File
advertisement

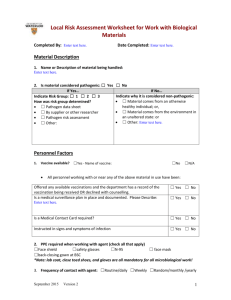
UNIT 5 Biosafety What is Biosafety? Principles and practices employed to protect laboratory personnel and the environment from exposure or infection while working with living organisms, biological materials, or agents. - Included are any materials that may be potentially infectious. - Includes recombinant DNA research Agents and Risks The “agent” is the what creates risk. Risks to the worker or environment are often unknown. Determining “acceptable risk”? Assessing Risk There is always risk! The risk must be identified The risk is evaluated The risk must be measured Plan to minimize the risk Who Determines Acceptable Risk? Assessment is conducted by a Biosafety Professional in partnership with and based on information provided by the Principal Investigator The assessment is presented to the Institutional Biosafety Committee (IBC) for approval Identifying Risk Understand the biology of the agent 1 Susceptibility and transmission within the host Hazards associated with equipment and procedures Goal: Provide the highest practical protection and the lowest practical exposure WHO-World Health Organization Agents Assigned Risk Groups RG-1 Unlikely to cause disease in humans or animals low individual or community risk RG-2 May cause disease but typically not serious individual risk, low community risk, treatable RG-3 May cause serious disease, usually treatable High individual but low community risk, serious respiratory agents RG-4 Serious or fatal, often not treatable, Easy transmission, high individual and community risk Biosafety Levels (BSL) Different than the Risk Groups!! Risk groups used in risk assessment BSL are used in risk management BSL are ways to control the agent facilities, safety equipment, practices, PPE, etc. Once risk is assessed then the appropriate BSL is determined BioSafety Level 1 Well characterized, non-pathogenic organisms or agents 2 Open bench- no containment Use good laboratory practices, waste disposal, and aseptic techniques Example: E. coli K-12 strains BioSafety Level 2 Agents of moderate hazard to personnel or environment Basic lab, but restricted access, containment during certain processes (i.e. aerosols, large volumes, etc.) Autoclave and Biological Safety Cabinet desired Use good laboratory practices, waste disposal, and aseptic techniques Example: most non-respiratory, non lethal, agents BioSafety Level 3 Agents of high hazard to personnel or environment Respiratory exotic or indigenous agents which are easily transmissible causing serious or lethal disease All work is contained, engineering controls and controlled environments we currently do not have the facilities to handle. Example: Mycobacterium tuberculosis, SARS, etc. BioSafety Level 4 FORGET ABOUT IT!!! Hemorrhagic fever, deadly viruses, etc. Total containment, airtight labs, “submarine” doors, air pumps, water treatment, HEPA filtration, etc. Positive pressure “moonsuits” Laboratory Acquired Infections (LAI) 3 Bacterial: 76% from clinical labs 8% from research labs Exposure: 60% acquired from inhalation Other exposures include: digestion, sharps, splashes, direct and indirect contact Viral 16% from clinical labs 70% from research labs 32% from animal related activities Biohazardous/Medical Waste Waste that is potentially infectious to humans, animals or plants. It includes: Medical Waste according to MMWRA Regulated Waste by MIOSHA Regulated Waste by CDC/NIH Biohazardous Waste Management Plan Must outline how generating facility complies with the MMWRA: Types of wastes generated 4 Storage and disposal of wastes Contingency plans Training Biohazardous Waste Categories Cultures and stocks of infectious agents and associated biologicals laboratory waste biological production waste discarded live and attenuated vaccines culture dishes and related materials contaminated PPE Biohazardous Waste Categories Liquid human and animal waste liquid or semi-liquid blood and blood products and body fluids contaminated items that would release blood or items that are caked with blood or other potentially infectious materials; NOT including urine or materials stained with blood or body fluids infectious animal waste (research) Biohazardous Waste Categories Pathological waste tissues 5 body parts other than teeth products of conception fluids removed by trauma or during surgery or autopsy/necropsy or other medical procedure and not chemically fixed Animal and plant pathogen waste Recombinant DNA waste Sharps Managing Liquid Biohazardous Waste Storage: Label and secure bulk vessels if not disposed of immediately Treatment: Chemical disinfection OR Autoclave Disinfection 10% bleach solution good for general disinfection High organics use 20% Needs to be made weekly Test contact time Ethanol Use 70% solution (most effective) Longer contact time and flammable *Should research and know effectiveness and contact time for the best disinfectant against your agent! 6 Managing Non-Sharp Biohazardous Waste labeled container lined with a biohazardous waste bag equipped with a lid. Managing Non-Sharp Biohazardous Waste Securely tie bags for transport to treatment/collection site. When moving wastes, use secondary containment; avoid using public halls and elevators. Breakable” Non-sharps Biowaste Store in labeled containers that are puncture-resistant, closable and will capture leakage Effective Waste Autoclaving Leave bag open during autoclaving or loosely closed Add water to bag prior to autoclaving if primarily dry materials Steam must contact materials Place bag in autoclavable tray with sides Treated Waste Bag Disposal Allow waste bag to cool Use fume hood to reduce odors Securely tie bag shut Place bag in a non-transparent black bag for regular disposal Is it a sharps hazard 7 Examples: – – needles – syringes – scalpels – all biologically contaminated objects that can easily penetrate skin (Pasteur pipettes, razor blades, etc.) Place sharps in approved sharps container for disposal! Sharps Containers Containers must be leak-proof, puncture-resistant, closable & labeled with the biohazard symbol. Proper sharps containers must be used for both clinic and field work. Proper Use of Sharps Containers Place tops on containers before use on lab bench Don’t forget to date the container when first put into use Remember: sharps containers are a one-way disposal system Proper Use of Sharps Containers Use sharps containers for sharps ONLY! • No solid biohazardous waste (i.e. gauze, un-broken pipettes, gloves) 8 • No mercury thermometers Sharps Container Disposal Containers must be permanently closed and disposed of through the animal facility manager: Within 90 days of first use When ¾ full Disposal methods: Landfill Incineration We use waste hauler 9