opioids.
How Does Methadone Work? 7
89
Therapeutically appropriate doses of methadone
also attenuate or block the euphoric of heroin
and other opioids.
When opiate medication dosage must be
adjusted to compensate for the effects of
interacting drugs (e.g., Rifampin for TB),
observe patients for signs or symptoms of opioid
withdrawal or sedation to determine whether
they are under medicated or overmedicated.
How Does Methadone Work? 8
90
Methadone is up to 80% orally
bioavailable, and its elimination half-life
ranges from 24 to 36 hours. When
methadone is administered daily in steady
oral doses, its level in blood should
maintain a 24-hour asymptomatic state,
without episodes of overmedication or
withdrawal (Payte and Zweben 1998).
How Does Methadone Work? 9
91
Methadone’s body clearance rate varies
considerably between individuals. The serum
methadone level (SML) and elimination half-life
are influenced by several factors including
pregnancy and a patient’s absorption,
metabolism and protein binding, changes in
urinary pH, use of other medications, diet,
physical conditions, age, and use of vitamin and
herbal products (Payte and Zweben 1998).
Early Research Findings Vincent P. Dole
1980, 1988
Patients do not experience euphoric,
tranquilizing, or analgesic effects. Their
affect and consciousness were normal.
Therefore, they could socialize and work
normally without the incapacitating effects
of short-acting opioids such as morphine
or heroin
(SAMSHA, U.S. Department of Health and Human Services: Treatment
Improvement Protocol 43: 17-18)
92
Early Research Findings Vincent P. Dole
1980, 1988
A therapeutic, appropriate dose of
methadone reduced or blocked the
euphoric and tranquilizing effects of all
opioid drugs examined, regardless of
whether a patient injected or smoked the
drugs (e.g., morphine, heroin, opium, etc.)
(SAMSHA, U.S. Department of Health and Human Services: Treatment
Improvement Protocol 43: 17-18)
93
Early Research Findings Vincent P. Dole
1980, 1988
No change usually occurred in tolerance levels
for methadone over time, unlike for morphine
and other opioids; therefore, a dose could be
held constant for extended periods (more than
20 years in some cases.)
Methadone was effective when administered
orally. Because it has a half-life of 24-36 hours,
patients could take it once a day without a
syringe. (SAMSHA, U.S. Department of Health and Human Services:
Treatment Improvement Protocol 43: 17-18)
94
Early Research Findings Vincent P. Dole
1980, 1988
Methadone relieved the opioid craving or hunger
that patients with addiction described as a major
factor in relapse and continued illegal use
Methadone, like most-opioid class drugs,
caused what were considered minimal side
effects, and research indicated that methadone
was medically safe and nontoxic.
(SAMSHA, U.S. Department of Health and Human Services: Treatment Improvement
Protocol 43: 22)
95
Expansion of Methadone from
Research to Public Health Program
96
Most patients were stabilized on methadone
doses of 80 to 120 mg/day.
Most patients who remained in treatment
subsequently eliminated illicit-opioid use.
In general, the team found that patients’ social
functioning improved with time in treatment, as
measured by elimination of illicit-opioid use and
better outcomes in employment, school
attendance, and domestic relations.
Columbia University School of Public Health, Dr. Frances Rowe Gearing, 1974
Poly Substance Use and Abuse
97
However, 20 percent of more of these patients
also had entered treatment with alcohol and poly
substance abuse problems., despite intake
screening that attempted to eliminate these
patients from treatment. (Gearing and Schweitzer 1974)
Methadone treatment was continued for these
patients, along with attempts to treat their
alcoholism and polysubstance abuse.
MMTP Becomes A Major Public
Health Initiative in the U.S.
98
Methadone maintenance became a major public
health initiative to treat opioid dependence
under the leadership of Dr. Jerome Jaffe, who
headed the special Action Office for Drug Abuse
Prevention in the Executive Office of the White
House in the early 1970s.
Dr. Jaffe’s office oversaw the creation of a
nationwide , publicly funded system of treatment
programs for opioid dependence
The pharmacotherapy of opiate
dependence
Robert Newman, MD,
Director, Baron Edmond de Rothschild Chemical Dependency Institute
Beth Israel Medical Center, NYC
Presented @ the 15th INTERNATIONAL CONFERENCE
ON THE REDUCTION OF DRUG RELATED HARM,
Melbourne, Australia, 20-24 April, 2004
99
The Baron Edmond de Rothschild
Chemical Dependency Institute
Methadone Maintenance (MMT).
Dole and Nyswander, 1964
Their goal: “… to look for some
medication to permit addicts to live as
normally as possible” *
Initial study ** with 22 “subjects”
“Maintenance dose” ranged from 10180mg
No reference to any preferred duration of
treatment
100
Methadone: seeking to explain success
Dole and Nyswander, 1967
“The unexpected response to a
simple medical program forced us to
re-examine our assumptions”
“We had been misled by traditional
theories based on weaknesses of
character.”
101
Addiction: A theory
Dole, 1970
“Persistent physiological changes
contribute – somehow! – to relapse
tendency after abstinence has been
achieved.”
102
Dole. Ann. Rev. Biochem. 30:821-840, 1970
1973 - support for the theory:
Opiate receptors/peptides in brain
“Identification of opiate receptors
provides insight into mechanism of
action of opiates.” *
Brain “contains substances with
morphine-like activity”**
103
“High on methadone?” No!
“We have not been able to find a medical or
psychological test capable of identifying patients
on methadone.”*
When given placebo “patients were unaware that
the medication had been changed” until
withdrawal began**
“Methadone given in constant daily doses causes
no euphoria, abstinence symptoms or demand for
escalation of dose.”**
* Dole and Nyswander. JAMA. 193(8):646-650, 1965
** Dole and Nyswander. NY State J of Med. 66(15):2011-2017,
1966
104
Methadone effectiveness and safety
US Government assessment, 1983
Retains more patients, longer, than any other
treatment
Heroin use and criminal activity significantly reduced
Employment increases
Marked improvement in health status
No major adverse consequences
Dosage/duration limits “therapeutically unjustified”
US National Institute on Drug Abuse DHHS publication
(ADM)83:1281, 1983
105
US Government on Methadone –
consistency! 1983-2004
1997: “Methadone significantly lowers illicit
opiate use and related illness and death,
reduces crime, enhances social
responsibility.”*
2004: “Methadone continues to be a safe
and effective treatment for addiction to
heroin.”**
* NIDA Notes, 1997,
http://www.drugabuse.gov/NIDA_Notes/NNVol12/NIPanel.html
** Subst. Abuse and Ment. Heath Services Admin., News release
6 Feb 2004
106
United Nations on harm reduction
and methadone, 2003
“UNODC is particularly committed to programmes
that reduce harm from drug abuse.”
“It is important to implement methadone
programmes urgently.”
Speech by Dr. Sandro Calvani, UNODC Regional Representative for East Asia
and the Pacific, given in Hong Kong 22 Oct. 2003
107
WHO/UNODC/UNAIDS
Position paper on “substitution”, 2004
“Maintenance treatment is an
effective, safe, cost-effective
modality.”
Available on line: http://www.who.int/substance_abuse/
108
When there’s commitment . . .
Hong Kong, 1975-76
End 1974:
one “pilot” programme, 500
patients
End 1975: approximately 2,000 enrolled
End 1976: approximately 10,000 enrolled
Admissions to voluntary in-patient drugfree programmes stable 1974-76: 2,3002,500/year
109
Newman J. Pub. Health Policy 6(4):526-538 (1985)
Roughly: For a
problem with heroin,
call this number for
same-day help!
110
Risk of HIV Infection in Hong Kong
(1984-2002)
160
140
120
100
80
60
40
20
Heterosexual
Homosexual/bisexual
Injecting Drug Use
20
02
20
01
20
00
19
99
19
98
19
97
19
96
19
95
19
94
19
93
19
92
19
91
19
90
19
89
19
88
19
87
19
86
19
85
19
84
0
Other/Unknown
Source: HIV Surveillance Report 2002 Update (Dept of Health, Hong Kong S.A.R., Nov 2003)
111
When there’s commitment . . .
Croatia 1991-present
Treatment started 1991; GPs mainstay of
MMT
Of 2,400 GPs nationally, over 1,000
provide MMT
High retention – 70-80%
Estimated 15,000 heroin addicts; 7,000
get Rx
112
Ivancic SEEA Addiction 4(1-2):15-17, 2003
Estimated number of patients receiving
methadone & buprenorphine in France, 1996-2001
Source: on web at http://www.drogues.gouv.fr/fr/professionnels/etdues_recherches/IT-4b.pdf
113
Ancient history
Dr. Ernest Bishop (NYC), 1920
“We have regarded failure to abstain from
narcotics as evidence of weak will-power.”
“We have prayed over our addicts, cajoled
them, exhorted them, imprisoned them,
treated them as insane and made them
social outcasts” – and we’ve consistently
failed!
114
Bishop, The Narcotic Drug Problem. Macmillan; NY 1920
Stepped Approach vs. All or Nothing
Approach
115
Optimal: drug cessation
Reduce drug use
Increased control of drug use
Alternative to injecting
Alternative to sharing
Reduce harm related to sharing and safer
sex practices
The Context for OST in Nepal
Heroin
Tidigesic (Buprenorphine)
The “Set”:
116
Norphine
Diazapam
Avil
The Subjective Meanings of Injecting