Organ Transplantation
advertisement

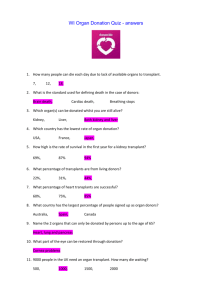
Majid Sajeel University of Gujrat Objectives Provide a history of transplantation Review organs that are transplantable Define types of transplants Issues related to recipients Overview of immunosuppression Issues related to donors Other considerations The History of Organ Transplant Prehistoric transplantation exists in mythological tales of chimeric beings 1903-1905: Modern transplantation began with the work of Alexis Carrel who refined vascular anastomoses as well as transplanted organs within animals 1914-1918: Skin grafting in WWI 1952: Dr. Hume at Peter Bent Bringham Hospital in Boston attempted allograft kidney from unrelated donor 1954: Dr. Joseph E. Murray transplanted kidney from Ronald Herrick to his identical twin, Richard Herrick, to allow him to survive another 8 years despite his ESRD 1956: First successful BMT by Dr. Donnall Thomas, the recipient twin received whole body radiation prior to transplant Continued… 1957: Azathioprine deveoped by Drs. Hitchings and Elion 1966: First successful pancreas transplant by Kelly and Lillehei 1967: First successful heart transplant by Christiaan Barnard in South Africa, That same yr., first successful liver transplant performed by Thomas Starzl 1981: First successful heart/lung transplant by Dr. Reitz at Standford 1983: First successful lung transplant by Dr. Joel Cooper; cyclosporin approved 1984: Congress passed the National Organ Transplant Act (NOTA 1999: pancreatic islet cell transplant by Dr. Shapiro 2008: face transplant Transplantable Organs/Tissues Liver Kidney Pancreas Heart Lung Intestine Face Bone Marrow Cornea Blood Types of Transplant Heterotopic organ added or Orthotopic organ replaced Autograft same being Isograft/Syngenetic graft identical twins Allograft/homograft same species Xenograft/heterograft between species Statistics On Waitlist as of 1/9/09 Transplanted in 2007 All organs 7282 All organs 2662 Kidney 5827 Kidney 1498 Liver 743 Liver 610 Pancreas 106 Pancreas 86 Kid/Panc 182 Kid/Panc 115 Heart 211 Heart 174 Lung 200 Lung 144 Heart/Lung 1 Heart/Lung 5 Intestine 12 Intestine 30 Transplant Regions Organs are first offered to patients within the area in which they were donated* before being offered to other parts of the country in order to: reduce organ preservation time improve organ quality and survival outcomes reduce costs incurred by the transplant patient increase access to transplantation *With the exception of perfectly matched donor kidneys. Pre-Transplantation Evaluation Blood Type (A, B, AB, and O) Rh factor does not matter Human Leukocyte Antigen (HLA); antigens on WBC Crossmatch; if positive, then cannot receive organ; done multiple times up to 48 hrs prior to transplant Serology; for HIV, CMV, hepatitis Cardiopulmonary, cancer screening Types of donor Organ donors may be living brain dead Brain dead means the donor must have received an injury (either traumatic or pathological) to the part of the brain that controls heartbeat and breathing In "living donors", the donor remains alive and donates a renewable tissue, cell, or fluid Reasons for donation and ethical issues Living related donors: donate to family members or friends in whom they have an emotional investment. The risk of surgery is offset by the psychological benefit of not losing someone related to them, or not seeing them suffer the ill effects of waiting on a list. Good Samaritan Good Samaritan or "altruistic" donation A donation to someone not well-known to the donor Choice: out of a need to donate Some donate to the next person on the list others use some method of choosing a criteria important to them Web sites are being developed that facilitate such donation Compensated donation Donors get money or other compensation in exchange for their organs Common in some parts of the world Whether legal or not Is one of the many factors driving medical tourism In Pakistan 40 percent to 50 percent of the residents of some villages have only one kidney They have sold the other for a transplant into a wealthy person Probably from another country Said Dr. Farhat Moazam of Pakistan, at a “World Health Organization” conference Pakistani donors are offered $2,500 for a kidney but receive only about half of that because middlemen take so much Tools Used to Stratify Transplant Recipients MELD/PELD= model for end stage liver disease and pediatric end stage liver disease MELD developed in 2002 to account for objective findings rather than subjective findings; range is 6-40 MELD:>12y.o Creatnine, Bilirubin, and INRinternational normalized ratio for prothrombin time PELD:<12 y.o. Alb, Bili, INR, growth failure and age Tools Used to Stratify Transplant Recipients CPRA=calculated Panel Reactive Antibody Used in allocation of kidney, pancreas Developed in 2004 Measure of antibody sensitization; reflects % of donors not compatible with candidate secondary to candidate’s unacceptable antigens POOLED HLA (100 DONORS) Panel Reactive Antibodies (PRA) Determination of Brain Death Defined formally in 1968 by ad Hoc committee at Harvard headed by Beecher Defined by government in Office of the President with Uniform Determination of Death Act in 1981 Individual who has sustained either 1. irreversible cessation of circulatory or respiratory functions or 2. irreversible cessation of all functions of the entire brain, including brainstem, is dead. A determination of death must be made in accordance with accepted medical standards. Diagnosis of Brain Death Pt suffered irreversible loss of brain function (either cerebral hemisphere or brainstem) Establish cause that accounts for loss of function Exclude reversible etiology: Intoxication }- perform tox screen NM blockade Shock Hypothermia (<90 deg F)warming blanket When Etiology Determined and NOT Reversible LACK OF CEREBRAL FUNCTION ___________________ Deep coma No response to painful stimuli **Can have spinal cord reflexes LACK OF BRAINSTEM FUNCTION ___________________ ____ Pupillary reflexes Corneal reflexes Occulocephalic reflexes Occulovestibular reflexes Gag reflex Cough reflex Key Elements in the Process of Donation after Cardiac Death Withdrawal of life sustaining measures Pronouncement of death from time of onset of asystole (usually btwn 2-5 minutes) To avoid conflicts of interest transplantation team physicians are not a member of the end-of-life care or declaration of death Liver within 30 min and kidney within 60 min If time to asystole exceeds 5 min, then recovery of organs is canceled Drawbacks to Transplantation after Cardiac Death Healthcare workers may be uncomfortable recommending withdrawal of care for one pt to obtain organ for a second Interval between withdrawal of care and death may be shortened and family relationship may be altered Conflict of interest Use of heart in cardiac transplantation References 1. 2. 3. 4. http://www3.niaid.nih.gov/topics/transplant/hist ory http://www.unos.org http://www.organdonor.gov http://en.wikipedia.org/wiki/Organ_transplantati on