File
advertisement

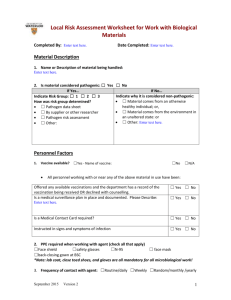
Basics of Biosafety Working Safely with Biological Materials What is Biosafety? Principles and practices employed to protect laboratory personnel and the environment from exposure or infection while working with living organisms, biological materials, or agents. Included are any materials that may be potentially infectious. Includes recombinant DNA research Hierarchy of Controls The Hierarchy of Controls is the preferred method of controlling preventing and controlling hazards. You must document that you went through this process. Administrative Control: Rotating workers more often to reduce exposure times Engineering Control: Installing guards on machinery, ventilation, sound proofing Safe Work Practices: policies and procedures increasing safety either by changing the actual way the work is done or by adding a tool to help Personal Protective Clothing or Equipment: respirators, ear plugs permissible exposure limit Administrative Controls Authorization/Approval Written biosafety procedures required for the experimental procedures and equipment including inventory of biological agents or materials Laboratory personnel biosafety training Medical Surveillance (BSL 2 and above) Health history Medical screening Immunization Serum storage Post-exposure prophylaxis Engineering Controls Biological safety cabinets, glove boxes Animal containment caging systems Safety equipment (filtered or sealed equipment) Ventilation system Containment facilities Personal Protective Clothing and Equipment Provides barrier against skin, mucous membrane or respiratory exposure to infectious agents during procedures Prevent spread of contamination Integrity wanes with use (i.e., change gloves frequently) Biosafety Levels (BSL) BSL are used in risk management BSL are ways to control the agent facilities, safety equipment, practices, PPE, etc. Once risk is assessed then the appropriate BSL is determined BioSafety Level 1 Well characterized, non-pathogenic organisms or agents Open bench- no containment Use good laboratory practices, waste disposal, and aseptic techniques (i.e. performed under sterile conditions) Example: E. coli K-12 strains BSL 1: Work Practices and Procedures Applications Non-infectious agent and tissue culture, media preparation Prevent Cross Contamination Keep cultures covered Flame instruments and containers Use sterile media and equipment Keep hands or face away from cultures BSL 1: Work Practices and Procedures Biosafety Procedures Work with agents may be conducted on open bench Wash hands often No mouth pipetting No eating or drinking in lab Minimize aerosol generation Decontaminate work surfaces Wear applicable PPE BioSafety Level 2 Agents of moderate hazard to personnel or environment Basic lab, but restricted access, containment during certain processes (i.e. aerosols, large volumes, etc.) Autoclave and Biological Safety Cabinet desired Use good laboratory practices, waste disposal, and aseptic techniques Example: most non-respiratory, non lethal, agents BSL 2: Work Practices and Procedures Increasing emphasis on safety procedures and practices Increasing need for staff training Increasing need for competent supervision Biohazard sign posted at entry door Biohazard labels affixed on regulated waste containers Use of personal protective equipment as a barrier to exposure: lab coat, gloves, eye and face protection Some work on open bench allowed BSL 2: Work Practices and Procedures Aerosol generating procedures performed in a biosafety cabinet: Homogenizing Vortexing Vigorous mixing Pipetting infectious liquids Sonication Pouring If breach occurs: Evacuate lab, post spill sign With appropriate PPE and disinfectant, decontaminate centrifuge, buckets, other items or areas BioSafety Level 3 Agents of high hazard to personnel or environment Respiratory exotic or indigenous agents which are easily transmissible causing serious or lethal disease All work is contained, engineering controls and controlled environments Example: Mycobacterium tuberculosis, SARS, etc. BioSafety Level 4 FORGET ABOUT IT!!! Hemorrhagic fever, deadly viruses, etc. Total containment, airtight labs, “submarine” doors, air pumps, water treatment, etc. Positive pressure “moonsuits” Exposure Controls Careful Pipetting Techniques Never blow out last drop in pipette Use pipetting aids with filters Never mix by suction and expulsion (mix by sonication) Discharge liquid down side of container, using tip-to-wall contact Deliver as close as possible to contents Work over plastic-backed absorbent matting (ensure it doesn’t slide forward or backward blocking air grill) Exposure Controls Use Extreme Care with Sharps Use sharps if only absolutely required as part of a process Percutaneous exposure risk Employ safe work practices Utilize safe sharp devices Aerosol exposure risk Use biosafety cabinet for removal of air from needle Use mechanical methods for needle removal Never bend, recap or manipulate sharps by hand Keep hands away from needle Exposure Controls Safe Work Practices Wash hands after each glove use and immediately or ASAP after exposure. Remove PPE before leaving work area. Flush body parts with water after contact with blood or OPIM OPIM = Other Potentially Infectious Material Exposure Controls Safe Work Practices Clean-up of spills and broken glassware/sharps contaminated with blood or OPIM • Wear protective eyewear and mask if splashing is anticipated • Remove glass and other sharps materials using a brush and dust pan, forceps, etc. Do not use your hands • Properly discard all materials into a sharps or puncture-resistant biohazardous waste container • Use paper/absorbent towels to soak up the spilled materials Exposure Controls Personal Protective Equipment (PPE) • Gloves - Latex - Nitrile - Vinyl - Utility Nitrile and vinyl gloves Exposure Controls Personal Protective Equipment (PPE) • Protective clothing - Lab coat - Gown - Apron - Shoe cover or boot Exposure Controls Personal Protective Equipment (PPE) • Eye-Face Protection and Masks - Safety glasses with side shields - Splash goggles - Face shield - Mask Biohazardous/Medical Waste Waste that is potentially infectious to humans, animals or plants Biohazard Labels and Signs: • Must have biohazard symbol • Labels attached securely to any containers Biohazardous /Medical waste Predominantly Lettering and symbol fluorescent orange in contrasting color or orange/red to background background Biohazardous Waste Categories Cultures and stocks of infectious agents and associated biologicals laboratory waste biological production waste discarded live and attenuated vaccines culture dishes and related materials contaminated PPE Biohazardous Waste Categories Liquid human and animal waste liquid or semi-liquid blood and blood products and body fluids contaminated items that would release blood or items that are caked with blood or other potentially infectious materials; NOT including urine or materials stained with blood or body fluids infectious animal waste (research) Biohazardous Waste Categories Pathological waste tissues body parts other than teeth products of conception fluids removed by trauma or during surgery or autopsy/necropsy or other medical procedure and not chemically fixed. …And More Biohazardous Waste Categories Animal and plant pathogen waste Recombinant DNA waste Sharps Managing Liquid Biohazardous Waste Storage: Label and secure bulk vessels if not disposed of immediately Treatment: Chemical disinfection OR Autoclave Disposal: THEN Flush to sewer Use proper PPE! Managing Non-Sharp Biohazardous Waste labeled container lined with a biohazardous waste bag equipped with a lid. Managing Non-Sharp Biohazardous Waste Securely tie bags for transport to treatment/collection site. When moving wastes, use secondary containment; avoid using public halls and elevators. “Breakable” Non-sharps Biowaste Store in labeled containers that are puncture-resistant, closable and will capture leakage, BUT…. …Do NOT use SHARPS containers! #3 Is it a sharps hazard? Examples: – – – – needles syringes Scalpels مشرط all biologically contaminated objects that can easily penetrate skin (Pasteur pipettes, razor blades, etc.) Place sharps in approved sharps container for disposal! …Syringes in research settings should be disposed of as a sharp to avoid public relations concerns! Sharps Containers Containers must be leak-proof, puncture-resistant, closable & labeled with the biohazard symbol. Proper sharps containers must be used for both clinic and field work. Proper Use of Sharps Containers Place tops on containers before use on lab bench Don’t forget to date the container when first put into use Remember: sharps containers are a one-way disposal system Proper Use of Sharps Containers Use sharps containers for sharps ONLY! • No solid biohazardous waste (i.e. gauze, un-broken pipettes, gloves) • No mercury thermometers What’s wrong with this picture? Sharps Container Disposal Containers must be permanently closed and disposed: Within 90 days of first use When ¾ full Disposal methods: Landfill مكب Incineration We الحرق use waste hauler متعهد للنفايات Safety Notes on Sharps Use Do not re-cap sharps Keep sharps container in close proximity to point of use (i.e. limit handling) for easy disposal Do not leave needles in pockets of coveralls or smocks Managing All That Other Waste… Do NOT discard medications in the trash. Return to source for disposal or seek assistance. Recordkeeping Medical Records • • • • • • For employees with exposure Confidential Hepatitis B vaccination status Post-exposure evaluations HCP’s written opinions Information provided to HCP as required HCP = Health Care Property Investors Recordkeeping Training Records • Dates • Content summary • Trainer name & qualifications • Attendee’s names & job titles